Reconstruction of Avulsive Defects of the Maxillofacial Complex
Causes of Avulsive Injuries of the Maxillofacial Complex
Assessment and Initial Medical Management
Initial Surgical Management of Avulsive Maxillofacial Injuries
Reconstruction of Avulsive Soft Tissue Injuries
Adjunctive Therapy for Complete and Partial Soft Tissue
Avulsions of the Maxillofacial Region
Reconstruction of Avulsive Hard Tissue Injuries
Small Mandibular Defects Requiring No Cutaneous or Mucosal Grafting
Large Mandibular Defects and/or Those Requiring Soft Tissue Coverage
Trauma, including unintentional and violent injury, remains the leading cause of death and disability in the United States for individuals from the age of 1 year to the mid-40s (Fig. 31-1).1 Arguably, no other physical deformity is as psychologically devastating as a traumatic defect to the face, exceeded only by those defects involving avulsive loss of hard and soft tissue.2 Although the art and science of prosthetic limb replacement has advanced tremendously during the past 2 decades, with current research investigating true brain-machine integration, no satisfactory component has been developed to serve as a replacement for the facial unit.3,4 Imagine an individual living a normal life, such as eating in a restaurant, shopping, or sitting at the local coffee house while using their laptop computer to browse the Internet. And, in one cruel twist of fate, the focal point of their self-image, and the source of their engagement with society, is permanently mutilated. Avulsed hard and soft facial tissues leave enormous psychological, interpersonal, functional, and physical disabilities, well beyond those encountered by those with congenital deformities or traumatic amputation of the extremities; integration back into society is slightly easier if you have never known life without your congenital defect, or your lower extremity amputation has been replaced by a state of the art prosthetic limb. The comprehensive management of avulsive facial injuries rarely has been the focus of any epidemiologic, demographic, or other therapeutic studies. A complete review of the potential treatment modalities, soft and hard tissue reconstruction options, and management principles of avulsive hard and soft tissue wounds to the craniomaxillofacial unit is beyond the scope of this chapter, and would take volumes of data and literature to address the topic adequately. Instead, the focus here is to provide the practicing facial trauma surgeon with an overview of the causes, incidence, diagnosis, classification, and surgical management of these devastating injuries.
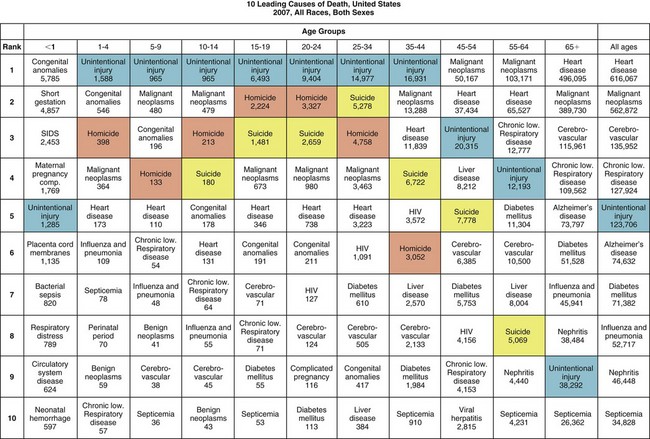
FIGURE 31-1 Statistics for leading causes of death in the United States, 2007. (From National Center for Injury Prevention and Control: WISQARS leading causes of death reports, 1999-2007, 2010 [http://webappa.cdc.gov/sasweb/ncipc/leadcaus10.html].)
Causes of Avulsive Injuries of the Maxillofacial Complex
The description of injury can be summarized simply as the effects of energy overcoming inertia. Our study of physics, and the work of Sir Isaac Newton, has shown that the velocity of a body remains constant unless the body is acted on by an external force. To quote Haug, “In the case of maxillofacial trauma, the object is the specific maxillofacial body part, and kinetic energy is provided by the wounding agent, either bullet, bludgeon, or motor vehicle.5 When considering avulsive defects of the maxillofacial complex, a sufficient quantity of energy must be delivered to the body part to remove it from its native bed. Kinetic energy (KE) is related as  mv2 (where m = mass and v = velocity), but Cunningham has hypothesized that softer tissues, such as brain and muscle, are associated with a lower exponent of injury (0.5) than harder tissues, such as bone, which would have a higher exponent (2.5) and therefore a higher likelihood of permanent injury. Thus, the corrected formula for estimating wounding capacity by kinetic energy would be as follows:
mv2 (where m = mass and v = velocity), but Cunningham has hypothesized that softer tissues, such as brain and muscle, are associated with a lower exponent of injury (0.5) than harder tissues, such as bone, which would have a higher exponent (2.5) and therefore a higher likelihood of permanent injury. Thus, the corrected formula for estimating wounding capacity by kinetic energy would be as follows:
depending on the location of the trauma.6
Firearm Injuries
Firearm injuries have been described in detail in another chapter of this text and are acknowledged as possibly the most common source of avulsive tissue loss of the craniomaxillofacial components currently seen by facial trauma specialists. Whether sustained as a the result of self-inflicted wound, accidental hunting or recreational incident, criminal activity, or of military or professional service to the community, high-energy avulsive ballistic wounds present a vexing treatment dilemma to restore form, function, and cosmesis adequately to the facial unit.6–8
Occupational and Farm Injuries
Industrial or agricultural accidents possess the potential to create severe crush or avulsive wounds of the soft and hard tissues of the maxillofacial complex. Whether low or high velocity, the sheer mass of the injury platform associated with industrial machinery create tissue injury patterns characteristics of a high-energy impact.9–11 As seen in firearm and ballistic injuries, if the injury pattern is consistent with a high-energy impact, the degree of tissue disruption occurring in the hard and/or soft tissues may result in separation from the native tissue bed and avulsion. If the wounding mechanism is a crush injury, the soft tissue overlying the bone can sustain catastrophic compromise to the vascular pedicle, resulting in soft and/or hard tissue necrosis. This necrosis, resulting in partial loss of tissue or the physical structure or complete loss of the anatomic component, has the same physical outcome as avulsion.
Tearing Injuries
Shearing or cutting injuries created by blades or saws, tearing wounds caused by industrial machinery, and bites inflicted by animals are capable of creating avulsive defects and contaminated crush injuries of the craniomaxillofacial unit.12–16 Whereas large domestic animals can bite with forces as great as 450 lb/inch, animals in the wild, such as bears or jaguars, can have bite forces in excess of 1700 lb/inch2,17 (Fig. 31-2). This form of crush injury can be contaminated by a wide range of microorganisms, including viruses, bacteria, and mycobacteria. Significant areas of soft tissue overlying the facial skeleton may be avulsed, crushed, or bruised, compromising vascular supply and delaying initiation of the body’s host defense mechanism. Gross contaminants on machinery parts, including industrial residue and/or microbial sources from many sites of origin, serve as infectious reservoirs, further complicating the normal healing cascade.
Abrasion Injuries
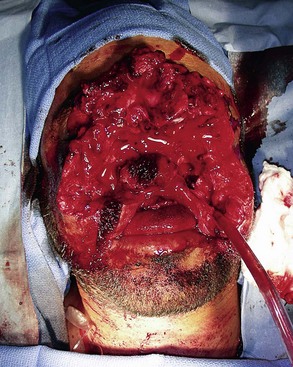
Abrasion injuries are another source of avulsive tissue loss in the craniomaxillofacial region, which have the potential to create horrific defects. Although relatively unusual for a victim to be actively dragged by a moving object, when it does occur, as seen in a motor vehicle accident (MVA) or a motorcyclist sliding along the road, the overlying soft tissues will bear the brunt of the injury18–20 (Fig. 31-3). Protruding anatomic structures, skin, muscles, and neurovascular components will be lost before the bone is potentially injured or avulsed. The result is an injury that is grossly contaminated and devoid of any healthy soft tissue for local flap reconstruction, and that will require adjacent tissue recruitment or remote transfer for adequate rehabilitation.21
Incidence
Historically underreported in the craniomaxillofacial trauma literature, or noted primarily in case reports from periods of military conflict, avulsive defects to the maxillofacial region have been recognized to occur infrequently and are perceived to have a poor prognosis in regard to an acceptable cosmetic and functional repair.5,20,21–30 In the civilian literature, the decade-long experiences of Clark et al at one of the busiest and premier level I trauma centers in the United States, have identified approximately 1.5 cases/year of avulsive tissue loss to the craniomaxillofacial region.24 Considering the reported volume of over 6700 unique trauma patient identifiers at the shock trauma center annually, the relative infrequency of this occurrence becomes apparent.31 Clark et al noted that approximately 46.6% of these injuries involve the mandible, maxilla, and orbit; 26.6% involve the mandible and maxilla; and 26.6% involve the mandible alone. Haug et al have reported a 1% occurrence of avulsive maxillofacial injuries (5 of 475patients) during a review of experiences at a civilian trauma center in Cleveland, with most cases involving self-inflicted gunshot wounds with shotguns in a suicide attempt.27 In a survey of over 9400 patients treated during the Vietnam conflict, Osbon had previously noted that 9.4% exhibit an avulsion of a notable portion of their mandible.25 Because Vietnam represented the first armed modern conflict against nonconventional military forces, the avulsive loss of mandibular anatomy was not previously experienced to the degree as seen in this conflict.29 Dobson outlined classic forms of warfare to include: minor conventional warfare, major conventional warfare, rural attack, and terrorist attack.32
Rural attacks, minor conventional warfare, and major conventional warfare displayed remarkably similar historical incidences of head and neck injury, with 16%, 16%, and 15% for British, Commonwealth, and military personnel, respectively, since 1914. Terrorist attacks, however, displayed a statistically higher incidence of 21%. In the only known paper published during Operation Iraqi Freedom–Operation Enduring Freedom (OIF-OEF) with reported battlefield conditions consistent with classic military combat, Montgomery et al noted the incidence of head and neck casualties as 25% for U.S. military personnel, which is consistent with the previously reported historic norms for U.S. conflicts.33 Dobson et al32 have described terrorist attacks as highlighted by the unconventional use of improvised explosive devices (IEDs), which correlates with the injury pattern of the IED as used by insurgents in OIF-OEF. Most hard tissue facial injuries were sustained in the mandible due to its prominence from the facial skeleton. This was also noted in Lew et al’s study of maxillomandibular fixation (MMF) and open reduction and internal fixation (ORIF) of mandible fractures being the second and fourth most commonly reported surgical procedures.29 The placement of IEDs, usually well below the level of the head and neck, would obviously place the anterior-inferior aspect of the mandible at increased risk as the explosive force and associated shrapnel would proceed in a superior vector, striking the lower face. Modern body armor plays a significant role in the overall survivability of wounded military personnel, but Dobson et al’s observations offer a unique perspective and potential additional cause for the increased craniomaxillofacial injuries seen in OIF-OEF.
Assessment and Initial Medical Management
Obviously, avulsive injuries to the craniomaxillofacial complex are potentially life-threatening (Fig. 31-4). Compromise of the airway through anatomic collapse, hemorrhage, foreign body obstruction, or aspiration are acknowledged as known risks, requiring immediate intervention to provide for continued oxygenation of the patient. As prescribed in the current Advanced Trauma Life Support (ATLS) protocols, securing the airway definitively should be accomplished by conventional oral or nasal endotracheal intubation, intubation of a visible component of a traumatically exposed trachea, or cricothyroidotomy or surgical tracheostomy.21 After the airway has been established, attention should be directed to a thorough analysis of the patient for potentially lethal injuries and appropriate interventions initiated. Control of hemorrhage should be established with simple pressure to the site by compression dressings or manual palpation, ligation of visible sources of active bleeding, or use of hemostatic dressings impregnated with components such as chitosan or similar compounds.33 Injuries to the deep vessels of the head or neck, or those not visible from routine surgical access, may require interventional approaches to gain control of the hemorrhage.34 During the course of fluid resuscitation, particular attention should be paid to the head and neck region because seemingly benign scalp lacerations, or those not recognized due to lack of hemorrhage secondary to hypovolemia, have been associated with exsanguinating hemorrhage as the patient’s mean arterial pressure is increased.35 If the head and neck region is covered under surgical drapes due to ongoing therapy in other areas of the body, this unrecognized source of bleeding can confound anesthesia providers and surgeons, or potentially be lethal.
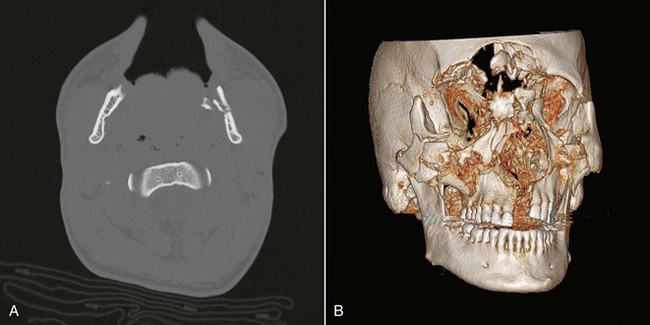
After all life-threatening injuries have been recognized and successfully managed, identification of the avulsive facial defects can be accomplished. Computed tomography (CT) scans with three-dimensional reconstruction are the minimum baseline studies required for the treatment planning of avulsive craniomaxillofacial defects (Fig. 31-5). Most avulsive soft tissue injuries, and all avulsive hard tissue injuries, will be definitively treated in an operating room environment. After stabilization, medical management should commence with appropriate early nutritional and psychiatric support for the patient, with antibiotic therapy directed toward cutaneous, oral, pharyngeal, nasal, and sinus contaminants.33,36 Because these wounds are typically contaminated, and may exhibit vascular compromise, consideration should be given to the administration of the appropriate tetanus prophylaxis (Table 31-1) and, in the case of animal bites, rabies prophylaxis (Fig. 31-6).
TABLE 31-1
Rabies Postexposure Prophylaxis (PEP) Schedule
| Vaccination Status | Intervention | Regimen* |
| Not previously vaccinated | Wound cleansing | PEP should begin with immediate thorough cleansing of all wounds with soap and water. If available, a virucidal agent (e.g., providine-iodine solution) should be used to irrigate the wounds. |
| Human rabies immune globulin (HRIG) | Administer 20 IU/kg body weight. If anatomically feasible, the full dose should be infiltrated around and into the wound(s), and any remaining volume should be administered at an anatomic site (IM) distant from vaccination administration. Also, HRIG should not be administered in the same syringe as vaccine. Because HRIG might partially suppress active production of rabies virus antibody, no more than the recommended dose should be administered. | |
| Vaccine | Human diploid cell vaccine (HDCV) or purified chick embryo cell vaccine (PCECV) 1.9 mL, IM (deltoid area†), one each on days 0,‡ 3, 7, and 14§ | |
| Previously vaccinated¶ | Wound cleansing | PEP should begin with immediate thorough cleansing of all wounds with soap and water. If available, a virucidal agent (e.g., providine-iodine solution) should be used to irrigate the wounds. |
| HRIG | HRIG should not be administered. | |
| Vaccine | HDCV or PCECV, 1.0 mL (deltoid area†), one each on days 0‡ and 3. |
*These regimens are applicable for persons in all age groups, including children.
†The deltoid area is the only acceptable site of vaccination for adults and older children. For younger children, the outer aspect of the thigh may be used. Vaccine should never be administered in the gluteal area.
‡Day 0 is the day that dose 1 of vaccine is administered.
§For persons with immunosuppression, rabies PEP should be administered, using all five doses of vaccine on days 0, 3, 7, 14, and 28.
¶Any person with a history of preexposure vaccination with HDCV, PCECV, or rabies vaccine absorbed (RVA); prior to PEP with HDCV, PCECV or RVA; or previous vaccination with any other types of rabies vaccine and a documented history of antibody response to the prior vaccination.
Adapted from (Centers for Disease Control and Prevention: ACIP recommendations: Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies, 2011[http://www.cdc.gov/rabies/resources/acip_recommendations.html]).
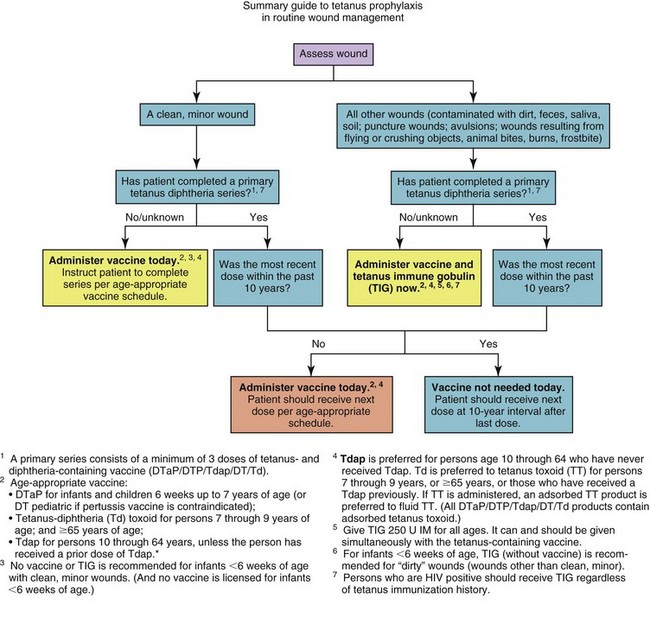
FIGURE 31-6 Summary guide to tetanus prophylaxis in routine wound management. (Centers for Disease Control and Prevention: ACIP recommendations: Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies, 2011[http://www.cdc. gov/rabies/resources/acip_recommendations.html]).
Classification
Avulsive Soft Tissue Maxillofacial Injuries
Avulsive injuries of the soft tissue of the craniomaxillofacial region should be classified as either complete avulsion or partial avulsion. Complete avulsion should be defined as an injury in which there is complete loss or detachment of a portion of the craniomaxillofacial structures, without the ability to regenerate the missing anatomic entity (Fig. 31-7). The ability to regenerate the missing component is directly related to the magnitude of the avulsion and the vascular status of the remaining soft tissue bed. A partial avulsion is defined as one in which the segment is still attached to the remaining native tissue bed, but presents with obvious concerns for viability (Fig. 31-8). The same classification holds true for scalp injuries. Complete avulsion would be one in which a portion of the scalp is lost and the magnitude of the loss is significant enough to prevent complete regeneration from the surrounding soft tissue bed (Fig. 31-9). A partial avulsion would be one in which loss of the scalp has occurred, with resultant vascular compromise, with or without the necessity for tissue replacement.
Avulsive Hard Tissue Maxillofacial Injuries
Currently, no universal classification system exists for avulsive defects of the craniomaxillofacial complex. The injuries are usually described in anatomic terms, such as mandibular, midfacial and/or upper facial third, or full thickness or partial thickness for skin, or by the wounding mechanism (e.g., low energy, thermal, high energy).27,28 With the advent of composite facial allografts, and the various descriptions used by the transplant community to describe these surgeries, a uniform system for the description of avulsive loss of craniomaxillofacial components will likely be forthcoming in the near future.37–40
Initial Surgical Management of Avulsive Maxillofacial Injuries
1. Secure a definitive airway.
3. Explore and identify remaining native tissue and documentation of avulsed components.
4. Identify, document, and primarily repair, if possible, the presence of significant soft tissue injuries:
5. Salvage and maintain remaining hard and soft tissues.
6. Establish anatomic landmarks and an osseous foundation for definitive reconstruction.
7. Prevent infection and subsequent exacerbation of soft tissue contracture.
Because of the likely multitude of surgical interventions and concurrent soft tissue edema that the patient will experience, not only due to the primary injury but as a tissue response to initial and subsequent fluid resuscitations, strong consideration should be given to performing an elective surgical tracheostomy if not done previously. Wound exploration for transected vessels should be performed with identification and definitive control established through ligation or cautery. Efforts should be directed to preservation of all hard and soft tissues, including those with questionable vitality, because they may be able to be preserved or surgically reattached through conventional or microsurgical techniques. Soft tissue is generally repaired from inside-out, with stable reapproximation of the deep tissues. Identification of clinically significant soft tissue injuries, including transection of the facial nerve or salivary ducts, should be performed under magnification with surgical loupes or microscope, and primary repair attempted, if feasible. The recognition of facial nerve injury is a critical finding for the rehabilitation of the patient because the determination for facial reanimation surgery and the timing for repair options have a finite period for intervention.41,42 Hard tissue repair can be accomplished by beginning with the mandible and reestablishment of the occlusion, followed by the midface and upper facial third. The frame of the midface and upper face should be established from the supraorbital bar, lateral orbital rims, malar buttresses, and arch projection first, followed by the central midface of the naso-orbital-ethmoid (NOE) region, with final corrections of the dentoalveolar unit at the Le Fort I level accomplished last. Although the mandible-first protocol generally is applied most often, if the midface or upper facial third is minimally injured, and a more accurate reconstruction for the surgical foundation can be accomplished in those areas, reconstruction should commence in those regions.
After this primary surgery, the patient should undergo a complete CT imaging survey to evaluate anatomic reduction or fixation, better identify tissue loss, and assist with treatment planning for an early reconstruction. As described by Powers and Robertson and others, the patient will likely require frequent returns to the operating room at 2- to 3-day intervals to control infection, decontaminate and/or débride necrotic tissue, and reassess vitality in the remaining tissues.33,43 Good mucosal coverage with adequate vascularity of the osseous structures internally, and similar cutaneous coverage externally, will help prevent infection and mitigate hard tissue necrosis.
Reconstruction of Avulsive Soft Tissue Injuries
Initial determinations of reconstructive options for avulsive soft tissue injuries are aligned under the decision to proceed with prosthetic reconstruction, or native soft tissue utilization. As previously described by Haug and Carlson, the necessity for adjunctive therapy of native soft tissue rehabilitation is determined by the following parameters: temperature, color, oximetry, and capillary refill.5
Ear Avulsions
Débridement of the wound begins the process of repair in treating complete and partial avulsions of the ear. The concept of débridement is well established in the literature and is a critical component in the management of avulsive injuries to the craniomaxillofacial complex.33,43 Serial washouts and débridement of tissue have become mainstays for craniomaxillofacial trauma surgeons in the treatment of these injuries. Unfortunately for many surgeons, the term débridement is synonymous with the absolute removal of tissue in the operating room. Although devitalized necrotic tissue does require excision, a more accurate definition of the goal of serial washouts should be the term decontamination. Preservation of all viable tissues is a critical component in the management of gunshot wounds to the maxillofacial region. Once tissues are lost, the surgeon is faced with two choices—compromise the anterior-posterior projection to allow for primary closure of native tissue or transfer additional tissue to the region via pedicled or microvascular grafts. Avoidance of the need for tissue transfer should be the goal, and judicious use of the practice of decontamination will assist in achieving the desired results.
Pulsatile jet irrigation with normal saline may be indicated for the débridement of avulsive soft tissue wounds. It is important, however, to prevent iatrogenic trauma with overexuberant use of jet irrigation. In the case of complete avulsion of an ear segment, in which the segment has been salvaged and accompanies the patient to the hospital, the component should be cleansed with antiseptic solution and a salvage procedure attempted with microvascular anastomosis, if possible.44 When microvascular anastomosis of an avulsed segment is not possible, the surgeon may elect to proceed with primary reattachment of the ear and adjunctive use of hyperbaric oxygen or leech therapy to address the resultant venous congestion and vascular concerns.45 If the ear has not been stored or transported in a cool environment, excessive contamination exists, or perceived excessive ischemia time with obvious tissue necrosis is present, the wound may be primarily closed and future reconstruction planned. Partial ear avulsions are those in which the traumatized segment of the ear is still attached but there is questionable vascularity to the partially avulsed segment. Partial ear avulsions should be treated with primary closure of the partially avulsed segment as soon as possible to prevent tissue necrosis and loss.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses