Minimally Invasive Oral and Maxillofacial Surgery Trauma
Endoscopic Treatment of Subcondylar Fractures
Condylar fractures are very common, making up almost one third of all mandibular fractures. There is extensive literature on the management of condylar fractures, which is a subject of significant controversy.1–3 In general, there are three treatment modalities for the management of condylar fractures—observation, closed reduction with some period of maxillomandibular fixation (MMF) and physical therapy; and open reduction and internal fixation (ORIF). Most patients with condylar fractures have a satisfactory outcome measured by mandibular motion with nonoperative management.4 The overall complication rate for treating subcondylar fractures by closed reduction or observation is only near 7%.2 Not surprisingly, the vast majority of condylar fractures are treated in this manner. Anatomic reduction is rarely achieved with this approach, and post-treatment TMJ function is often dependent on adaptation of the altered condylar morphology with physical therapy, neuromuscular training, and guiding elastics.5,6 Nevertheless, there are several instances in which ORIF is the preferred treatment, as described by Zide and Kent7, and later by Haug and Assael8 in their reports regarding indications for the open reduction of condylar fractures. Most agree that significant condylar displacement and ramus height instability are the two main indications to treat subcondylar fractures via an open approach.9 In addition, many surgeons supporting open reduction cite decreased treatment and rehabilitation time, improved anatomic reduction,10 consistent occlusal results,11 and preservation of facial symmetry.12 Furthermore, patients appreciate not having to have their jaws immobilized with MMF.
The topic of open versus closed reduction of subcondylar fractures remains controversial. However, when open reduction has been decided, options include using the submandibular, retromandibular, or preauricular incision. All these approaches allow appropriate access to the subcondylar region, thus enabling proper reduction and fixation. However, these incisions do not come without risks, such as facial scars, intraoperative or postoperative bleeding, salivary fistula, infection, and temporary or permanent facial nerve injury.13–16
With these open approaches, the incidence of facial nerve injury reported is as high as 30%.17 In Ellis et al’s review of the literature, less than 1% of the 455 patients who underwent open treatment of condylar fractures had permanent facial nerve injury, whereas 12% had transient weakness.13 Furthermore, in this series of 93 patients with subcondylar fractures treated open, 17.2% developed temporary facial nerve weakness, with no cases of permanent weakness in patients that followed up. In this same series, 7.5% of patients developed wide or hypertrophic scars postoperatively.
Although rare, the risks for treating subcondylar fractures with standard ORIF are not benign. The benefits of ORIF in treating subcondylar fractures often outweigh these risks. Some surgeons have sought to minimize the risks of treating subcondylar fractures further by developing minimally invasive approaches to the ramus condyle unit. With the aim of minimizing the risks in treating subcondylar fractures with ORIF, while still benefiting from the advantages seen in rigid fixation, some surgeons have turned their attention to minimally invasive approaches to the ramus condyle unit.18–20
Treating subcondylar fractures with endoscopy provides the surgeon with excellent visibility, magnifying and illuminating the operative field. A smaller incision and less dissection are needed, resulting in less postoperative swelling, less pain, shorter hospital stay, quicker postoperative recovery, lower risk to the nerve and smaller inconspicuous scars.21–23 Nevertheless, the surgeon must invest a significant amount of time to learn and master these techniques and the cost of equipment is often high.
Both intraoral and extraoral endoscopic approaches have been described for the treatment of subcondylar fractures. Advocates for the intraoral approach cite benefits such as lack of visible scars and low risk of facial nerve injury.24 However, its use is limited for some types of subcondylar fracture, particularly the medially displaced or dislocated fracture.25 The extraoral endoscopic approach has made the treatment of medial overriding and dislocated fractures much easier, with minimal risk for facial nerve injury and a small, 1.5-cm submandibular scar.18 Here we describe the extraoral and intraoral endoscopic approaches for treating subcondylar fractures.
Extraoral Approach
The extraoral approach described here was developed at the Massachusetts General Hospital (MGH) to gain access to the ramus condyle unit (RCU) for a variety of procedures, including vertical ramus osteotomy with rigid fixation for mandibular setback, condylotomy for condylar sag, high condylectomy, condylectomy, costochondral graft reconstruction, coronoidectomy, and open reduction and rigid fixation of subcondylar fractures. The technique used in all minimally invasive ORIF cases at MGH is the extraoral approach described below.18,26
Surgical Technique
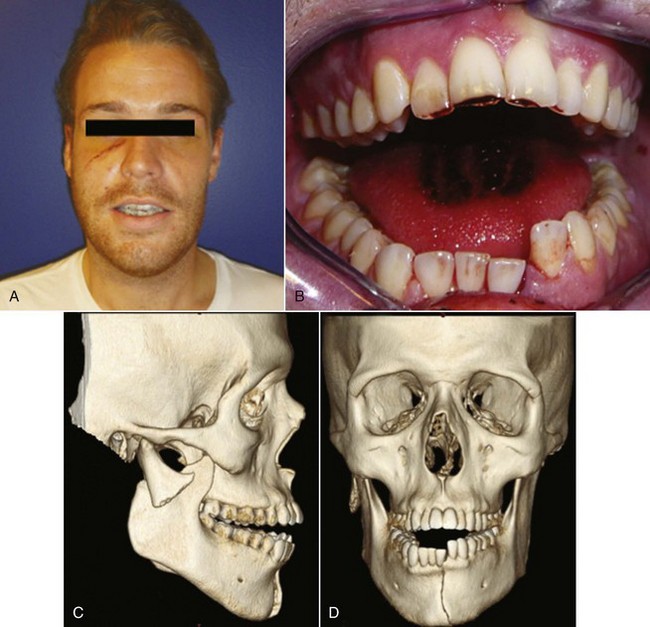
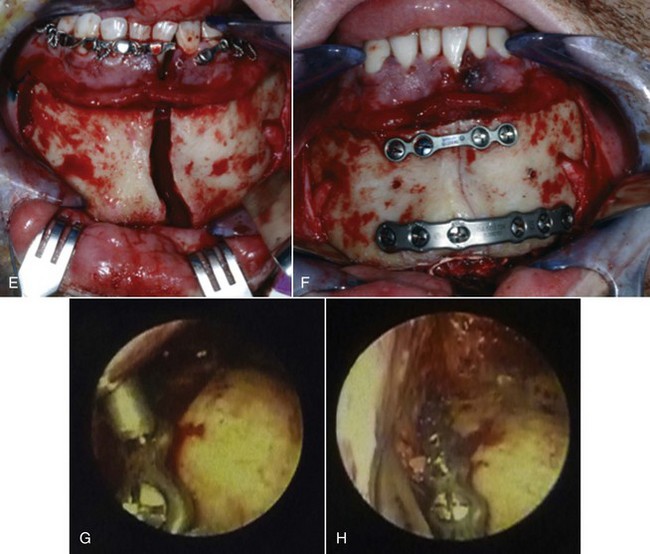
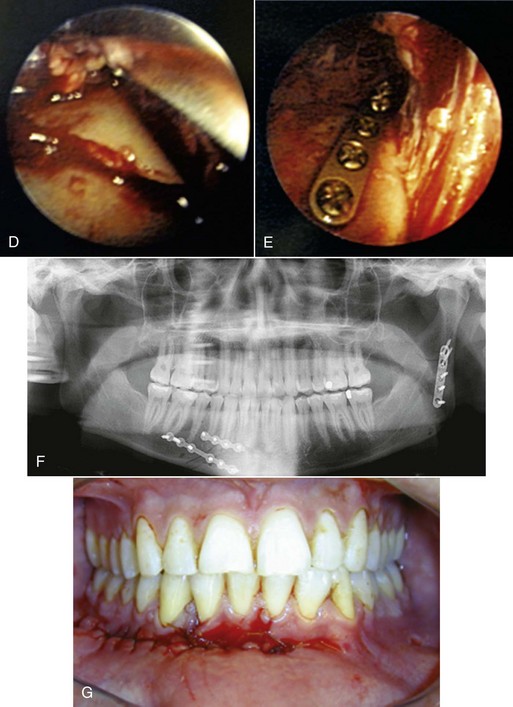
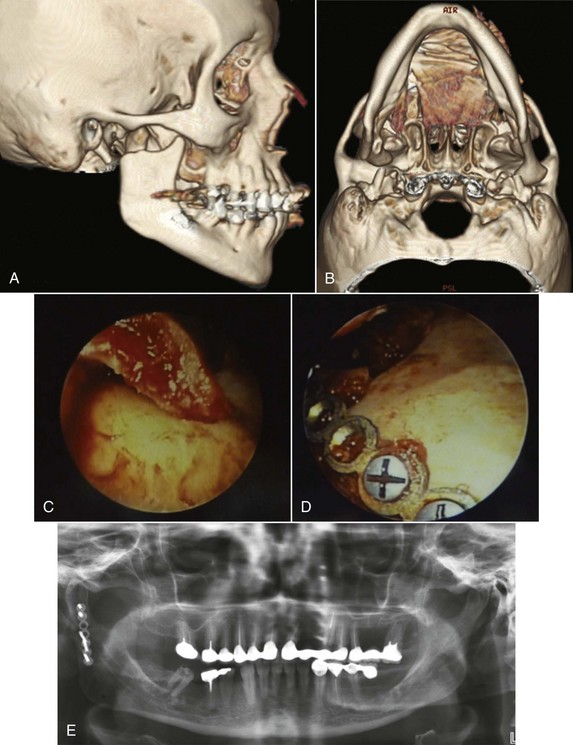
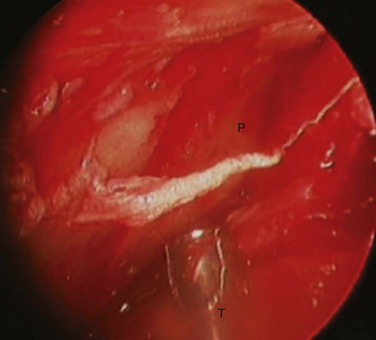
With endoscopic visualization, the proximal and distal fragments of the fracture are identified and mobilized. In the case in which the fracture is laterally overriding, a 24-gauge wire is passed through a 1.5-mm drill hole at the mandibular angle to distract the distal segment inferiorly, enabling the reduction of the fracture. The proximal segment is reduced with the condylar neck head positioned in the glenoid fossa. The fracture is reduced and the distracted distal segment is released, wedging the two segments together. The reduction is verified by directly visualizing the fracture lines at the posterior border and sigmoid notch. The fracture is fixated using a 2.0-mm, five-hole titanium miniplate. The plate may be positioned into place with a plate holder, and screwed to the proximal fragment first, enabling the surgeon then to remove the plate holder and control the proximal fragment while aligning the distal segment for fixation. Reduction at the posterior border is verified and the distal screws are placed, either through the incision or with the aid of a percutaneous trocar (Figs. 34-1 and 34-2).
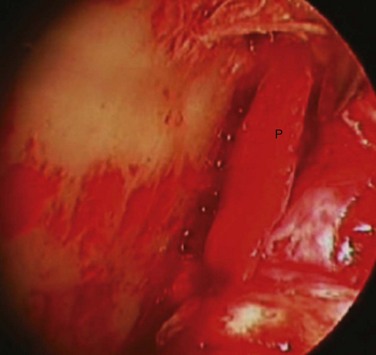
When the proximal segment is medially displaced, an attempt is made endoscopically to visualize the proximal segment, and manipulate it into the lateral overriding position. Typically, this is accomplished endoscopically (Fig. 34-3). If unsuccessful, an endoscopic vertical ramus osteotomy can be performed to permit access to the condylar fragment.22
Outcomes
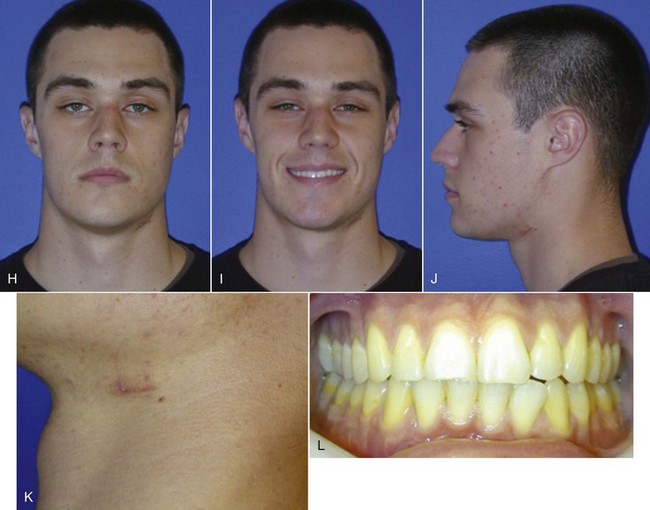
At MGH, in a retrospective analysis of 20 consecutive patients with subcondylar fractures (n = 22 sides) who underwent endoscopic ORIF, 1 patient had temporary marginal mandibular nerve weakness at 1 week follow-up, which resolved several weeks later. There were no permanent postoperative injuries to the marginal mandibular nerve and no unacceptable facial scars were encountered.18,26 In all cases, there were no cases of postoperative malocclusion and all patients had normal TMJ range of motion without pain. Miloro has found similar results in a series of six consecutive subcondylar fractures treated with extraoral endoscopic ORIF.27
Of the 20 patients in the series treated at MGH, 14 were treated initially with endoscopic ORIF and 6 were treated after failed MMF. Of these fractures, 14 were displaced and eight sides were dislocated. Four patients with medial displacement required a vertical ramus osteotomy with subsequent ex vivo removal and fixation of the proximal segment and condyle. In all cases, the RCU heights were restored and there were no abnormalities in healing, facial or trigeminal nerve injury, jaw motion, occlusion, facial asymmetry, or pain. None of the patients required MMF postoperatively and all were discharged from the hospital in less than 23 hours after the procedure.26
Endoscopic Intraoral Approach
Jacobovicz and Lee first described the intraoral endoscopic approach to subcondylar fractures in 1998.28 This approach showed promising results and those who supported it cited benefits such as lack of visible scars and low risk of facial nerve injury. The approach has its limitations, particularly for the management of medially displaced subcondylar fractures.29 It has also been shown to be technically challenging, requiring a steep learning curve, even for those experienced in endoscopic oral and maxillofacial surgery.30 Since its initial description, there have been several modifications described with the aim of easing the technical challenges encountered.26,31,32
Surgical Technique
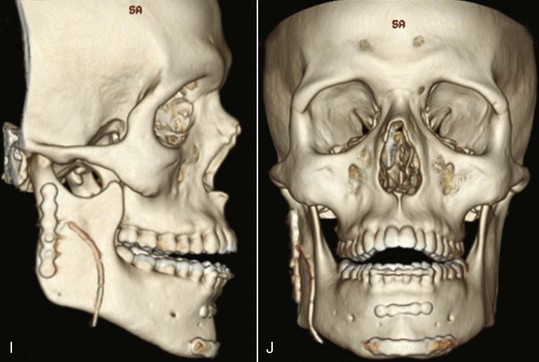
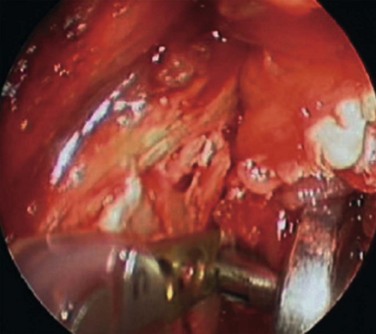
An intraoral incision is made in the posterior mandibular buccal sulcus, with subsequent subperiosteal dissection along the lateral ramus, angle, and posterior border of the mandible, thus creating an optical cavity for a 4-mm, 30-degree angle scope (Karl Storz, Tuttlingen, Germany). A percutaneous, 40-mm guarded trocar is placed transbuccally, perpendicularly at the level of the subcondylar fracture. The optical cavity is maintained by retraction with the guarded trocar, the endoscope is placed through the intraoral incision, and the proximal fragment of the subcondylar fracture is visualized and dissected under direct endoscopic vision (Fig. 34-4).
The patient is then placed into temporary elastic MMF, thus facilitating reduction of the fracture. The proximal segment can be reduced into position by applying a medially directed force against the lateral surface of the proximal segment with the trocar (Fig. 34-5). The anatomic reduction is verified with direct endoscopic visualization and positional screws are placed through the trocar for initial stabilization of the segments. A fixation plate is then used for definitive fixation. The patient is released from MMF postoperatively (Fig. 34-6).
Outcomes
With this technique, the authors confirmed good anatomic reduction, mandibular projection, lower face width, facial height, premorbid occlusion, and a maximal incisal opening of 39 mm without pain. Lee et al followed this with a longitudinal study of 20 patients with 22 fractures that were repaired using this technique.33 Functionally, all patients had restoration of their premorbid occlusion and an average maximal incisal opening of 43 ± 6 mm at 8 weeks postoperatively. All patients were pleased with the aesthetic results of the repair, including chin projection, jaw line, and symmetry; 21 of the 22 fractures showed radiographic evidence of fracture reduction. One patient with medial override showed an improved but imperfect reduction and there was no evidence of late condylar remodeling in any of the patients.
Operative times were also measured. Fractures with lateral override (20 of 22) were easily reduced and fixated endoscopically (131 ± 39 min). Medial override fractures (2 of 22) were challenging to repair and required a much longer operative time (269 ± 139 minutes)33.
Since 1998, there have been several reports describing modifications of the intraoral endoscopic subcondylar fracture repair. Sandler used two separate trocars for improved reduction and fixation.34 The first trocar was placed 20 mm anterior to the tragus along the canthal-tragal line and the second was placed 10 mm below the first site. In 2002, Schon et al used angulated drills and scr/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses