Managing Traumatic Injuries in the Young Permanent Dentition
Injuries to the primary dentition are discussed in Chapter 15. Also covered there are the following fundamental areas relevant to managing trauma in children of any age:
This chapter deals with injuries to the young permanent dentition, but the reader is strongly advised to review the fundamental areas just noted in Chapter 15. Frequent reference will be made to them.
The reader is encouraged to review and use an excellent online resource, “The Dental Trauma Guide” (www.dentaltraumaguide.org),1 to assist in diagnosing and treating tooth injuries. This guide, developed by Dr. Jens O. Andreasen and sponsored in part by the University Hospital, Copenhagen, and the International Association of Dental Traumatology, contains updated guidelines on a broad array of injuries and is easy to use.
Etiology and Epidemiology of Trauma in the Young Permanent Dentition
Falls during play account for most injuries to young permanent teeth. Children engaging in contact sports are at greatest risk for dental injury, though the use of mouth guards greatly reduces their frequency (see Chapter 40). In the teenage years, automobile accidents cause a significant number of dental injuries when occupants not wearing seat belts hit the steering wheel or dashboard. As noted in Chapter 15, children with seizure disorders also injure their permanent teeth more frequently. In contrast to the primary dentition, permanent teeth suffer crown fractures more frequently than luxation injuries. The lower crown/root ratio and denser alveolar bone in the permanent dentition contribute to this phenomenon. Maxillary central incisors are again most commonly injured, and protruding incisors are at greatest risk (Figure 34-1).2
Classification of Injuries to Young Permanent Teeth
Classification of tooth fractures and luxation injuries is discussed in Chapter 15 (see Figure 15-1).
History
The essential elements of the medical and dental history are discussed in Chapter 15. The use of a trauma assessment form to help organize the gathering of historical and clinical data is emphasized (see Figure 15-8). The reader is reminded to determine the status of the child’s tetanus prophylaxis and to consult the child’s physician if there is any question about its adequacy.
Another issue worthy of review relates to the potential for injury to the central nervous system. Older children are likely to suffer harder blows at play, and thus the dentist should find out if the child lost consciousness or became disoriented or nauseated after the injury. Positive findings indicate immediate medical consultation. As noted in Chapter 15, significant head injuries can lead to symptoms many hours after the initial trauma, and parents should be cautioned to watch for the signs noted previously for 24 hours, including waking the child every 2 to 3 hours throughout the night.3
Clinical Examination
Refer to Chapter 15 for a thorough discussion of the clinical examination. An important difference between the primary and permanent dentition exists in respect to “vitality” or sensibility testing. Whereas it is not routinely performed in the primary dentition, sensibility testing can be a useful diagnostic aid in the permanent dentition. The dentist should be aware that pulp testing might not elicit reliable responses from erupting permanent teeth and from those with open apices. Furthermore, recently traumatized teeth may not respond to any sensibility test for several months. Positive findings following a traumatic injury are thus more valuable for assessing pulp vitality than are negative responses.
Cold testing with agents like difluorodichloromethane or carbon dioxide snow yield the most reliable results,4 although the thermal shock of the low temperature applied can cause infraction lines in the enamel.5 Some clinicians prefer electrical vitality testing because it uses a stimulus that can be gradually increased and precisely recorded.
Pulp tests that use cold or electrical impulse do not actually measure “vitality” because that requires confirmation of uninterrupted blood flow through the pulpal tissue. Instead, these tests measure neural response, which serves as a proxy for vascular health. Laser Doppler flowmetry has potentially great clinical value because this technique directly measures blood flow and does not rely on sensory nerve response.6 The technique is also painless and is reliable in teeth with immature apices.7 However, modifications in this instrument’s design and a significant reduction in its cost are necessary for it to achieve widespread use. Another noninvasive technique that has potential diagnostic value is pulse oximetry,8 which measures blood oxygen saturation in the vessels monitored. Although there is currently no commercial product available, future technological advances will enable development of affordable devices that attach to teeth and will give the clinician a better measure of tooth vitality.
Principles of radiographic diagnosis for permanent teeth do not differ from those for primary teeth. A common error made by dentists in diagnosing traumatic injuries is to take an insufficient number of radiographs. Additional views taken from slightly different angles both vertically and horizontally can significantly improve the accuracy of diagnosis.9
It is important to note the urgency of follow-up radiographs after injury. Reviewing radiographs at 1 month after injury will detect signs of pulpal necrosis and inflammatory resorption. At 2 months, replacement resorption can be detected.9
Pathologic Sequelae of Traumatized Teeth
Refer to Chapter 15 for a discussion of the pathologic sequelae of traumatized teeth.
Treatment of Traumatic Injuries to the Permanent Dentition
The dentist treating a traumatic injury follows essentially the same principles of gathering historical information and completing a clinical examination, regardless of the child’s age. Furthermore, the pathologic sequelae of injuries to teeth are similar for both primary and permanent teeth. However, there are many significant differences in the way that injuries to permanent teeth are treated. As in the primary dentition, a complete diagnostic workup (described in Chapter 15) should precede all treatment. Even though a blow may cause little if any obvious injury to a permanent tooth, it may lead to pulp necrosis as a result of disruption of the neurovascular bundle at the apex of the tooth. Posttreatment evaluation is indicated for all traumatic injuries.
Enamel Fractures
In some cases, minor enamel fractures can be smoothed with fine disks. Larger fractures should be restored using an acid-etch/composite resin technique (see Chapter 39).
Enamel and Dentin Fractures
The primary issue in managing fractures that expose dentin is to prevent bacterial irritants from reaching the pulp. Standard care in the past called for covering exposed dentin with calcium hydroxide (CaOH) or glass ionomer cement to seal out oral flora. Recent research indicates that sealing exposed dentin with a bonding agent enables the unexposed pulp to form reparative dentin. Some clinicians are thus advocating simultaneous acid etching of dentin and enamel followed by dentin and enamel bonding without placement of CaOH or glass ionomer.10 However, a recent review of pulp capping with dentin adhesive systems reported that these systems are not indicated owing to increased inflammatory reactions, delay in pulp healing, and failure of dentin bridge formation.11 This author recommends covering the deepest portion of dentin fractures with glass ionomer cement, followed by a dentin-bonding agent (see Chapters 20 and 39). The tooth can then be restored with an acid-etch/composite resin technique (Figure 34-2). If adequate time is not available to restore the tooth completely, an interim covering of resin material (a resin “patch”) can temporize the tooth until a final restoration can be placed. Some dentists routinely place such a partial restoration to ensure an appropriate posttreatment evaluation when the patient returns for the final restoration. This is a reasonable strategy, provided that care is taken to ensure an adequate seal.
Fractures Involving the Pulp
Management of crown fractures that expose the pulp is particularly challenging (Figure 34-3). Pertinent clinical findings that dictate treatment include the following:

 FIGURE 34-3 Crown fracture exposing the pulp.
FIGURE 34-3 Crown fracture exposing the pulp.
1. Vitality of the exposed pulp
2. Time elapsed since the exposure
The objective of treatment in managing these injuries is to preserve a vital pulp in the entire tooth (see Chapter 33). This allows for physiologic closure of the root apex in immature teeth. It is important to note that root end closure does not signal completion of root maturation. Progressive deposition of dentin normally continues in roots through adolescence, making them stronger and more resistant to traumatic insult. Maintaining a vital pulp in the tooth crown allows the clinician to monitor the tooth’s vitality periodically.
Direct Pulp Cap
A rubber dam is applied, and the tooth is gently cleaned with water. Commercially available CaOH paste or mineral trioxide aggregate (MTA)12,13 is applied directly to the pulp tissue and to surrounding dentin. It is essential that a restoration be placed that is capable of thoroughly sealing the exposure to prevent further contamination by oral bacteria. As in the management of dentin fractures, it is acceptable to use an acid-etch/composite resin system for an initial restoration. A calcific bridge stimulated by the capping material should be evident radiographically in 2 to 3 months.
Pulpotomy
It is difficult to determine clinically how far the inflamed pulp extends. The tooth shown in Figure 34-4 had been fractured for 4 days with a pulp exposure approximately 3 mm in diameter. The dentist elected to remove all tissue in the pulp chamber, with obvious success. Figure 34-4, B, demonstrates complete maturation of the root, including apical closure and dentinal wall thickening as well as a calcific barrier at the amputation site. However, maintaining some pulp tissue in the crown allows the dentist to monitor the vitality of the tooth and thus is preferable when possible.
In 1978, Cvek14 noted that in most cases of pulps exposed for more than a few hours, the initial biological response is pulpal hyperplasia. Inflammation in these cases rarely extends beyond 2 mm. In his study involving 60 teeth with pulps exposed from 1 hour to 90 days, Cvek removed only 2 mm of the pulp and the surrounding dentin. He covered the pulp stumps with CaOH and reported a success rate of 96%.14 The long-term success reported by Fuks and colleagues15 confirms these findings and indica/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline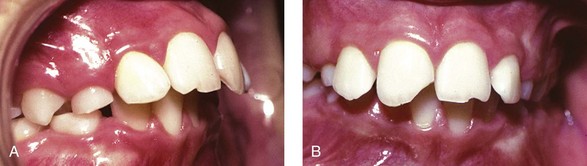
 FIGURE 34-1
FIGURE 34-1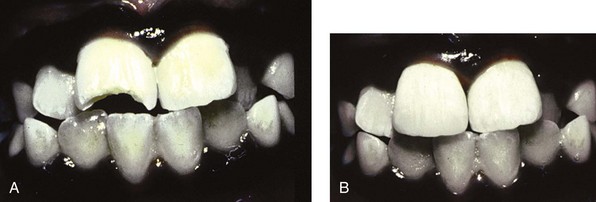
 FIGURE 34-2
FIGURE 34-2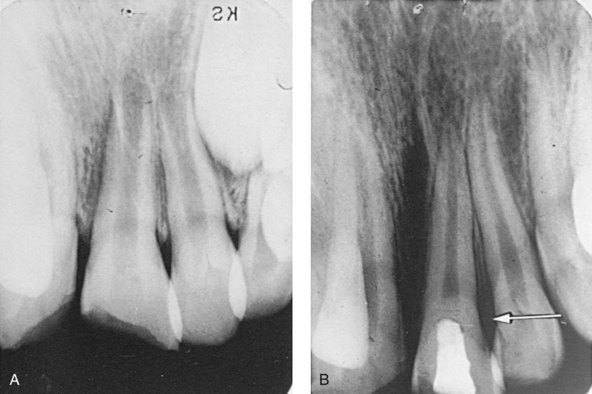
 FIGURE 34-4
FIGURE 34-4