CHAPTER 5
Rapid Alveolar Expansion of Osteoperiosteal Flaps
An ideal is a blueprint for failure.
—Theo Mestrum
The use of alveolar sagittal split osteotomy to augment posterior alveolar width is reserved for the deficient alveolar ridge that has adequate height but inadequate width for dental implants.1–7 The narrowest transalveolar dimension that can be technically split is 2.5 to 3.0 mm.1 Ridges that are 3.5 to 5.0 mm wide1 can be split with sharp osteotomes,1,8 whereas 2.5- to 3.0-mm ridges are best split with piezoelectric surgery. 9,10 However, the desired minimal facial bone thickness next to an implant is 2.0 mm.11,12
A number of procedures have been used following alveolar split osteotomy, including intra-alveolar bone grafting13 and implant placement with or without bone grafting.14,15 These procedures have utilized full mucoperiosteal flaps or a partial-thickness flap dissection technique.
A third flap approach to crest split expansion of alveolar bone is the minimal reflection access of the osteoperiosteal flap. This bone flap, commonly called the book flap, is used when bone grafting is done.1 This same osteoperiosteal flap can also be manipulated without bone grafting in an alveolar width distraction procedure.16–21 In this procedure, a bone-spreading device is placed directly into the alveolar split osteotomy site to initiate alveolar width distraction immediately after the alveolar split osteotomy. The advantages of a width distraction procedure include the relatively brief operating time, reduced patient morbidity, significantly reduced healing time, and superior quality of bone formed compared to that formed after interpositional grafting.22 The book flap sometimes can be used with simultaneous implant placement, whereas width distraction requires a delayed implant placement protocol.19,21
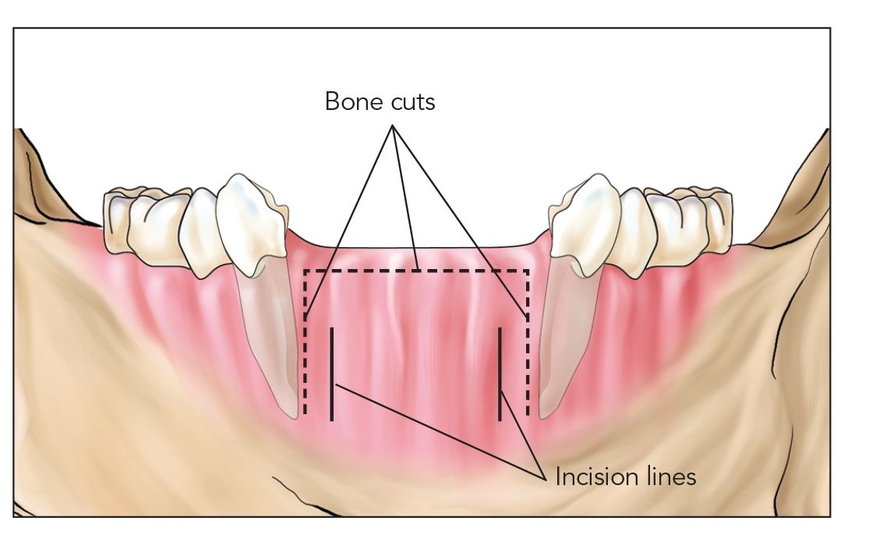
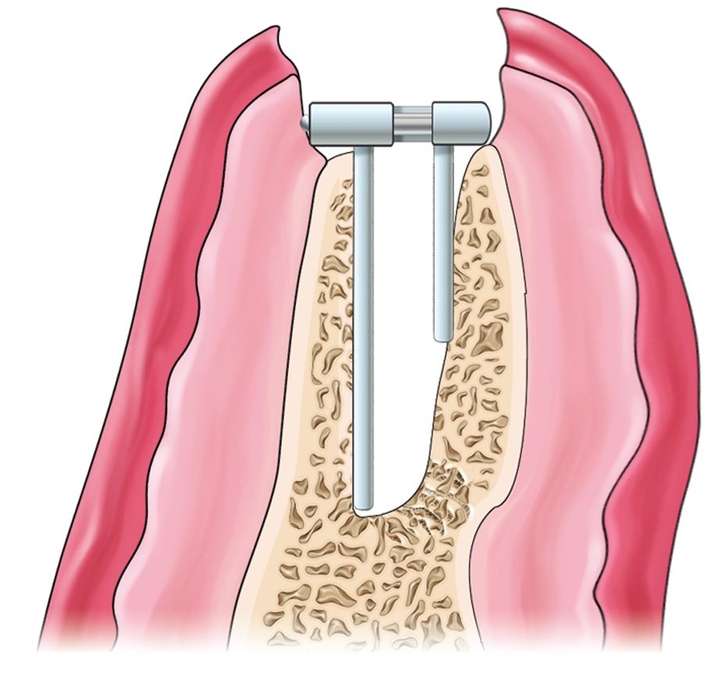
Fig 5-1a The alveolar crest widener is able to widen the alveolus 5 to 6 mm as long as the crest is of adequate height near the alveolar plane.
Still another variation of buccal plate manipulation presented in this chapter is a procedure called rapid alveolar expansion. This technique creates space for an implant immediately and without outfracturing the buccal plate bone while using the controlled leverage of a bone spreader. After posterior alveolar sagittal split osteotomy, the intervening device is used to expand lingual and facial bony walls, which heal endosteally without bone graft. In some instances, recombinant human bone morphogenetic protein 2 (rhBMP-2) is applied in the gap. After a gap of up to 4 mm is created at the time of surgery, the device holds the site open until a callus is formed; healing is by secondary intention, analogous to the healing in dental extraction sockets.17,20
 Surgical Technique
Surgical Technique
The alveolus, usually a posterior segment in either arch, is approached through a minimally reflected crestal incision for placement of an alveolar crest expander (Figs 5-1a and 5-1b). An osteotomy is performed; piezoelectric surgery is usually required because of the narrowness of the alveolus. Vertical limiting cuts are made to limit the anterior-posterior dimension of the split. The bone-spreading device (Crest Expander, Surgi-Tec) is malleted in place to a depth of 10 mm (Figs 5-1c to 5-1e). The alveolus is automatically widened by about 2 mm at this point.
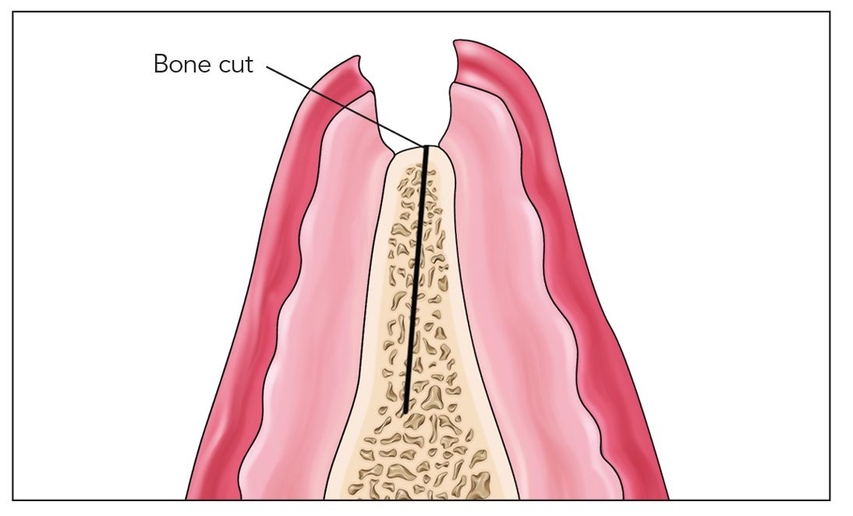
Fig 5-1b The unreflected incision allows access with a piezoelectric knife. It is not always necessary to connect the incisions, which helps to prevent dislodgment of the mucoperiosteum.
With activation of the device, the segment will bend, without fracturing, to widen the gap. In the mandible, expansion of 3 or 4 mm is achievable; in the maxilla, expansion of 5 or 6 mm is possible. If the site is overexpanded, the buccal (or lingual) plate may fracture free and become flaccid, converting the site into an i-flap that requires bone grafting (see chapter 7). Following completion of bone spreading, the device is secured to an adjacent tooth and left in place without grafting for 4 to 6 weeks (Figs 5-1f and 5-1g).
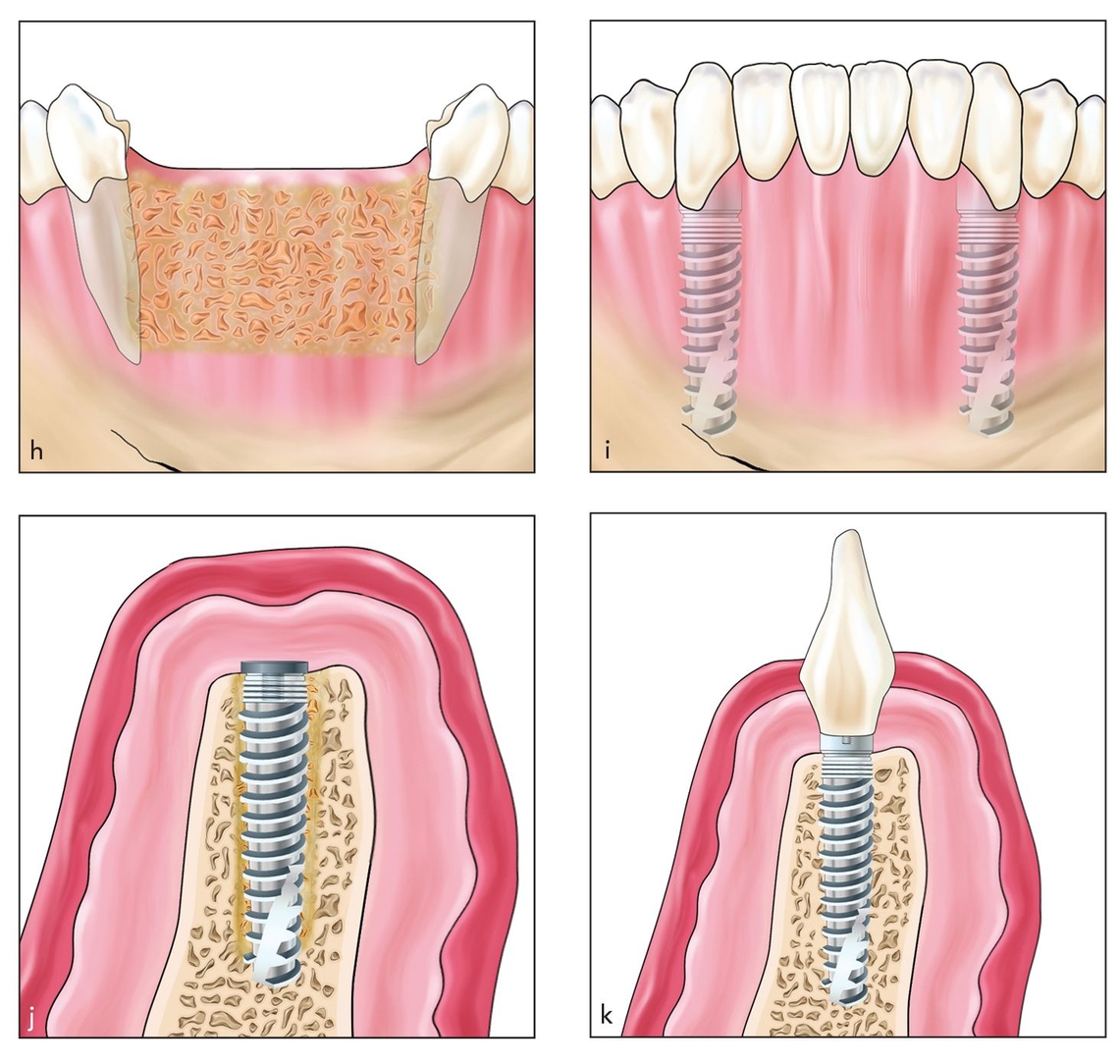
After callus formation (5 to 6 weeks), the device is removed and implants are placed transgingivally through osteoid into basal bone, where primary fixation must be achieved. The implant should be submerged for 3 months before being exposed for final restoration (Figs 5-1h to 5-1k).
When the exposed gap is wide, such as 5 mm or wider, or the bone walls appear avascular, a collagen carrier should be used to place rhBMP-2 interpositionally.23 Implant placement in this setting is delayed for 4 months. However, in certain settings, the device can be removed on the same day as activation, and implants can be placed immediately after the alveolar split and expansion procedure. When implants are placed simultaneously, the maximum width desirable is about 3 mm, and one implant is placed to hold the gap prior to removal of the bone spreader.
Figs 5-1c and 5-1d Following osteotomies (dotted line), the segment can be split just enough to insert the distraction device. Only a few sutures are placed to close the tissue around the device.
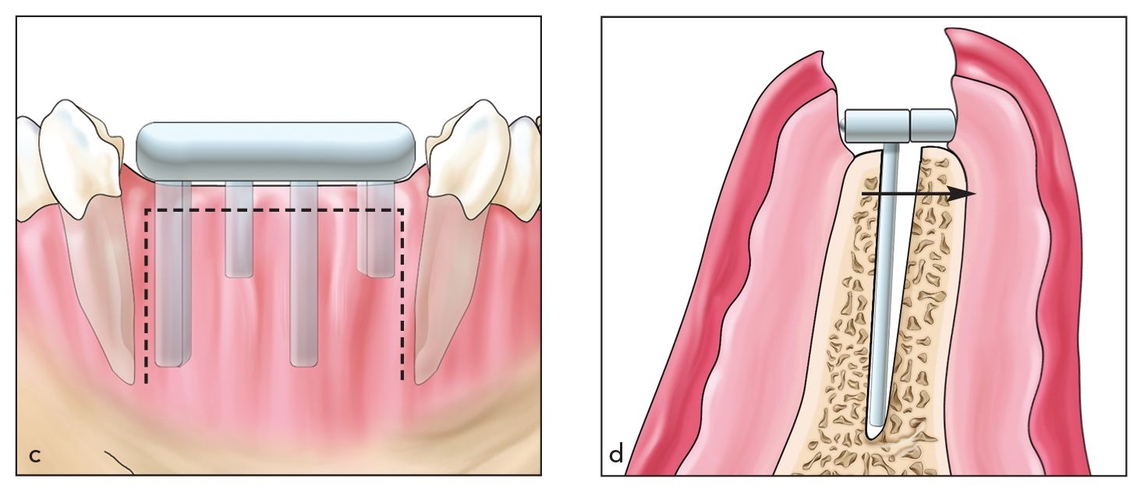
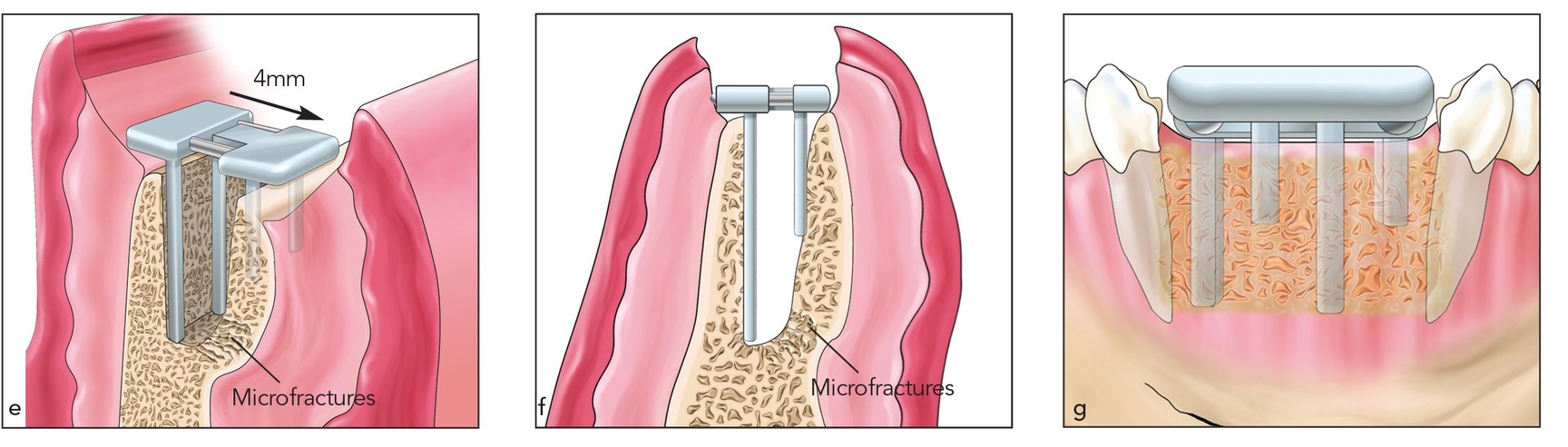
Figs 5-1e to 5-1g When the device is in place and the tissue is coapted to the device, it is immediately activated, widening the segment an additional 1 to 2 mm for a total of 3 to 4 mm. The device is left to heal without grafting for 4 to 6 weeks.
Figs 5-1h to 5-1k After the device is removed, implants can be placed the same day or a few weeks later as long as apical fixation can be obtained. Following osseointegration, the restoration is completed.
Case 1: Mandibular rapid alveolar expansion without rhBMP-2
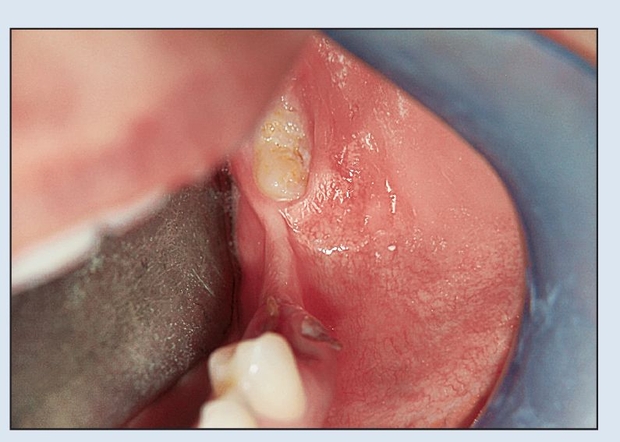
Fig 5-2a The patient has a narrow posterior alveolus with sufficient height.
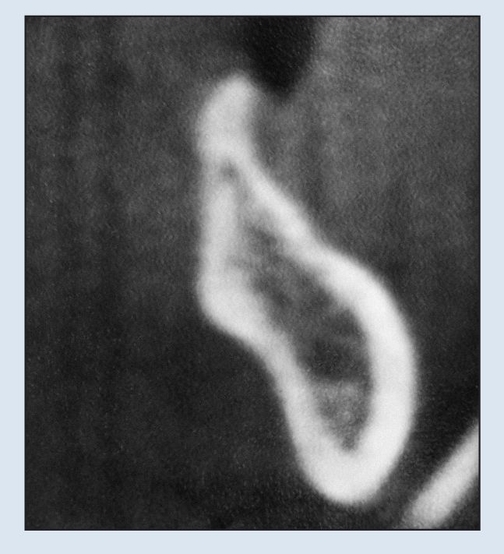
Fig 5-2b The computed tomography (CT) scan reveals a 2- to 3-mm-wide alveolus.

Fig 5-2c The preoperative panoramic radiograph reveals that the alveolus is level with the alveolar ridge.
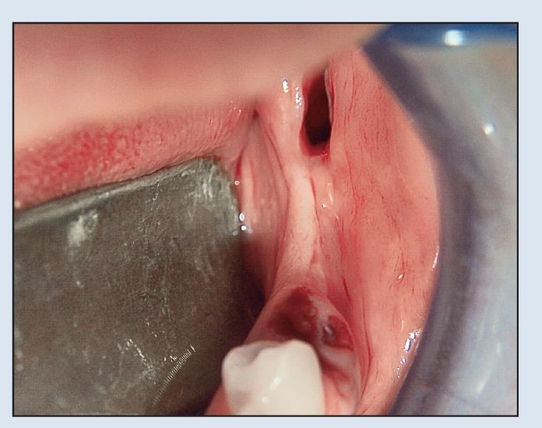
Fig 5-2d Flapless dental extractions are performed.
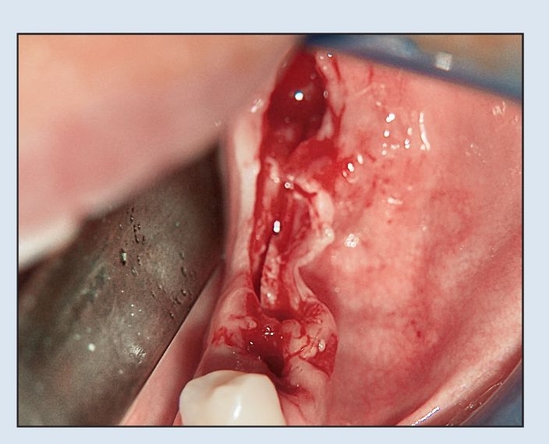
Fig 5-2e A flap is minimally reflected, just exposing the crest to provide access to a piezoelectric knife. The ridge is then split to a depth of 10 mm.
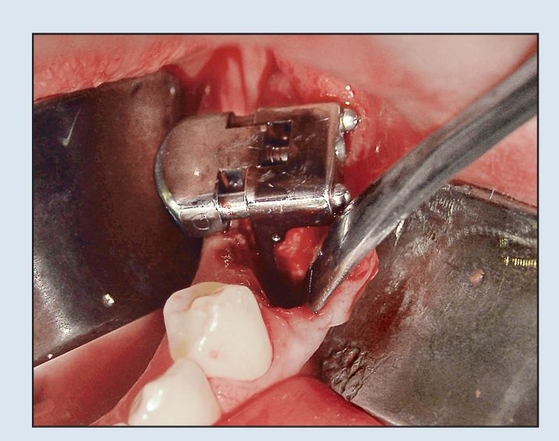
Fig 5-2f After a vertical cut is made 2 mm behind the adjacent tooth to preserve subpapillary bone, the bone spreader is tapped in place, automatically spreading the alveolus 2 mm.
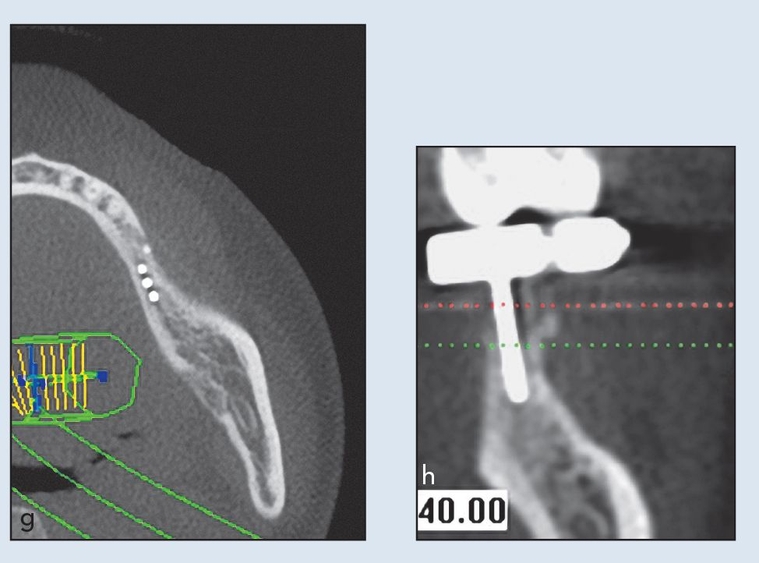
Figs 5-2g and 5-2h The device was activated carefully to prevent fracture of the lingual or buccal plate. A postplacement CT scan confirms device placement and plate integrity.
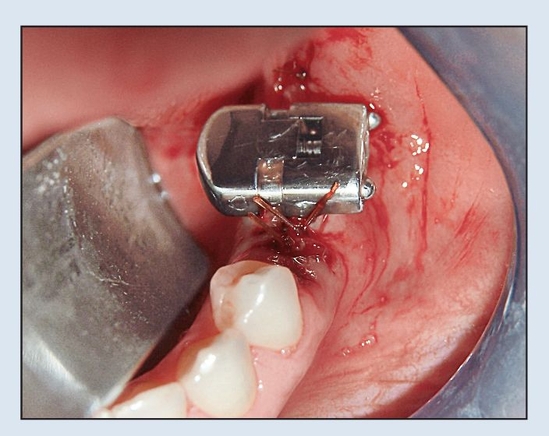
Fig 5-2i The wound is closed primarily with chromic gut suture.

Fig 5-2j Implants are placed 6 weeks after expansion.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


