Examination, Diagnosis, and Treatment Planning for General and Orthodontic Problems
Entirely opposite to the prevailing beliefs about the quiescence of the teenage years is the reality of a rapidly changing patient challenging his or her environment head-on and learning to cope in the process. The implications of these changes for dentistry1 are summarized as follows:
1. Rapid, unpredictable, and irregular skeletal and dental growth. The adolescent growth spurt is associated with accompanying facial growth of up to 35% of total height of the face. More than a dozen teeth, primary and permanent, exfoliate and erupt between the ages of 10 and 13 years. Immunologic changes, hormonal shifts, and other subtle and not so subtle physical developments alter the oral cavity.
2. The environmental challenges, with their obstacles and pitfalls. Few adults would choose to return to adolescence. Drugs, smoking, sexually transmitted diseases, peer pressure, acne, more competitive education, career decisions, alcohol, and family pressure are some of the challenges that today’s adolescent must face. Perhaps the most poignant statement on this aspect of the teenage years is that accidental death is the leading cause of mortality. Dental professionals see trauma, oral manifestations of sexual activity, hormonal gingivitis, smokeless tobacco–induced hyperkeratosis, noncompliance with dental recommendations, and drug-related behaviors, to mention a few examples.
3. The need to learn to cope, make decisions, and become independent. It is not surprising that primitive cultures associated emerging adulthood with rituals and great significance. Adolescence has always been a time to make decisions, seek independence from families, deal with sexuality, and choose a career. The dentist may see this turmoil reflected in poor compliance with oral hygiene or refusal to accept treatment. The missed appointment is just one of many ways to say, “I am too involved in my search for self, my changing values, and handling my environment to worry about my teeth.”
The Patient History
• Every day, approximately 3000 teenagers start smoking.
• Out-of-wedlock births have increased by 50% in recent years.
• Radiation and medications used in dentistry can be dangerous to a fetus.
• The majority of adolescents now try drugs or alcohol before leaving high school. Untoward interactions between prescribed and illicit medications can be fatal.
• Sexually transmitted diseases are epidemic in the adolescent age group.
• Encourage parents to complete histories with adolescents, not for them.
• Allow the adolescent the opportunity to contribute to the history alone, which can be done in the context of a final check before treatment at chairside.
• Never treat an adolescent without a consenting parent available. Dental care would be considered nonurgent care and most jurisdictions require adult consent.
• Explain suspicions or concerns to both parent and adolescent.
• Establish a policy on deferring treatment and dealing with identified problems of a serious nature that is medicolegally consistent and sound.
• Have resources available in case consultation with a specialist is needed. It is far better to have an established professional relationship than to seek help from a stranger.
The Examination
The techniques of clinical examination remain the same for the adolescent, but closer attention is paid to identification of problems specific to this group, such as occlusal disharmonies, periodontal conditions, and temporomandibular joint disorders. Table 37-1 lists some of the clinical findings peculiar to adolescent patients.
Behavioral Assessment
1. Sexual abuse. The young adolescent girl or boy who has been sexually abused with oral penetration may be reluctant to accept dental care from a dentist of the same sex as the perpetrator. Aids in uncovering this situation are a good history of previous compliance, behavioral cues such as depression, and overt refusal of care when oral contact is made. Nonetheless, confirmation is difficult because the parents may be unaware of the abuse. It may be the limit of the dentist’s role to recommend counseling for such a child in the hope that intervention may uncover the cause.
2. Rampant caries. Clinicians have noted that rampant caries, a condition of rapid onset and progression of decay in an adolescent (more often a girl), is often associated with personality problems (Figure 37-1). The typical manifestation is a shy, reluctant, introverted person who is passive about treatment. The behavioral signs can be varied, with the girl crying silently or not saying a word during the appointment. In some cases, appointments can degenerate as the child whimpers and finally loses her composure. Time and engagement in conversation are often the most successful behavioral management keys in dealing with these adolescents. Dramatic changes in behavior can occur with the dentist’s verbal reinforcement of improved hygiene and provision of even temporary aesthetic anterior restorations that allow the patient to smile and experience a more positive self-image.
3. Extreme anxiety. Pinkham and Schroeder2 described the behavioral management of the child who shows extreme anxiety at the prospect of dental treatment. Desensitization by psychological intervention may be the key to development of acceptable clinical behavior in such children. Tools available to the dentist are the use of noninvasive therapies at first, reinforcement of positive accomplishments, positive peer interaction, and involvement with a psychologist. The poorly treated or untreated adolescent phobic may become the adult dental phobic.
4. Eating disorders. Treatment of the child with an eating disorder can be difficult. Experience indicates that these patients, disproportionately girls, tend to develop dependency on a male authority figure. They also require a dentist’s full attention during office visits and, unless counseled, may demand time outside scheduled appointments.
5. Illicit drug use. Clinicians have noted bizarre behavior on the part of adolescents and young adults who present for treatment after taking nonprescription medications. A number of untoward reactions to dentist-administered medications have been associated with prior ingestion of drugs or alcohol by a young patient. Manifestations of drug ingestion may vary from a slight mental dissociation or drifting to outright verbal aberrations or extreme changes in personality.
1. Peers are important. The adolescent’s relationship to those outside the nuclear and extended family becomes important. Friends, classmates, teammates, and popular persons of similar age are all involved in the life of the teenager. A dentist can enhance his or her ability to communicate with adolescents by asking about peer interaction and by knowing who is involved in the teen’s life.
2. Fads and experimentation are part of adolescence. Successful adolescent practitioners are those who are aware of the trends, popular fads, and celebrities that are of interest to teens. A clear demonstration of this to teens is the presence of posters or contemporary music in the operatory. The dentist who knows the trends and interests of the adolescent has an edge in establishing communication and in reaching the teen on a nonauthoritarian basis. These are an entree into the teen’s world that can be fostered and can lead to discussion of more significant issues with a sense of relationship. Contrast that access to the barrier that arises when both teen and dentist see themselves as worlds apart.
3. Teens are trying to establish independence, searching for identity, making educational or career choices, and experimenting with sexuality. All of these involve a certain degree of stress. Within that stressful period are times of anxiety, satisfaction, anger, excitement, and a host of other emotions. The dentist is a small part of the adolescent’s world but is a mirror of it. How the practitioner fosters the healthy development of personality in a child and counsels him or her toward independence and career may be important in terms of both the teen’s life and his or her dental health. In talking with teens, it is helpful to remember their “problem list” and to empathize about the stress of their lives, which is real to them. The office visit should be a mirror of life. It should provide a respite from pressures and be a cameo of the role that the adolescent plays as an adult patient. The relationship that the dentist would like to have with the adolescent as an adult should be fostered.
4. The basis of success in adolescent-adult interactions is a good relationship. The most significant factor in successful compliance and communication is the quality of the relationship between the dentist and the adolescent. In earlier periods of life, the child could be successfully motivated with reason, praise, or other approaches. The changing values and their short-term intensity in adolescence belie the use of these approaches in fostering long-term motivation. A feeling of trust, good communication, and a perception by the teenager of the dentist’s sincere interest provide a strong motivation for compliance.
Determination of Developmental Status
The most important question usually faced is whether patients are still growing facially, so that the timing of surgical care can be instituted for those with excess growth issues like mandibular protrusion or vertical excesses. The most reliable and sensible method, which speaks directly to this issue, is taking serial cephalometric radiographs and superimposing their tracings (see Figure 30-53). This method is helpful not only for orthodontic treatment planning, but also for determining when implant placement is feasible relative to vertical facial growth.
Periodontal Evaluation
In the adolescent more emphasis is placed on the periodontal examination. The prevalence of periodontal disease begins to increase in this age group.3 The reason for this increase in periodontal disease is unknown at this time. Therefore a thorough evaluation of the supporting structures is an absolute necessity. A periodontal probe is used to measure pocket depths, the width of keratinized gingiva, and the amount of attached gingiva, and to establish a bleeding index (Figure 37-2). Periodontal probing should be confined to fully erupted teeth. Mobility tests may reveal slightly increased mobility in erupted teeth without complete root formation. The use of disclosing agents to reveal plaque, though helpful, may be discontinued at the patient’s request. If a panoramic radiograph is used for diagnosis, selected periapical films may be needed if the clinical examination exposes any unusual periodontal findings. Referral to a specialist is suggested if significant periodontal disease is evident. During orthodontic treatment, gingival, plaque, and bleeding indices should be established at regular intervals to detect newly active periodontal disease. Over the next decade, the increase in overweight and obesity with attendant increase in early-onset diabetes may yield more adolescents with early periodontal disease and bone loss. But to date, studies are equivocal on this relationship and dentists should simply include periodontal evaluation as a part of the adolescent examination.
Related Hard and Soft Tissue Problems
A number of pathologic conditions may occur in adolescence and may be first noticed in this period. One is temporomandibular joint disorder (TMD), described in more detail later in this chapter. An eating disorder can manifest as enamel erosion of all teeth if vomiting is a regular component of this psychiatric disorder.4 Bulimia is the term given to characterize those who vomit regularly to purge themselves of food in a misdirected attempt to control their weight. Bulimia affects far more girls than boys, but boys can exhibit similar behavior. The regurgitated stomach contents, which are highly acidic, erode the enamel of teeth in a process called perimolysis (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline TABLE 37-1
TABLE 37-1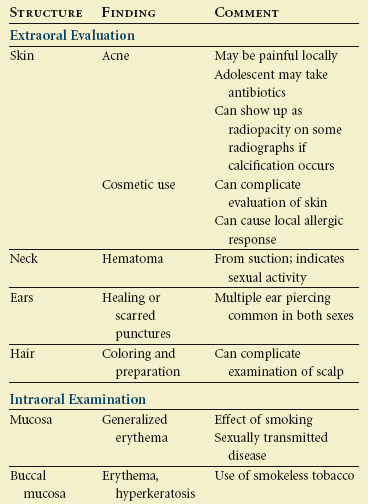

 FIGURE 37-1
FIGURE 37-1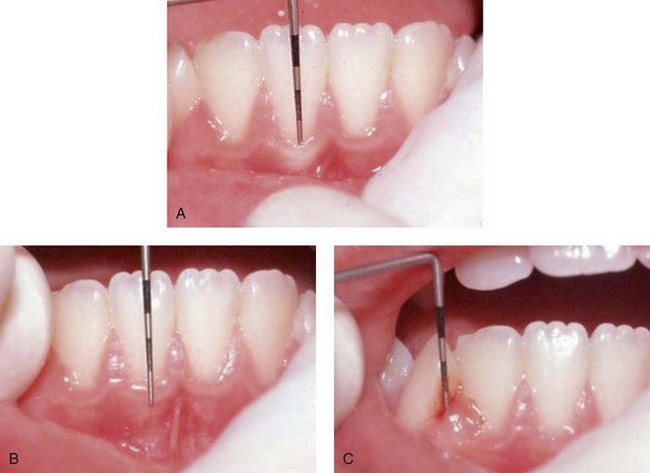
 FIGURE 37-2
FIGURE 37-2