It is likely that prehistoric people did not have the infections which we have associated today with impacted and partially impacted third molars. Although caries and periodontal disease were prevalent, evidence suggests that dental pathology was relatively low. Towards the end of the 17th century, people experienced an increase in the prevalence of dental disease, most likely as a result of shift in lifestyle and diet.
From that time until the advent of modern dentistry at the beginning of the 20th century, there was a dramatic acceleration in the rate of dental disease associated not only with third molars but also with every other tooth. Today, despite advances in preventive dentistry, the location of third molars in the dental arches often make them difficult to care for, and their frequent impaction exposes patients to degenerative conditions infrequently associated with any other tooth.
As a general principle, teeth should not be removed without due cause. This applies to unerupted/ impacted third molars as much as it does to any other teeth. All forms of surgery, whether under local anesthesia or general anesthesia, carry some risk of complications and there is an inevitable morbidity associated with surgical removal of teeth even in the best of hands. Apart from this, there is a question of cost involved. Therefore, there has to be a distinct reason for the removal of third molar tooth.
Even though not all unerupted/impacted teeth cause problems, all have that potential. Based on extensive
clinical studies the following indications for removal have been identified.
1. Pericoronitis and Pericoronal abscess: This is the most common cause for extraction of mandibular third molars (25 to 30%). Pericoronitis is commonly found to be associated with distoangular and vertical impaction. If improperly treated, infection may extent posteriorly resulting in sub masseteric abscess.
In certain cases chronic pericoronal abscess may point extra orally leading to difficulty in diagnosis regarding the focus of origin of infection (Figs 3.1 A to C)
The aim of a study conducted by Halverson et al (1992)1 was to obtain a predictive clinical profile of the impacted mandibular third molar at greatest risk for pericoronitis. It was noted that 81% involved vertically oriented while mesioangularly impacted accounted for only 11.2% of pericoronitis cases. The remaining cases comprised distoangular and horizontally impacted mandibular third molar (3.4% and 3.8% respectively). It was concluded that the risk for pericoronitis appears to increase with greater vertical orientation and higher the eruption.
2. Dental Caries: Incidence of caries of the 2nd molar or 3rd molar is about 15%. This high incidence is attributed to difficulty to perform oral hygiene measures in the third molar area (Figs 3.2 and 3.3).
Shugars and co-investigators (2004) noted a definite association between dental caries incidence in asymptomatic third molars and caries in restorations in second and first molars. One third of the study population had caries in the third molar. Almost all the patients who had caries in the third molar also had caries in the first or second molar. The absence of caries in the first or second molar was associated with caries-free third molar. Hence, removal of third molars maybe a prudent option to avoid caries of other molar teeth
Figs 3.1 A to C: (A) Chronic pericoronal abscess in relation to impacted third molar pointing extra orally (black arrow), (B) Intraoral view showing impacted 48 (green arrow), (C) Periapical X-ray showing horizontally impacted tooth with the root closely related to mandibular canal
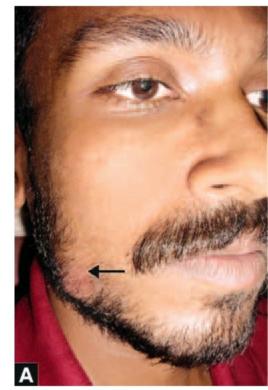

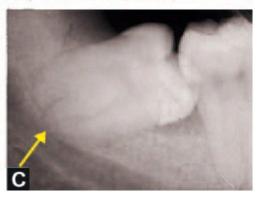

Fig.3.2: Horizontally impacted 38 with dental caries

Fig.3.3: Secondary caries beneath the restorations in 37 and 38 (yellow arrows)
Partially erupted impacted tooth with extensive caries can cause traumatic ulcer of buccal mucosa (Fig.3.4) or tongue.
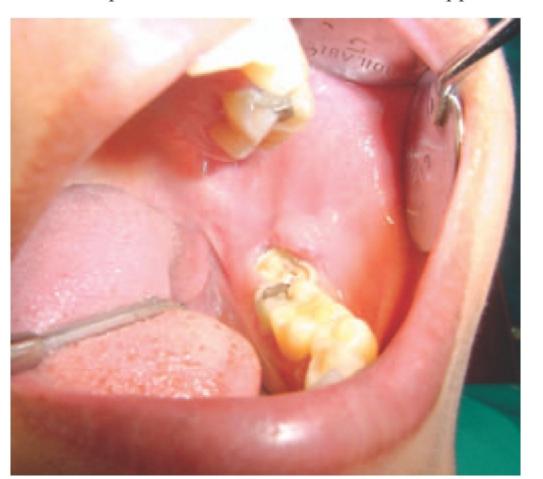
Fig. 3.4: Ulceration of buccal mucosa due to sharp margins of carious 38.
3.Periodontal diseases: Blakey et al (2002) reported that the prevalence of increased periodontal probing depths (PD) in the third molar region is higher than that is expected in asymptomatic third molars. They noted that in a sample of 329 patients 25% cases had at least one PD->5 mm in the third molar region. Increased periodontal probing depths and attachment loss leads to increased periodontal pathogen colonization and increased levels of inflammatory mediators. Various other studies have shown that chronic oral inflammation associated with periodontal disease has been implicated in increasing the risk of cardiovascular disease and renal insufficiency, restricted fetal growth and preterm births. Endothelial cell activation is the common cause for these clinical conditions.
Recurrent food impaction between the partially erupted third molar results in periodontal inflammation and subsequent bone loss. This weakens the support of the second molar and later on leads to pulpo periodontal involvement. Where there is periodontal disease and pocketing between the third molar and the second molar, there is some evidence to suggest that if removal of the third molar is delayed beyond the age of 30 years then the condition may become irreversible. Removal of the third molar will result in repair of the injured periodontium and therefore early removal of the impacted third molar is beneficial. Untreated horizontal and mesio-angular impactions are particularly prone to cause bone loss distal to the second molar (Fig.3. 5)
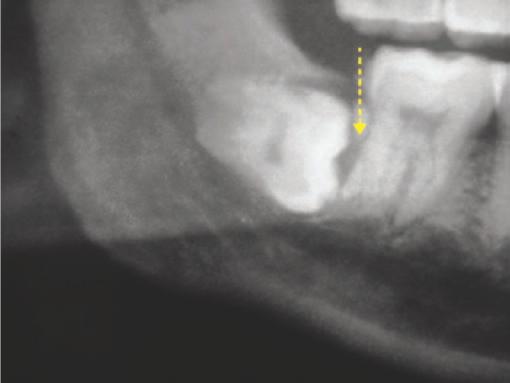
Fig.3.5: Horizontal impaction of 48 causing bone loss (yellow arrow) distal to 47
Late removal of such impacted teeth has not been shown to improve the periodontal status of the adjacent second molar, but early extraction of the impacted wisdom tooth reduces periodontal damage.
4. Orthodontic reasons:
a. Crowding of incisors: Third molars can produce an anterior component of force leading to crowding of mandibular incisors. Hence removal of third molars have been recommended during or after orthodontic treatment (Figs 3.6 A to C ).
Figs 3.6 A to C: (A) Crowding of mandibular incisors which is suspected to have originated secondary to impaction of 38 and 48 (B and C)


However, there has been much contention regarding the role of wisdom teeth in post-treatment change (commonly called relapse) after orthodontic treatment. Many still believe that they create pressure on the front teeth as they develop and erupt causing crowding of the lower anteriors. Much of the reasoning for this is that during the late teens to mid to late twenties, lower incisor crowding can be seen to develop in many cases and this also happens to be the most common age group for developing wisdom teeth to erupt or become impacted; hence the association.
The hypothesis that the mesial pressure from the third molars is transferred through the contact points resulting in the narrow contacts of the lower incisors is slipping. Recent studies have examined the strength of this hypothesis and the following statements can be made:
-The presence or absence of third molars, whether impacted or erupted, does not influence the amount of post-retention relapse following orthodontic treatment (Kaplan, 1974).
-There is no difference in mandibular incisor crowding between people who have third molars impacted, erupted normally, congenitally absent or extracted early (Ades et al, 1990).
-Direct measurement of proximal contact pressure before and after third molar extraction reveals no mesial pressure from impacted third molars (Southard at al, 1991).
-A critical review of the literature reveals a weak association between third molars and incisor crowding. Therefore, it is impossible to exclude third molars as a minor factor in the development of late incisor crowding (Vasir and Robinson, 1991).
On this basis, it can be concluded that although there are many valid reasons for third molar extraction, there is no reason to believe that extraction of third molars will alleviate or prevent crowding of incisors. Therefore, routine prophylactic removal cannot be justified solely for reasons of orthodontic stability.
b. To facilitate orthodontic treatment: Since current trends in orthodontics have shifted towards non-extraction therapy, molar distalization mechanics and treatment modalities have become increasingly popular especially in the management of Class II malocclusion. The use of headgear for molar distalization was followed by easier to use non-compliance intraoral appliances. In those cases where distalization of second molars is considered, extraction of impacted / erupted maxillary third molar tooth is indicated to facilitate the distal movement of maxillary molars.
5. To facilitate orthognathic surgery: In the presurgical preparation for orthognathic surgery, removal of third molars at the planned osteotomy sites should be considered. Bilateral sagittal split osteotomies (BSSO) can be better performed when third molars are not present at the site of osteotomy. Third molars (both erupted and unerupted should be removed preferably one year before the planned osteotomy to ensure the formation of adequate bone (Figs 3.7 A to D).




Figs 3.7 A to D: (A) Intra-oral photo of an 18-year-old young man with class III incisor relationship and mandibular excess who is being prepared to undergo surgical mandibular setback by bilateral sagittal split osteotomy (BSSO), (B) Cephalogram of the patient showing all features of mandibular excess. (C) OPG of the same patient showing impacted 38 and 48 with the apex incompletely developed (yellow arrows) which makes its surgical removal easy, (D) Extracted 48 showing the incompletely developed roots (yellow arrows)
Rigid fixation of the osteotomized segments is facilitated when there is adequate sound bone to secure plates and screws. Erupted maxillary third molars that are out of occlusion after a mandibular advancement should be considered before orthognathic surgery. However, maxillary third molars that are developing or are superiorly positioned are more easily removed at the time o/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses