Treatment Planning and Management of Orthodontic Problems
When considering treatment for problems during the mixed-dentition years, the precise problem and the goals of treatment must be clearly in mind. Few problems will receive definitive or complete treatment at this stage of development, although some simple and isolated dental problems may be resolved. As always, information regarding the patient’s problems is gathered through an interview of the patient and the parents and a clinical examination. First, a list of goals is created by the clinician. The goals should address functional and aesthetic concerns of the patient and the clinician. After the goals of treatment have been established, a list of orthodontic problems is generated from this database, and the problems are ranked in order from most to least severe.1 The order is determined by patient, functional, and aesthetic concerns. The clinician is specifically trained to identify functional and aesthetic problems. This problem list does not always match the concerns of the parent and child. These concerns should be listened to carefully and often dictate treatment direction and treatment satisfaction outcomes. Many times the motivation for treatment can be elicited from these concerns. If the child patient desires to have treatment, cooperation will usually be good during treatment, and little parental support will be necessary. This is called internal motivation. External motivation, motivation supplied by the parent for treatment, will require continuous parental support to successfully complete treatment. If the chief complaint or reason for seeking treatment ranks low on the treatment priority list or will be addressed later in the treatment plan, an explanation should be provided to the child and parent to justify this situation.
Skeletal Problems
Three basic alternatives for treating skeletal discrepancies exist: growth modification, camouflage, and orthognathic surgery. Growth modification is a means to change skeletal relationships by using the patient’s remaining growth to alter the size or position of the jaws. Camouflage and orthognathic surgery usually are considered for adolescent patients with minimal or no growth remaining or nongrowing adult patients. Camouflage orthodontic treatment is aimed at hiding a mild skeletal discrepancy by moving teeth situated on the jaws so that they fit together. The skeletal discrepancy still exists, but it is disguised by a compensated occlusion and acceptable facial aesthetics. Orthognathic surgery places the jaws and teeth in a normal or near-normal position through the use of surgical procedures and presurgical and postsurgical orthodontic treatment.2 For the mixed-dentition patient, only growth modification or no treatment is a reasonable choice for skeletal intervention.
Growth modification during the early mixed-dentition years rests on several assumptions that are not as clear as many would presume. First, a child must be growing for the growth to be modified. Most normal children in the 6- to 12-year age group are actively growing, and their faces are also growing. Furthermore, clinicians have thought that it is easiest to correct skeletal problems if a child is undergoing maximal facial growth during treatment. Although the data to support this contention are not voluminous or clear,3 clinicians have long sought to predict maximum somatic growth and maximal facial growth from other indicators. There appears to be wide variation in the amount of facial growth occurring at one time and an equally wide variation in the correlation of facial growth with overall body growth and other indicators that have been chosen.4–6 Because of this state of inaccuracy, the clinician should use as many indicators as possible (personal growth history, skeletal growth maturation, and onset of menarche) to make an educated decision about whether the child is growing at an acceptable rate. Girls tend to enter the adolescent growth spurt as defined by obvious somatic growth at around 10 years and boys at around 12 years.
The second assumption made when growth modification is undertaken is that the practitioner can accurately diagnose the source of the skeletal discrepancy and then design treatment that will apply the appropriate amount and direction of force to correct the discrepancy. Diagnosis is not an exact science and may be confusing even with the use of cephalometric measures,7 and the discrepancy may be due to a number of small skeletal problems rather than to one easily identified discrepancy. It is important to remember that not all class II or class III malocclusions are created equal or have only one skeletal feature at fault. Force delivery to dental and skeletal structures also is inexact, and the clinical impression and treatment response may dictate alteration in the amount and direction of force applied to modify growth. Certainly orthodontic treatment for skeletal problems is not just a “see it” and “fix it” situation.
Alternatively, growth modification may work by accelerating the desired growth but not changing the ultimate size or shape of the jaw. A deficient mandible may not end up larger than it ultimately would have been, but it may achieve its final size sooner. This requires the clinician to make some final dentoalveolar changes or compensations to establish an ideal occlusion following growth modification. This type of growth modification response also shows large individual variability. There is support for this interpretation of growth modification based on recent randomized clinical trials that demonstrate little difference between an early- and a late-treatment group of patients with skeletal class II malocclusion.8
Growth Modification Applied to Anteroposterior Problems
Class II Maxillary Protrusion
Class II maxillary protrusion is best managed by headgear therapy to restrict or redirect maxillary growth on the basis of retrospective studies and randomized clinical trials.8,9 Headgear places a distal force on the maxillary dentition and the maxilla (Figure 35-1). Theoretically, the relative movement of dental and skeletal structures depends on the amount and time of force application. In actual practice, it is probably not possible to move selectively only teeth or bones.9 Generally, skeletal and tooth movement are greater with higher forces, but tooth movement can occur with either heavy or light forces. The best approach is probably to apply forces ranging from 12 to 16 ounces per side for 12 to 14 hours and then monitor the skeletal and dental changes and adjust accordingly. Certainly, the skeletal and dental response varies according to the type of headgear chosen and the resultant direction of force exerted by the headgear. The most common varieties, cervical and high pull, provide predominantly distal and occlusal and distal and apical forces, respectively. Traditionally, one avoids using a headgear that tends to extrude posterior teeth in a person with a long face or a limited overbite. On the other hand, a headgear that extrudes the molars is often useful in a patient with a short face and a deep bite.
Class II maxillary protrusion can also be managed with a removable functional appliance of the activator, bionator, or twin block type (Figure 35-2). Although a functional appliance is primarily designed to stimulate mandibular growth, studies have indicated that it has some secondary effects of restricting forward maxillary skeletal and dental movement.8,10,11 This happens because the mandible, which is postured forward, tends to return to a more distal position as a result of the distal muscle and soft tissue forces that are also transmitted through the appliance to the maxilla and the maxillary teeth. The maxillary teeth tend to tip lingually rather than to move bodily, and the mandibular teeth tip facially.
Another functional appliance is the Herbst appliance, which is a fixed appliance used to reposition the mandible forward. It is held in place with bands, stainless steel crowns, bonding, or a cemented cast framework (Figure 35-3). A pin and tube apparatus forces the mandible forward and places constant force on the maxilla and maxillary and mandibular teeth as the mandible attempts to return to a normal and more distal posture. Maxillary teeth tend to move distally and mandibular anterior teeth move forward. This appliance has shown changes similar to those of functional appliances in randomized clinical trials.11
Class II Mandibular Deficiency
The mandibular-deficient patient is usually treated with a removable or fixed functional appliance that positions the mandible forward in an attempt to stimulate or accelerate mandibular growth. Retrospective clinical studies have shown that these appliances can produce a small average increase in mandibular projection (2 to 4 mm/year).12,13 This has been confirmed by randomized clinical trials.8,14 Patient response varies greatly, and in many cases the increased growth does not totally correct the class II skeletal problem for several reasons. First, the amount of growth is not enough to overcome the discrepancy. Second, all the available growth would have to be specifically directed to produce anteroposterior change. This is usually not the case because some dental eruption and vertical growth occurs. This interaction between anteroposterior and vertical dimensional changes decreases ultimate mandibular projection and class II correction because the mandible grows downward and forward and not straightforward. The rest of the anteroposterior discrepancy is managed by restricting maxillary growth, tipping the maxillary teeth back, and tipping the mandibular teeth forward. Different appliances can be designed that exaggerate the secondary responses of maxillary restriction and dental movement if desired. The Herbst appliance, mentioned previously, also has been used with mandibular-deficient patients. Some studies also indicate that headgear treatment may cause an increase in mandibular growth.14,15
Class III Maxillary Deficiency
True midface deficiency can be treated by using a reverse-pull headgear or facemask to exert anteriorly directed force on the maxilla (Figure 35-4).16 The facemask applies force to the maxilla through an appliance (either a removable splint or fixed appliance) attached to the teeth; tooth movement also occurs. Some clinicians also use the facemask with maxillary expansion (either rapid or slow) in an effort to enhance the transverse coordination of the arches or to facilitate anterior movement of the maxilla due to alteration of the bony interfaces with other skeletal structures. A comparison of clinical studies found that less maxillary incisor movement occurs when expansion accompanies protraction.17 One prospective study found no difference between the expansion and nonexpansion approaches.18
Another approach is to use a facemask with miniplates attached to the maxilla. This method can be used in the late mixed dentition, probably at about 10 to 11 years of age, and shows greater skeletal change and movement in the zygomatic area as well.19 Finally, miniplates can be attached to the maxilla and mandible, and intraoral elastics can be used at around the same age. This has the effect of substantial change and no need for an extraoral appliance, which means the elastic force can be used continuously.20
Timing of this treatment has been controversial. Some authors believe that the ideal time to attempt this treatment is soon after eruption of the permanent incisors, whereas others have waited a bit longer. Clearly, postpubertal treatment is not indicated for growth modification.21 Data indicate that there is little anteroposterior difference in treatment effect whether treatment is applied early or late, as long as the treatment is completed before 10 to 11 years of age.22,23 Unfortunately, the long-term success of maxillary protraction is not clear. One fact appears to be emerging: mistaken diagnosis or treatment in patients whose class III malocclusion is the result of mandibular protrusion will usually fail. But, even with those who are correctly diagnosed, one in four will require additional treatment to correct the skeletal malocclusion.24
Class III Mandibular Protrusion
Class III mandibular protrusion has been historically managed with chin cup therapy (Figure 35-5). The theory of chin cup therapy is to apply a distal and superior force through the chin that inhibits or redirects growth at the condyle. Again, studies in animals have shown some change in absolute mandibular size, but clinical application in humans routinely has been less successful.25,26 The typical short-term treatment response to chin cup therapy is a distal rotation of the mandible and lingual tipping of the lower incisors. Therefore chin cup therapy is well tolerated in patients with mild mandibular protrusion and short to normal vertical proportions. It is contraindicated, however, in a person with a long lower face because the anteroposterior correction would come at the expense of an increased vertical dimension. The long-term results of chin cup therapy indicate that although a transient positive change can occur, the long-term results are difficult to differentiate from those in untreated patients.26 It may be possible that the use of class III elastics to maxillary and mandibular miniplates will prove useful in treating mandibular protrusion, but the short- and long-term data are not clear at this point. Functional appliances designed for the management of class III mandibular excess show the same minor changes as those occurring in class III maxillary deficiency.
Growth Modification Applied to Transverse Problems
The most common transverse problem in the preadolescent is maxillary constriction with a posterior crossbite. Management of maxillary constriction can begin as soon as the problem is discovered if the child is mature enough to accept treatment. Treatment has the potential to eliminate crossbites of the succedaneous teeth, increase arch length, and simplify future diagnostic decisions that can be complicated by functional shifts. Most clinicians agree with the philosophy of early correction if there is a mandibular shift. Generally, it is believed that long-term facial asymmetry attributable to soft tissue enlargement and in some cases mandibular asymmetry can result from untreated mandibular shifts.27 Regardless of philosophy, treatment before adolescence and midpalatal suture bridging is recommended.
Three appliances can be used to correct the constriction, but the appliances are not interchangeable. In Chapter 27, the quad helix and the W arch for management of maxillary constriction are described. The appliances provide both skeletal and dental movement in the 3- to 6-year-old child.28 As the patient gets older, more dental change and less skeletal change occur. This is true because the midpalatal suture, which was open at an early age, has developed bone interdigitation that makes it difficult to separate. More force is required to separate the suture after initial interdigitation of the suture to obtain true skeletal correction than a quad helix or W arch can deliver.
In the older preadolescent patient, in whom there is a chance that the midpalatal suture is closed, an appliance that can deliver large amounts of force is necessary to correct the skeletal constriction.29 Rapid palatal expansion is the term given to the procedure in which an appliance cemented or bonded to the teeth is opened 0.5 mm/day to deliver 2000 to 3000 g of force (Figure 35-6). In the active phase of treatment, there is little dental movement because the periodontal ligament has been hyalinized, which limits dental movement, and the force is transmitted almost entirely to the skeletal structures. During retention, however, the skeletal structures begin to relapse toward the midline. Because the teeth are held rigidly by the appliance, they move relative to the bones. Depending on the amount of expansion needed, active treatment normally takes 10 to 14 days. Another approach to skeletal expansion is slow rather than rapid palatal expansion.30 Essentially the same appliance is used as in rapid palatal expansion, although force levels are calibrated to provide only 900 to 1300 g of force. Coupled with a slower activation rate, slow palatal expansion widens the palate by dental and skeletal movement. Although the final position of the teeth and supporting structures is approximately the same in rapid and slow expansion, proponents of slow expansion maintain that slower expansion is more physiologic and stable. Transverse growth modification also can be accomplished by means of acrylic or wire buccal shields attached to functional appliances or lip bumpers. The buccal shields relieve the teeth and alveolar structures from the resting pressure of the cheek muscles and soft tissues. Transverse expansion of 3 to 5 mm can be achieved, although the changes vary considerably. Whether the movement is dental or skeletal and whether it will remain stable is still in question because there are no controlled experimental studies to provide answers.
Growth Modification Applied to Vertical Problems
Vertical skeletal problems are manifested as long and short facial heights and usually are located below the palatal plane.31 The short-faced person has a reduced mandibular plane angle and undererupted teeth. In the long-faced patient, the mandibular plane angle, lower facial height, and amount of dental eruption are increased in comparison with the patient with a normal face. Vertical skeletal problems can be managed with growth modification techniques, and some can be managed successfully; however, even when the treatment has been successful, maintaining the correction is extremely difficult. The face grows vertically for a long time, and there is a tendency for the original growth pattern and problem to recur.
Vertical Excess
Vertical skeletal excess may be managed with extraoral force or intraoral force. Extraoral force is delivered by means of a high-pull headgear through the maxillary first molars. The force is applied in a superior and distal direction and is designed to inhibit vertical development of the maxilla and eruption of the posterior maxillary teeth32 (Figure 35-7). Because no force is applied to the mandibular teeth, they are free to erupt and compensate for the reduced vertical development in the maxilla. In some cases, this compensatory eruption can eliminate all the positive effects of the high-pull headgear and lead to downward and backward rotation of the mandible instead of forward mandibular projection.
An alternative method for controlling vertical development is to block the eruption of the maxillary and mandibular teeth. A functional appliance can be designed that will force the mandible open to an increased vertical rest position. The force of the mandible attempting to return to its original vertical rest position is transmitted to the maxilla and the teeth in both arches. This results in mandibular growth being directed forward because no dental eruption has occurred to increase the vertical dimension and less increase in lower and total face height33 (Figure 35-8). Temporary anchorage devices (TADs) may prove to be of value in restricting vertical facial development. TADs are small diameter titanium screws placed into cortical bone. They do not osseointegrate so they can be removed after use. TADs provide the clinician with an anchor to apply force to teeth without causing other teeth to move because the screw is located in bone. In theory, the screws should not move, although it appears they do move with force application. In cases of vertical excess, TADs are placed to provide an intrusive force to the maxillary posterior teeth.34 Placing TADs in the mixed dentition patient is more difficult, however, because there are unerupted teeth in the way of insertion and the cortical bone does not hold the implant as well before approximately 12 years of age. Regardless of the means used to manage vertical excess, excellent patient cooperation is necessary because treatment must be continued or retained as long as the patient is growing.
Vertical Deficiency
Vertical skeletal deficiencies can be managed with either headgear or functional appliances, depending on the accompanying anteroposterior relationships. The force vector from the headgear should direct the maxilla distally and extrude the maxillary posterior teeth, which would require cervical pull headgear. Because functional appliances are typically designed to inhibit eruption of upper and lower anterior teeth and promote eruption of the posterior teeth, they can also increase vertical facial height (Figure 35-9). In addition, because there is a component of forward or mesial movement of teeth as they erupt, an astute clinician will encourage lower molar eruption in class II cases (lower molar moves forward into class I) and upper molar eruption in class III cases. As in vertical skeletal excess, the original growth pattern tends to recur until growth is complete, and retention should be designed to prevent this recurrence.
Dental Problems
Space Maintenance
A philosophy for space maintenance and the appliances recommended for the primary dentition are discussed in Chapter 25. The same philosophy and appliances apply to space maintenance in the 6- to 12-year-old age group. However, treatment for early loss of primary teeth in the mixed dentition requires some additional thought and consideration. Loss of posterior teeth in the primary dentition is a nearly universal indication for space maintenance therapy. In the mixed dentition, the timing of permanent tooth eruption, timing of tooth loss, presence of succedaneous teeth, and extent of crowding must also be taken into account.
Potential Alignment and Space Problems
Ectopic Eruption
Problems associated with ectopic eruption of the permanent first molar have been discussed previously in Chapter 30. A 3- to 6-month observation period usually is the best initial therapy if the resorption is not too severe, because there is a possibility that the molar will self-correct spontaneously or “jump” distally and erupt into its normal position (Figure 35-10). Intervention is necessary if the molar is still blocked from erupting at the end of the observation period or if the permanent molar is severely impacted.35 The goal of treatment is to move the ectopically erupting tooth away from the tooth it is resorbing, allow it to erupt, and retain the primary second molar.
If a small amount of movement is needed and little or none of the permanent molar is clinically visible, a piece of 20- to 22-mil brass wire can be passed around the contact between the permanent molar and the primary second molar. The brass wire is tightened every 2 weeks. When the wire is tightened, the periodontal ligament space is compressed and the molar is forced distally until it can slip past the primary molar and erupt (Figure 35-11). In some cases, a steel spring clip separator may be used to dislodge the molar, but only in cases in which there is minimal resorption of the primary molar. It may be difficult to seat the spring if the contact point between the molars is below the cementoenamel junction of the primary molar. Some authors advocate elastomeric separators, but they must be carefully supervised because they may dislodge in an apical direction, causing a periodontal abscess. Some elastomeric separators are not radiopaque and can be difficult to locate in the gingival sulcus.
Another method of moving the permanent molar distally is to band the primary second molar and apply a distal force to the permanent molar through a helical spring or elastomer (Figure 35-12). In fact, a type of band-and-spring appliance can be constructed at chairside using the orthodontic archwire tube on a molar band; the appliance is easily activated intraorally at subsequent appointments. These methods require that the occlusal surface of the permanent molar be visible so that force can be applied to move the tooth distally. A small ledge of resin or a metal button can be bonded to the occlusal surface to serve as the point of force application, or the end of the spring can be bonded directly to the impacted tooth. However, salivary contamination of the occlusal surface sometimes makes bonding a frustrating and difficult procedure. An even more cost-effective technique is to bond a permanent first molar bracket on the primary second molar and a permanent second molar bracket on the permanent first molar; then a self-retained helical spring is constructed between the two teeth to move the permanent first molar distally. This can all be accomplished chairside in a few minutes by a proficient wire bender. Such a band-and-spring appliance should be evaluated every 2 weeks and can work effectively in a short time because of the minimal root development on the permanent molar.
Occasionally, the primary second molar must be removed if the permanent molar has caused extensive resorption of the primary root structure. In these cases, loss of arch length is certain, and some plan of treatment for the impending space deficiency should be considered in advance (Figure 35-13). If there is a congenitally missing second premolar or premolar extraction followed by space closure is being considered because of the crowding, then reduction in arch length by mesial movement of the molars is advantageous. To manage the space after extraction of the primary molar, a distal shoe can be placed to guide eruption of the permanent molar. A distal shoe maintains space but does not regain much space that was lost before the primary molar extraction. An alternative plan is to allow the permanent molar to erupt and then u/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline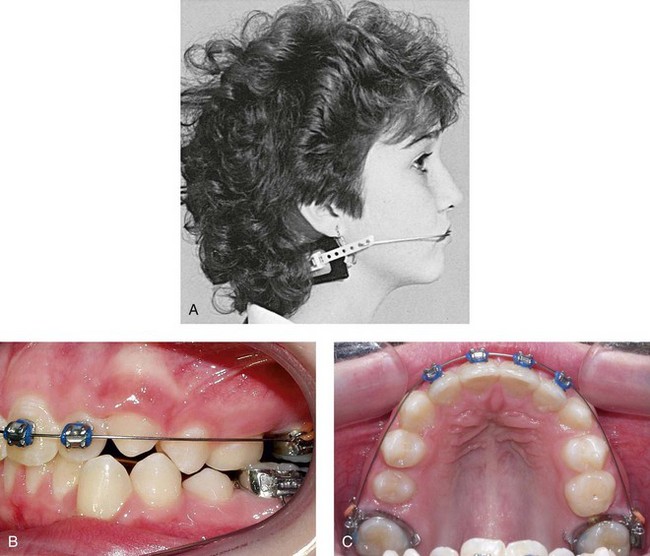
 FIGURE 35-1
FIGURE 35-1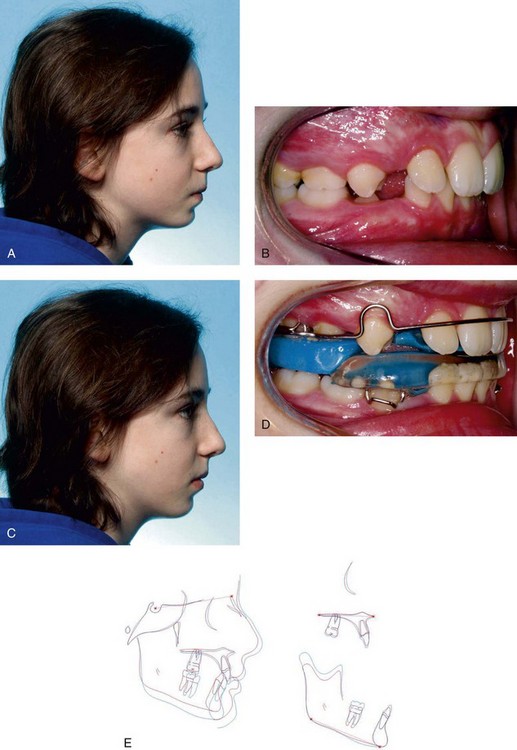
 FIGURE 35-2
FIGURE 35-2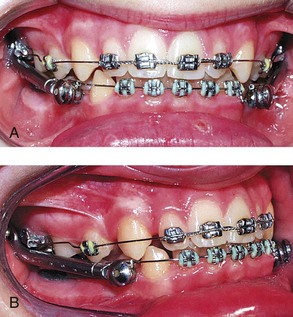
 FIGURE 35-3
FIGURE 35-3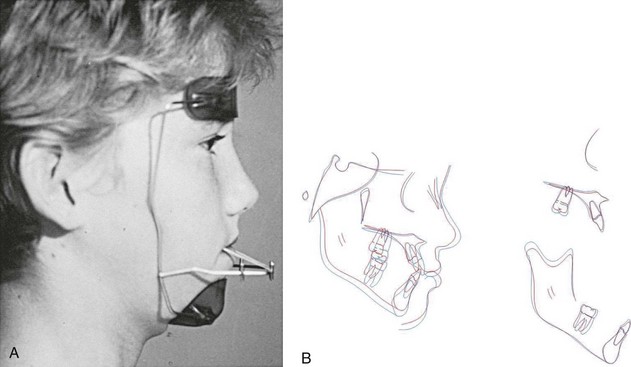
 FIGURE 35-4
FIGURE 35-4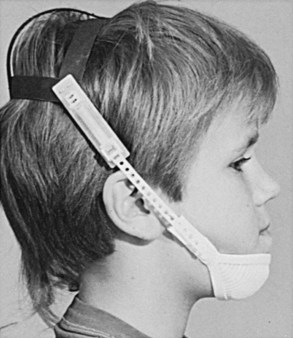
 FIGURE 35-5
FIGURE 35-5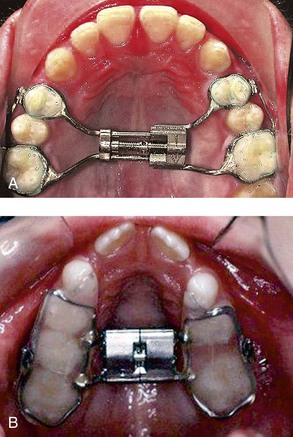
 FIGURE 35-6
FIGURE 35-6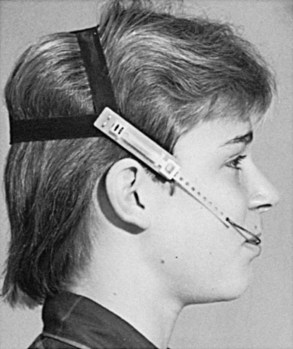
 FIGURE 35-7
FIGURE 35-7
 FIGURE 35-8
FIGURE 35-8
 FIGURE 35-9
FIGURE 35-9
 FIGURE 35-10
FIGURE 35-10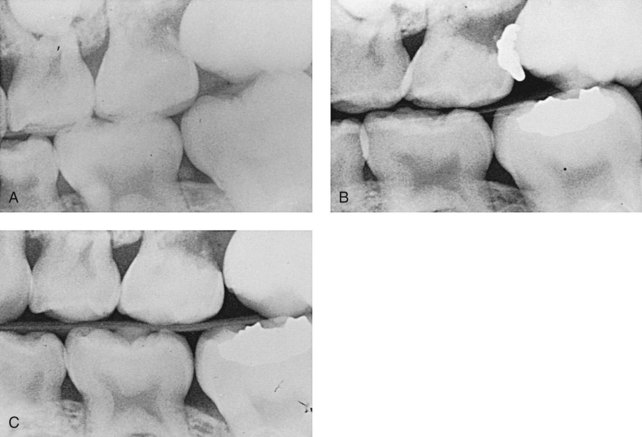
 FIGURE 35-11
FIGURE 35-11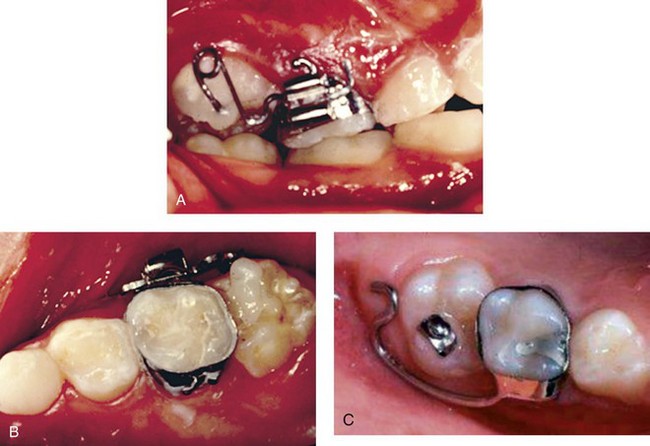
 FIGURE 35-12
FIGURE 35-12