Treatment of Aggressive and Atypical Forms of Periodontitis
The majority of patients with common forms of periodontal disease respond predictably well to conventional therapy, including oral hygiene instruction, nonsurgical debridement, surgery, and supportive periodontal maintenance. However, patients diagnosed with aggressive and some atypical forms of periodontal disease often do not respond as predictably or as favorably to conventional therapy. Fortunately, only a small percentage of patients with periodontal disease are diagnosed with aggressive periodontitis. Patients who are diagnosed with periodontal disease (any type) that is refractory to treatment present in small numbers as well. Even fewer patients are diagnosed with necrotizing ulcerative periodontitis. Each of these atypical disease entities poses significant challenges for the clinician not only because they are infrequently encountered, but also because they may not respond favorably to conventional periodontal therapy.24,40 Furthermore, the severe loss of periodontal support associated with these cases leaves the clinician faced with uncertainty about treatment outcomes and difficulty in making decisions about whether to save compromised teeth or to extract them.
Aggressive Periodontitis
Aggressive periodontitis, by definition, causes rapid destruction of the periodontal attachment apparatus and the supporting alveolar bone (see Chapter 25). The responsiveness of aggressive periodontitis to conventional periodontal treatment is unpredictable, and the overall prognosis for these patients is poorer than for patients with chronic periodontitis. Because these patients do not respond “normally” to conventional methods and their disease progresses unusually fast, the logical question is whether there are problems associated with an impaired host immune response that may contribute to such a different disease and result in a limited response to the usual therapeutic measures. Indeed, defects in polymorphonuclear leukocyte (PMN, neutrophil) function have been identified in some patients with aggressive periodontitis.30,31 Also, in a small number of cases, a systemic disease, such as neutropenia, can be identified that clearly explains the unusual severity of the periodontal disease for that individual.12,13 In most patients with aggressive periodontitis, however, systemic diseases or disorders cannot be identified. In fact, the irony is that these patients are typically quite healthy. Numerous attempts to examine immunologic profiles in patients with aggressive periodontitis have failed to identify any specific etiologic factors common to all patients.
The prognosis for patients with aggressive periodontitis depends on (1) whether the disease is generalized or localized, (2) the degree of destruction present at the time of diagnosis, and (3) the ability to control future progression. Generalized aggressive periodontitis rarely undergoes spontaneous remission, whereas localized forms of the disease have been known to arrest spontaneously.29 This unexplained curtailment of disease progression has sometimes been referred to as a “burnout” of the disease. It appears that cases of localized aggressive periodontitis often have a limited period of rapid periodontal attachment and alveolar bone loss, followed by a slower, more chronic phase of disease progression. Overall, patients with generalized aggressive periodontitis tend to have a poorer prognosis because they typically have more teeth affected by the disease and because the disease is less likely to go spontaneously into remission compared with patients with localized forms of aggressive periodontitis.
Therapeutic Modalities
Treatment of aggressive periodontitis must be pursued with a logical and regimented approach. Several aspects of treatment must be particularly considered when managing a patient with aggressive periodontitis. One of the most important aspects of treatment success is to educate the patient about the disease, including the causes and the risk factors for disease, and to stress the importance of the patient’s role in the success of treatment.1 Essential therapeutic considerations for the clinician are to control the infection, arrest disease progression, correct anatomic defects, replace missing teeth, and ultimately help the patient maintain periodontal health with frequent periodontal maintenance care. Educating family members is another important factor because aggressive periodontitis is known to have familial aggregation. Thus family members, especially younger siblings, of the patient diagnosed with aggressive periodontitis should be examined for signs of disease, educated about preventive measures, and monitored closely. It cannot be stressed enough that early diagnosis, intervention, and if possible, prevention of disease is more desirable than attempting to reverse the destruction that results from aggressive periodontitis.
Conventional Periodontal Therapy.
Conventional periodontal therapy for aggressive periodontitis consists of patient education, oral hygiene improvement, scaling and root planing, and regular (frequent) recall maintenance. It may or may not include periodontal flap surgery.3 Unfortunately, the response of aggressive periodontitis to conventional therapy alone has been limited and unpredictable. Patients who are diagnosed with aggressive periodontitis at an early stage and who are able to enter therapy may have a better outcome than those who are diagnosed at an advanced stage of destruction. In general, the earlier the disease is diagnosed, the more conservative the therapy and the more predictable the outcome.
Regenerative Therapy.
The concept and application of periodontal regeneration has been established in patients with chronic forms of periodontal disease (see Chapter 61). The use of regenerative materials, including bone grafts, barrier membranes, and wound-healing agents, are well documented and often used. Intrabony defects, particularly vertical defects with multiple osseous walls, are often amenable to regeneration with these techniques. Most of the success and predictability of periodontal regeneration have been achieved in patients with chronic periodontitis; much less evidence is available about the use of periodontal regeneration for patients with aggressive periodontitis.
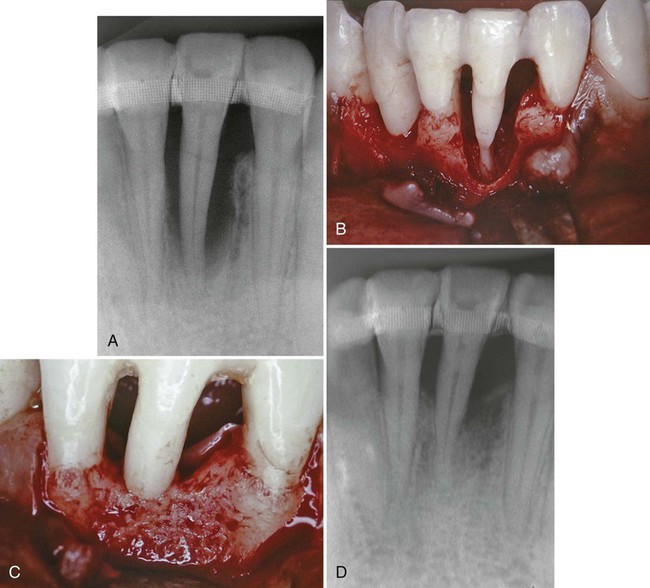
Periodontal regenerative procedures have been successfully demonstrated in patients with localized aggressive periodontitis in some clinical case reports. Dodson et al14 demonstrated the regenerative potential of a severe, localized osseous defect around a mandibular incisor in a healthy, 19-year-old black man diagnosed with localized aggressive periodontitis. The patient presented with severe bone loss localized around one of the mandibular incisors. Using open-flap surgical debridement, root surface conditioning (tetracycline solution), and an allogenic bone graft reconstituted with sterile saline and tetracycline powder, the surgeons reduced the probing pocket depth from 9 to 12 mm down to 1 to 3 mm (3 mm of recession was noted), and significant bone fill of the defect (about 80%) was reported (Figure 40-1). This case illustrates the potential for healing severe defects in patients with localized aggressive periodontitis, especially when local factors are controlled and sound surgical principles are followed. The authors cited several factors that likely contributed to the success of this case, including a probable transition of disease activity from aggressive to chronic, tooth stabilization before surgery, sound surgical management of hard and soft tissues, and good postoperative care.14
Antimicrobial Therapy.
The presence of periodontal pathogens, specifically Aggregatibacter actinomycetemcomitans, has been implicated as the reason that aggressive periodontitis does not respond to conventional therapy alone. These pathogens are known to remain in the tissues after therapy to reinfect the pocket.9,57 In the late 1970s and early 1980s, the identification of A. actinomycetemcomitans as a major culprit and the discovery that this organism penetrates the tissues offered another perspective to the pathogenesis of aggressive periodontitis and offered new hope for therapeutic success, namely, antibiotics.9 The use of systemic antibiotics was thought to be necessary to eliminate pathogenic bacteria (especially A. actinomycetemcomitans) from the tissues. Indeed, several authors have reported success in the treatment of aggressive periodontitis using antibiotics as adjuncts to standard therapy.33,34,35,70
There is compelling evidence that adjunctive antibiotic treatment frequently results in a more favorable clinical response than mechanical therapy alone.65 In a systematic review, Herrera et al23 found that systemic antimicrobials in conjunction with scaling and root planing offer benefits over scaling and planing alone in terms of clinical attachment level, probing pocket depth, and reduced risk of additional attachment loss. Patients with deeper, progressive pockets seem to benefit the most from systemic administration of adjunctive antibiotics. Many different antibiotic types and regimens were reviewed. Because of limitations in comparing data from different studies, however, definitive recommendations were not possible. In a meta-analysis of the literature (six randomized clinical trials were included), Sgolastra et al59 found that the systemic use of combined amoxicillin and metronidazole as an adjunct to scaling and root planing for the treatment of generalized aggressive periodontitis showed significant clinical attachment gain (p < 0.05) and pocket reduction (p < 0.05) as compared to scaling and root planing alone.
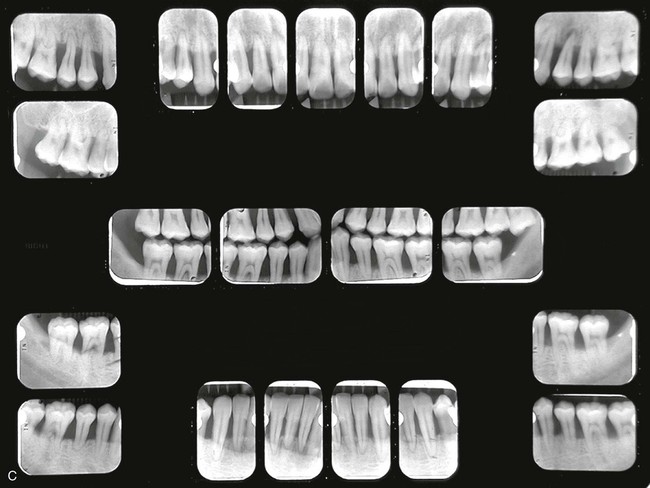
Figure 40-2 shows the before and after results of an aggressive periodontitis case treated nonsurgically with scaling and root planing and adjunctive antibiotic therapy. The patient, a 34-year-old Asian male, presented with a complaint of loose teeth and bleeding gums. He requested treatment to save his teeth. Treatment consisted of patient education including oral hygiene instructions and nonsurgical therapy with adjunctive antibiotics. All teeth were thoroughly scaled and root planed under local anesthesia over two treatment appointments, and the patient was treated with systemic amoxicillin (500 mg, 3 times a day for 2 weeks) during the period of treatment. All areas responded favorably with probing pocket depths decreasing from 3 to 13 mm down to 2 to 5 mm. Bleeding on probing diminished from generalized to very few isolated areas. He has been on periodontal maintenance with good results for more than 5 years.



Genco et al18 treated localized aggressive periodontitis patients with scaling and root planing plus systemic administration of tetracycline (250 mg, four times daily for 14 days every 8 weeks). Measurements of vertical defects were made at intervals of up to 18 months after the initiation of therapy. Bone loss had stopped, and one-third of the defects demonstrated an increase in bone level, whereas in the control group, bone loss continued.
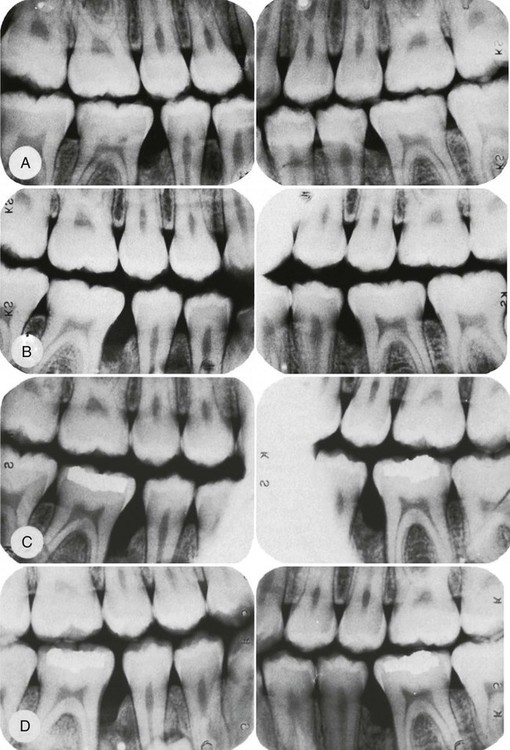
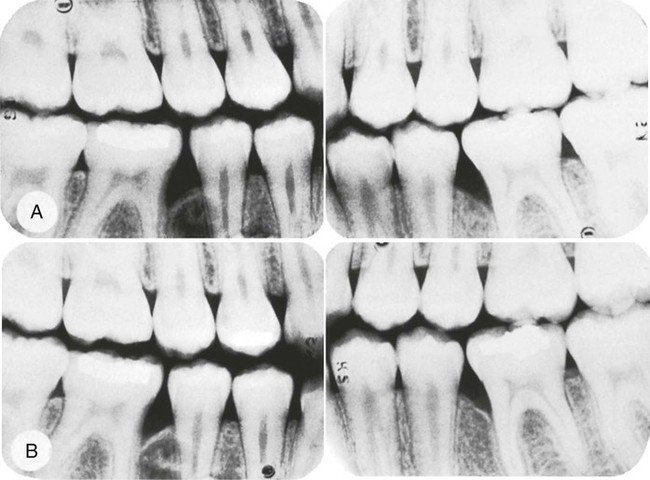
Liljenberg and Lindhe33 treated patients with localized aggressive periodontitis with systemic administration of tetracycline (250 mg, four times daily for 2 weeks), modified Widman flaps, and periodic recall visits (one visit every month for 6 months, then one visit every 3 months). The lesions healed more rapidly and more completely than similar lesions in control patients. These investigators reevaluated their results after 5 years and found that the treatment group continued to demonstrate resolution of gingival inflammation, gain of clinical attachment, and refill of bone in angular defects.34 Figures 40-3 and 40-4 show radiographs of a case with similar treatment and results.4
Clearly, numerous studies support the use of adjunctive tetracycline along with mechanical debridement for the treatment of A. actinomycetemcomitans–associated aggressive periodontitis (Box 40-1). Given the possible emergence of tetracycline-resistant A. actinomycetemcomitans, there is concern that tetracycline may not be effective. In these cases the combination of metronidazole and amoxicillin may be advantageous. The combination of these two antibiotics with conventional periodontal therapy21,22 provides better disease control and better clinical improvement in attachment levels in difficult-to-manage periodontitis cases than similar periodontal therapy without antibiotics. Similar effects were seen for a variety of antibiotic types. However, a lack of sufficient sample sizes among studies makes it difficult to offer specific recommendations about which antibiotics were most effective.23
The criteria for selection of antibiotics are not clear. Good clinical and microbiologic responses have been reported with several individual antibiotics and antibiotic combinations (Table 40-1). The optimal antibiotic or combination for any particular infection probably depends on the case. Choices must be made based on patient-related and disease-related factors.
TABLE 40-1
Antibiotic Therapy for Aggressive Periodontitis
| Associated Microflora | Antibiotic of Choice |
| Gram-positive organisms | Amoxicillin–clavulanate potassium (Augmentin)10,67 |
| Gram-negative organisms | Clindamycin19,20,63,67 |
| Nonoral gram-negative, facultative rods | Ciprofloxacin36 |
| Pseudomonads, staphylococci | |
| Black-pigmented bacteria and spirochetes | Metronidazole19,60 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


