Examination, Diagnosis, and Treatment Planning of the Infant and Toddler
Break the Cycle of Early Childhood Caries
Disrupt the Acquisition of Harmful Microflora
Manage the Risk/Benefit of Habits
Establish a Dental Home for Health or Harm
Impart Optimal Fluoride Protection
Use Anticipatory Guidance to Arm Parents in the Therapeutic Alliance
Concepts of Infant Oral Health
Infant Oral Health as a Diagnostic Process
Elements of the Infant Oral Health Visit
Growth and Development Treatment Planning
Office Readiness for Infant Oral Health
Responsibility of Nondental Professionals Regarding Infant Oral Health
Infant Oral Health
In 1986, the American Academy of Pediatric Dentistry adopted a position on infant oral health recommending that the first visit occur within 6 months of the eruption of the first primary tooth.4 This bold recommendation was based on the recognition that many children by age 3 years had already experienced dental caries and, more troubling, that those who had experienced caries remained prone to recurrent decay, even with subsequent preventive intervention.5 For many years before adoption of that policy and to this day, physicians claim responsibility for the oral health of the child younger than 36 months.9 The rationale, though somewhat circuitous, assumed that children visited a physician from birth at regular intervals but did not see a dentist until later in life. Unfortunately, physicians’ knowledge and inclination to practice preventive dentistry have been shown to be lacking. In fact, whereas the incidence of permanent tooth dental caries has declined consistently over the last three decades, that of primary tooth caries has not, and it remains to be seen whether the medical community can effect a change in that pattern.
Effecting a major shift in health behavior, such as instituting an infant oral health visit to a dentist, is not without problems. Some dentists are still reluctant to see these children because of expectations of negative behavior, a lack of understanding of preventive opportunities, and concern about reimbursement for procedures.39 Rightfully, physicians question whether a major shift in practice that places infants in dental offices will work, given the reluctance of dentists and the scarcity of pediatric dentists who might see these children.
The purpose of this chapter is to describe the objectives, procedures, and rationale for infant oral health. The chapter will focus mainly on preventive aspects of infant oral health, and the reader can look to Chapter 18 for more information on diagnosis and treatment planning for children 3 years and older. The care of the infant patient offers the unique opportunity to begin with a clean slate and keep it there; at no other point in life will the dentist have the same level of parental concern, attention, and compliance.
Goals of Infant Oral Health
Nowak has outlined the rationale for infant oral health, providing a logical and compelling argument for seeing a child at a time when dental caries has not had time to develop, habits are still beneficial, and the entire dental preventive armamentarium is available.31 The goals can be summarized by the following six tenets.
Break the Cycle of Early Childhood Caries
Primary tooth caries, now called early childhood caries, remains a problem for many children. In many studies, by 5 years of age, as many of half of children have experienced dental caries. In subpopulations of poor and minority children, the rate is higher and the condition begins earlier.29 Although the cause of such early-onset disease remains unknown, the concentration of disease in certain populations suggests that diet, microflora, and even prenatal factors may be contributory. Of even more concern is the cyclic nature of early childhood caries, in which children afflicted remain at risk throughout childhood, even when preventive services are available.5 Although it remains to be demonstrated that early intervention can prevent caries and its recurrence in at-risk children, it is difficult to ignore the much larger percentage of caries-free children who have access to care and prevention.
Disrupt the Acquisition of Harmful Microflora
Research suggests that children are inoculated with caries-initiating bacteria vertically by caretakers, primarily mothers. The relationship between maternal salivary levels of mutans streptococci (MS) and the risk of infant infection seems to be relatively strong because mothers with high levels of MS tend to have children with high levels, whereas those with low levels tend to have children with low levels.17 If a child’s caretaker harbors virulent organisms, then transmission via kissing, shared food, or other contact can occur and begin the caries process.43 Horizontal MS transmission, between members of a family or groups such as those found in daycare, has also been reported in the literature, but is generally not thought to be the primary mode of transmission in most populations.3 On the plus side of this acquisition model is the potential to prevent transmission, reduce the caretaker’s bacterial inoculum, or use antibacterial chemotherapeutic agents to eliminate the infection before it becomes chronic and leads to dental caries. In a general dental practice, prenatal counseling, maternal oral health, and infant oral health form the chain for prevention of bacterial acquisition.
Establish A Dental Home for Health or Harm
The concept of a dental home has been suggested as a means to focus preventive, treatment, and referral services to optimize oral health.32 Our physician colleagues understand the benefits of establishing a doctor-family relationship. Care is begun with nonthreatening preventive services; if an emergency occurs, parents know where to turn; if questions arise, reliable and trusted information is available; if treatment is needed, a firm foundation of trust has been built. The U.S. Surgeon General’s report notes quite clearly that those children who have a dentist are more likely to receive preventive services.42 Research has shown that early preventive oral health care targeted to high-risk populations can lower overall dental costs and yield better oral health outcomes.37 Reports of preschool-aged, Medicaid-enrolled children have shown that the earlier a preventive dental visit occurred, the more likely these children were to use subsequent preventive services and experience lower dentally related costs.25 From the standpoint of a general dental practice, the one-stop, family orientation is a strong factor in success.
Impart Optimal Fluoride Protection
Fluoride remains dentistry’s best preventive tool, and optimal fluoride exposure is a tenet of early intervention. The current concern about fluorosis gives even more importance to oversight of fluoride exposure during the period when teeth are at greatest risk, in the first 3 years of life. Physician-driven fluoride supplementation has not been very effective, and with current recommendations of the Centers for Disease Control and Prevention that require caries risk to be added to the equation, dentist involvement is crucial to maximize anticaries benefit and minimize fluorosis risk.20
Concepts of Infant Oral Health
Risk Assessment
An infant presents a clean slate in terms of acquired conditions and diseases, but as the child grows and expands his or her world, risk increases. Taking a broad view of risk that goes beyond infectious disease and encompasses trauma and injury, orthodontic problems, and compliance issues helps ensure total oral health. Risk assessment is defined as identification of factors known or believed to be associated with a condition or disease for purposes of further diagnosis, prevention, or treatment. According to the American Academy of Pediatric Dentistry guidelines, “risk assessment: 1. fosters the treatment of the disease process instead of treating the outcome of the disease; 2. gives an understanding of the disease factors for a specific patient and aids in individualizing preventive discussions; 3. individualizes, selects, and determines frequency of preventive and restorative treatment for a patient; and 4. anticipates caries progression or stabilization.”5 Current caries-risk assessment models entail a combination of factors including diet, fluoride exposure, a susceptible host, and microflora that interact with a variety of social, cultural, and behavioral factors. An essential part of the infant oral health visit is a specialized history addressing risk. Risk assessment is an offshoot of wellness theory in that a child may exhibit risk but not demonstrate overt disease. By eliminating the risk factors before disease occurs, the disease process can be prevented in the immediate future as well as in the long term. An example would be the infant sleeping with a bottle of sweetened liquid but with no overt dental caries. Intervention would be focused on eliminating the habit and diminishing the risk of early childhood caries. Table 13-1 depicts the caries-risk assessment form developed by the American Academy of Pediatric Dentistry, which can be used by health professionals to identify risk for dental caries in children of all ages, beginning at 6 months.5 The American Academy of Pediatric Dentistry has also developed caries management protocols, with the objective to assist health care providers in the decisions regarding individualized treatments. These protocols are based on the patients’ caries risk levels, age, and parental compliance with preventive strategies recommended, and aids practitioners in determining the types and frequency of diagnostic, preventive, and restorative care for dental caries management. Such protocols should increase the probability of more successful and cost-effective treatments. An example of a caries management protocol for children 1 to 2 years old is shown in Table 13-2.5
 TABLE 13-1
TABLE 13-1
Caries-Risk Assessment Form from Birth to 5 Years Old (For Dental Providers)
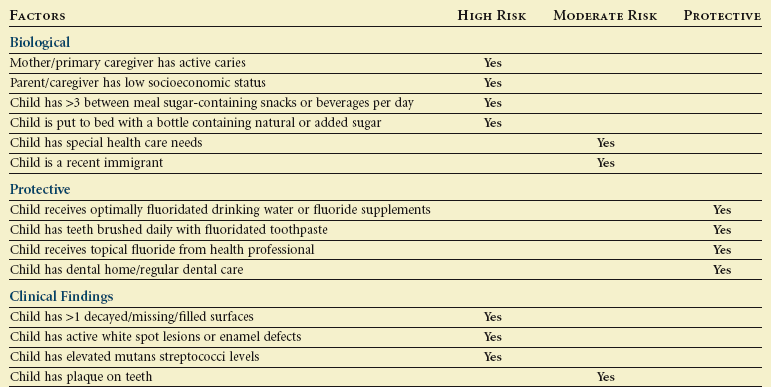
Overall assessment of the child’s dental caries risk: High  Moderate
Moderate  Low
Low 
From American Academy of Pediatric Dentistry: Clinical guideline on caries-risk assessment and management for infants, children, and adolescents, Pediatr Dent 33(special issue):110–117, 2011.
 TABLE 13-2
TABLE 13-2
Example of a Caries Management Protocol for 1- to 2-Year-Old Children
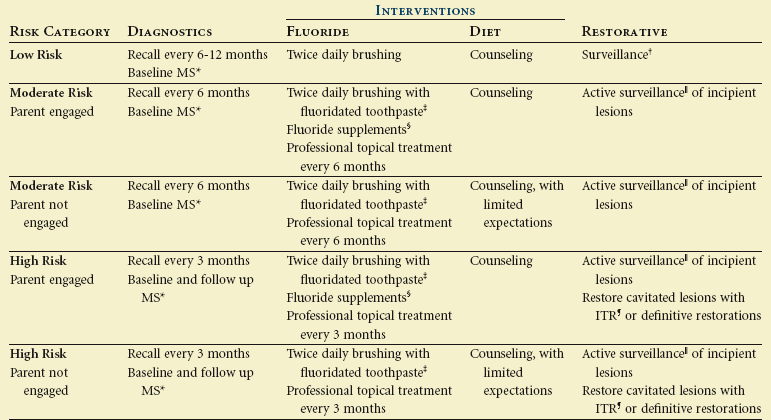
*Salivary mutans streptococci bacterial levels.
†Periodic monitoring for signs of caries progression.
‡Parental supervision of a “smear” amount of toothpaste.
§Need to consider fluoride levels in drinking water.
 Careful monitoring of caries progression and prevention program.
Careful monitoring of caries progression and prevention program.
¶Interim therapeutic restoration.
From American Academy of Pediatric Dentistry: Clinical guideline on caries-risk assessment and management for infants, children, and adolescents, Pediatr Dent 33(special issue):110–117, 2011.
Anticipatory Guidance
The concept of anticipatory guidance is long established in pediatric care but relatively new to dentistry. Our preventive message has tended to be static and not tailored to the developmental stage of the patient. Throughout childhood and later life, environment and growth and development force change; the infant is very different from the school-aged child and lives in a broader, more complex world. Even in adulthood, the elderly patient’s needs are far different from those of a middle-aged person. Anticipatory guidance is defined as proactive counseling of parents and patients about developmental changes that will occur in the interval between health supervision visits. Guidance includes information about daily caretaking specific to that upcoming interval. Anticipatory guidance is the complement to risk assessment; addressing protective factors is aimed at preventing oral health problems. An example of anticipatory guidance would be to discuss ambulation of the child at the initial dental visit and warn parents about possible tooth trauma that often occurs as the infant stands to walk. Authors have recommended that anticipatory guidance areas include oral development, fluoride adequacy, nonnutritive habits, diet and nutrition, oral hygiene, and injury prevention.33 These six areas capture the major concerns related to major oral conditions of dental caries, periodontal disease, trauma, and malocclusion.
Health Supervision
Regular, comprehensive preventive and therapeutic dental care for every child is far superior to fragmented episodic care and therefore is a worthwhile goal. Health supervision is defined as the longitudinal partnership between dentist and family individualized to focus on health outcomes for that family and child. This is a departure from the “every 6 months” approach that is common to dental practice and that frankly has no strong basis. Some children require more frequent supervision visits and others less. The health supervision interval is the alternative to the traditional recall period, and the health outcome is the desired changes monitored at each interval. In infant oral health, the dentist assesses risk at the beginning of the interval, offers preventive advice using anticipatory guidance, and administers necessary treatment or prevention in the dental office. Outcomes are the measures that indicate success. These can be physical (reduction in gingival inflammation), cognitive (understanding of the caries process), or behavioral (elimination of the nighttime bottle habit). For example, the presence of plaque on primary teeth in infants is a strong predictor of future dental caries, so after oral hygiene instruction, parents can monitor success by looking for the presence of plaque.2 A desired outcome would be absence of plaque. Parents leave armed not only with tools (anticipatory guidance) to effect outcomes but also with measures (outcomes) they can look for and that the dentist also uses at the end of the supervision interval to determine success.
Elements of the Infant Oral Health Visit
Risk Assessment
The parent or guardian is the historian for the child. In Chapter 18, the general health history is discussed in depth. In this chapter, we will focus on historical elements related to oral disease risk. Box 13-1 depicts a risk assessment form for infant oral health.6 Historical risk elements can be divided into perinatal factors, diet and nutrition, fluoride adequacy, oral hygiene, bacteria transmission, oral habits, injury prevention, and oral development. The clinician should combine the general health history responses described previously with those focused on risk of oral disease (i.e., demographic information and clinical findings) to form an individual historical risk profile for the child and help in determining preventive and treatment strategies.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline Box 13-1
Box 13-1