APPROACHES TO TREATMENT OPTION FOUR
OVERDENTURES
An overdenture is a complete or partial removable prosthesis fabricated over and partially supported by one or more retained roots or dental implants.
Types
(i) The teeth are cut flush with the gingivae, the pulp canals sealed and an overlying denture made (Fig 31-1a).
(ii) The teeth are cut, leaving supragingival stumps with or without the provision of auxiliary devices to assist retention and stability (Figs 31-1c, 2b, 4e, 5g, 6q).
(iii) As in (ii), but with osseointegrated fixtures acting as the supragingival stump (Fig 31-3a).

Fig. 31-1a (i) Failed bridgework, there was caries of all abutments.
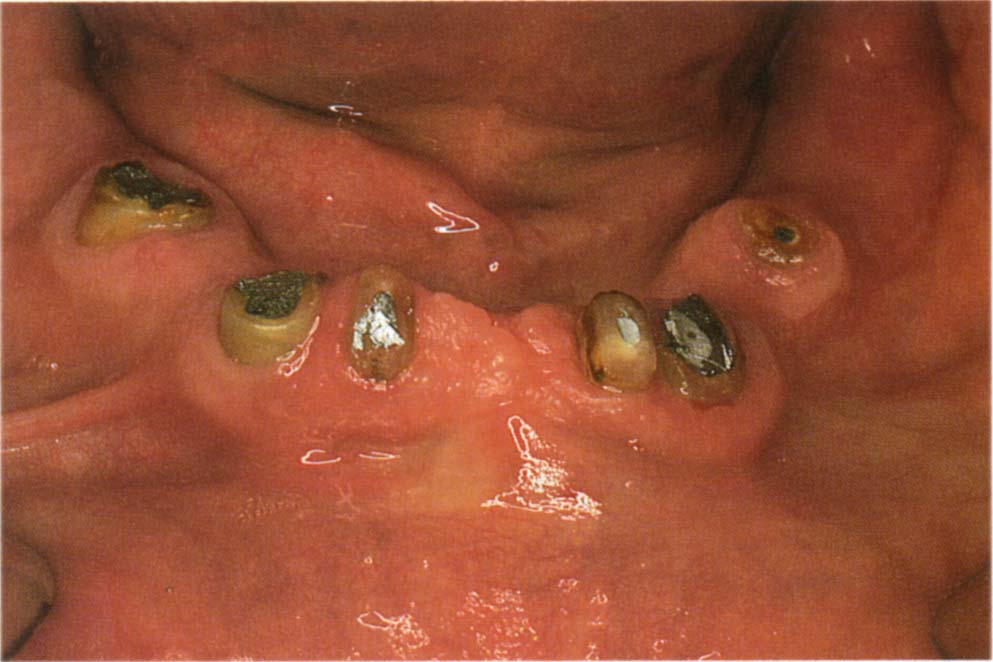
Fig. 31-1a (ii) Teeth cut flush – pulp chamber obturated and overdenture made.
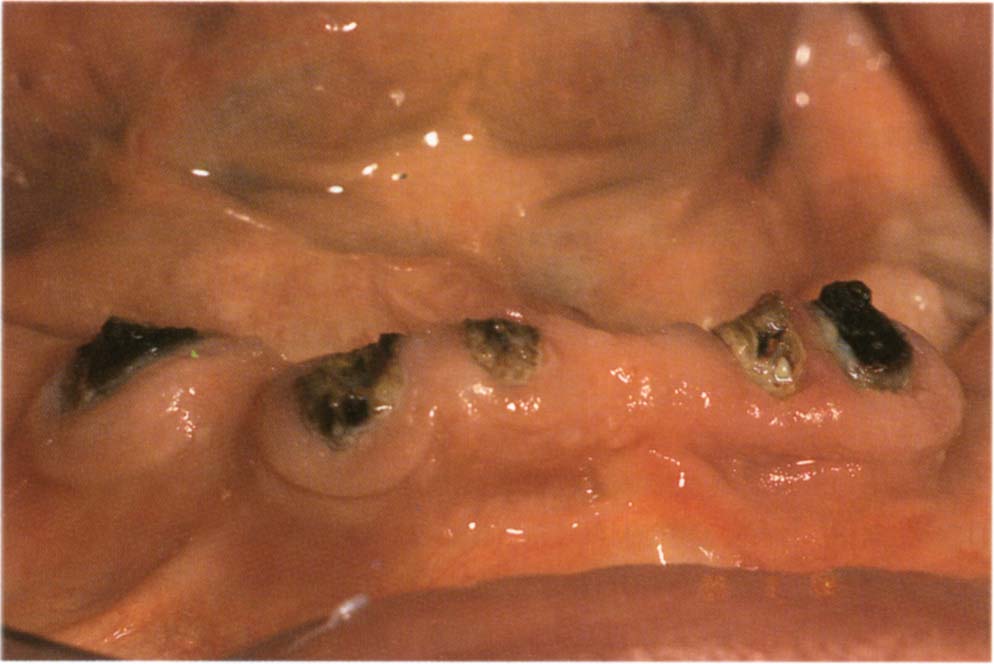
Fig. 31-1b One year following overdenture placement – note the caries.

Fig. 31-1c Supragingival tooth stumps approximately 3 mm high have been retained to give some resistance to lateral forces, carious roots will be extracted. (Different patient from Fig. 31-1b)

Fig. 31-1d Overdenture with spaces to accommodate the roots. The denture is adjusted using pressure relief cream (Kerr or Mizzy) as an indicator so that there is even contact on the saddles when the denture is held firmly to place with the fingers, contact on the top of the root faces, but slight relief around the gingival margins.
Indications
As for the provision of a full or partial denture, but with some salvagable roots or, in the case of osseointegrated fixtures, insufficient number and length of fixtures to support a fixed bridge. Particular indications for an overdenture rather than a fixed bridge are:
- Jaw relationships requiring teeth to be set so far off the ridge that gingival form can only be obtained by using a removable prosthesis.
- Advanced ridge resorption – as above.
- Aesthetic considerations, to give more flexibility in tooth positioning.
- Phonetic considerations, to seal the space that can arise between a fixed bridge and the mucosa or in the embrasures.
- Emergencies, if a bridge required removal, rendering a fixed prosthesis unserviceable.
- Intermediate treatment, whilst deciding if a fixed prosthesis is feasible and justified. Subsequent failure of a fixed bridge inserted under questionable circumstances with conversion to an overdenture may be hard for the patient to accept, whereas conversion of an overdenture to a fixed bridge is more acceptable.
Advantages over Complete Dentures
- Maintenance of bone
- Better retention and stability
- Enhanced proprioception
- Psychological aspects
- Greater chewing power
Maintenance of Bone
The typical edentulous facies associated with old age is ascribed to the loss of alveolar bone, rather than the crowns of the teeth.1 The retention of residual roots2–3 and the presence of osseointegrated fixtures4 reduce over the long-term loss of the residual alveolar bone, thereby improving aesthetics. Furthermore, maintenance of the alveolar ridge enhances denture retention and stability. However, although with mandibular overdentures two osseointegrated fixtures retain bone around the fixtures, the posterior bone, in patients who have been edentulous for less than 10 years, resorbs on average by two to three times that of complete denture wearers.4 This could result from rotation about the anterior bar, leading to increased posterior loading. Minimal posterior resorption occurred in patients with mandibular fixed prostheses which were supported by four to six fixtures. There were no differences in the amount of resorption occurring between the overdenture group and complete denture group, when patients had been edentulous for 10 years or more. Prescription for young patients with mandibular overdentures, supported by two anterior implants, should be cautiously evaluated in relation to posterior bone resorption.
Quirynen et al. (1991)5 reported that maintenance of bone around fixtures, over an observation period of up to four years is beneficial in the mandible, – 0.8 mm bone loss in the first year, followed by less than 0.1 mm per annum thereafter – particularly when the fixtures are joined by a bar, but poor in the maxilla – up to 2 mm – when the fixtures are not connected.
Improved Retention and Stability
Retention is the resistance to vertical forces which dislodge the denture in an occlusal direction. Retained roots and osseointegrated fixtues can be used to enhance retention in two ways:
- Undercuts on the residual root surfaces.
- Auxiliary devices.
Stability is the resistance to non-occlusally directed dislodging forces:
- Vertical forces: forces which dislodge the denture towards the edentulous ridge are resisted if non-mobile roots or osseointegrated fixtures are retained.
- Lateral dislodging forces: these are resisted by supragingival root faces/fixtures, with or without auxiliary devices.
Two important considerations in relation to possible failure of tooth retained overdentures, are:
(i) Failure of the original restorations, due to caries. Auxiliary retention and stability devices should not be used until, and unless the caries is controlled. Figure 31-1a shows root surfaces following provision of an over-denture. Figure 31-1b shows the same root surfaces one year later. Provision of auxiliary devices would have been an expensive and time-consuming affair and without the control of disease, destined to further failure. It is always possible to modify the obturated roots to receive auxiliary devices once the disease has been controlled. Ettinger et al. (1984)6 reported a progressive increase in caries rate up to 20.6% over a five year period for unrestored, unsupervised root abutments. However, in 254 patients recalled at six monthly intervals for maintenance treatment, Ettinger (1988)7 reported an abutment loss of 4.2% over a 12 year period, emphasizing the importance of disease control.
(ii) Failure of the original restorations due to other causes. In these cases, auxiliary devices may be prescribed even when failure is due to advanced periodontitis, provided the roots are not so mobile as to be useless. Indeed, auxiliary devices can be especially helpful, since bone loss associated with the periodontitis may result in relatively flat ridges, making the transition to a conventional complete denture almost impossible, yet the mobility of the abutments acts as a stress breaker.
Whilst many devices have been described for auxiliary retention and stability, it is better to use a small variety to good effect rather than a large variety indifferently. Useful devices are: stud attachments (Fig 31-2), bar and clip attachments (Figs 31-3 to 31-6), bar and clip attachments in conjunction with copings within the denture (Fig 31-6). Both dentist and technician must be knowlegeable in the use of such devices.
Proprioception
It has been reported that the retained roots will enhance proprioception, leading to greater sensation and control of mandibular movements.8–9
Psychological
The transition to complete dentures is often associated with ageing. Often, the patient has striven for many years to maintain fixed bridgework and suddenly, is advised to change from what appears to them to be a full mouth of teeth to a ‘mouthful of dentures’. The thought that some teeth are being kept, albeit beneath a denture, gives a psychological boost to the patient, making the transition more acceptable.
Greater Chewing Power
Rissin et al. (1978)10 reported that overdenture patients have improved masticatory efficiency, compared to complete denture wearers.
Auxiliary Retention Devices
Stud Attachments (Fig 31-2)
For example, Dalbo stud attachment (Cendres et Metaux 31.02.8); Ball Attachment – (Nobelpharma SDCA 115–117, DCA 113, DCB 112, DCA 111) – see Appendix for laboratory details.
A spheroidal attachment (patrix) is soldered to a root face casting, which is usually integral with a post. For osseointegrated fixtures (Nobelpharma), the attachment is screwed into the fixture. A cylindrical device (matrix) within the denture fits over this and, being split, is able to spring over the greatest diameter of the patrix. With a cobalt chromium frame, if space permits, it is advisable to extend small extension ‘fingers’ of chrome over the matrix, distributing compressive forces to the metal rather than confining them to the acrylic. The matrix is adjusted by gently bending the split ‘leaves’ with the special tool provided. A spacer ring can be placed over the root face casting to elevate the matrix, prior to attachment to the denture. Subsequent removal of the spacer enables the denture, when under load, to move towards the ridge without loading the matrix and patrix. The spherical form of the patrix allows the denture to rotate.
Ogata and Aoki, in 1990,11 reported that, as spacer thickness decreased, the magnitude of lateral forces decreased and the vertical forces increased. If a stable denture base can be provided, omission of the spacer is desirable, since lateral torquing forces are those most likely to cause cementation failure or root fracture. In the case of fixture supported overdentures the immobility of the fixture makes the incorporation of a spacer necessary, any small denture instability can lead to fracture of the denture.

Fig. 31-2a The bridge from 43–46 had failed in an elderly patient. An immediate partial denture was made. Dalbo attachment soldered to root cap and post (root cap and post made indirectly).

Fig. 31-2b Denture in place with matrix attached to Dalbo attachment.

Fig. 31-2c Tooth added, note the opening lingually to enable the matrix to be attached to the crown intraorally. The denture is held firmly in place with all minor connectors and rests firmly seated against the teeth or crowns and acrylic resin beaded onto the matrix to lock it to the crown. Fabrication of a new bridge would have necessitated either osseointegrated fixtures or removal of existing crowns and bridges, neither of which were desired by the patient.

Fig. 31-2d Final denture.
Advantages
- Can be used with non-parallel roots or osseointegrated fixtures provided the occlusal surfaces of the root caps can be made parallel, since the bases of the patrices should be parallel.
- Can be used as a solitary attachment in just one root, if necessary, to provide interim increased retention of the denture.
- Allows some rotation of the denture.
- Through the use of a spacer it allows, where necessary, movement of the denture towards the tissues without loading of the attachment.
- Enables fairly easy replacement of the matrix.
- Is not excessively bulky, although providing sufficient room for it can sometimes prove difficult.
Disadvantages
- Each attachment functions independently of the others, so there is no increase in horizontal stability from abutments being splinted together.
- All displacing forces may act on a single retainer, leading to cementation failure.
- They are sometimes impossible to position correctly on the root face.
- They have a poor prognosis when used with maxillary fixture retained overdentures.5
Outline of Procedure for Stud Attachments (Fig 31-2a)
1) Fabricate and fit an immediate denture.
2) Prepare the post hole(s) and root face(s), or insert osseointegrated fixtures.
3) For fixtures: second stage surgery and ball abutment connection to the fixtures. The mucosa must be allowed to heal completely before making the definitive denture. Reline the denture with tissue conditioner.
4) For teeth: impression of post hole and root face.
5) Fabricate post and root cap with patrix (see Appendix).
6) Try in the casting.
7) Reline the denture, if necessary.
8) Cut away the acrylic of the denture and ensure that it does not encroach on the casting or implant abutment.
9) Adjust the denture to ensure even mucosal contact. Paint the undersurface with pressure relief cream (Mizzy – Kerr), hold the denture in place with firm finger pressure. Observe the cream for even displacement. If uneven, adjust the bare areas (Fig 31-4d).
10) Cement the post.
11) For cemented posts wait a minimum of one hour – preferably 24 hours.
12) Attach the matrix to the denture, as described for bar and clip devices.
Bar and Clip Device
For example, Cendres et Metaux bar and clip (55.01.2); overdenture kit (Nobelpharma – DCB 110) (Figs 31-3 to 31-6 – see Appendix).
A clip fits over a cylindrical gold alloy bar. The clip springs apart to move over the greatest diameter of the bar. Occlusally directed displacing forces are resisted by the clip gripping the bar. A spacer may be placed between the clip and bar during the attachment of the clip to the denture. Subsequent removal of the spacer allows the denture to be depressed towards the ridge, without loading the clip and overlying acrylic. The bar is attached to abutment teeth by copings over tooth stumps or by copings over post and cores. It is attached to fixtures by gold cylinders attached to the abutments. Posts can only be joined to the bar by cast or soldered joints if the posts have parallel paths of insertion. Alternatively, with divergent roots, one end of the bar may be screwed to the retainer in the tooth. The clip can be adjusted by bending the leaves towards each other using a flat plastic instrument.
Advantages
- Relatively cheap.
- Flexible in application.
- Easy to vary the design with irregular ridge forms.
- Usually ample space is available for the attachment.
- Where necessary and when located correctly it allows rotation of the denture around the bar (this is particularly useful for lower dentures).
- Clips are easily adjusted and replaced, if necessary.
- The use of a spacer allows, where necessary, movement of the denture towards the tissues without loading of the attachment.
- Since they are splinted together by the bar, displacing forces are disributed to all the retainers.
- Good prognosis for mandibular fixture supported overdentures.5

Fig. 31-3a Bars and clip attached to osseointegrated fixtures. The acrylic resin is relieved lingual to the abutments to permit rotation to occur when the saddles are loaded, although saddle displacement will be minimal. Note that the bar supporting the clip is positioned perpendicular to a line bisecting the angle formed by joining the two edentulous ridges. See also Figure 33-14.
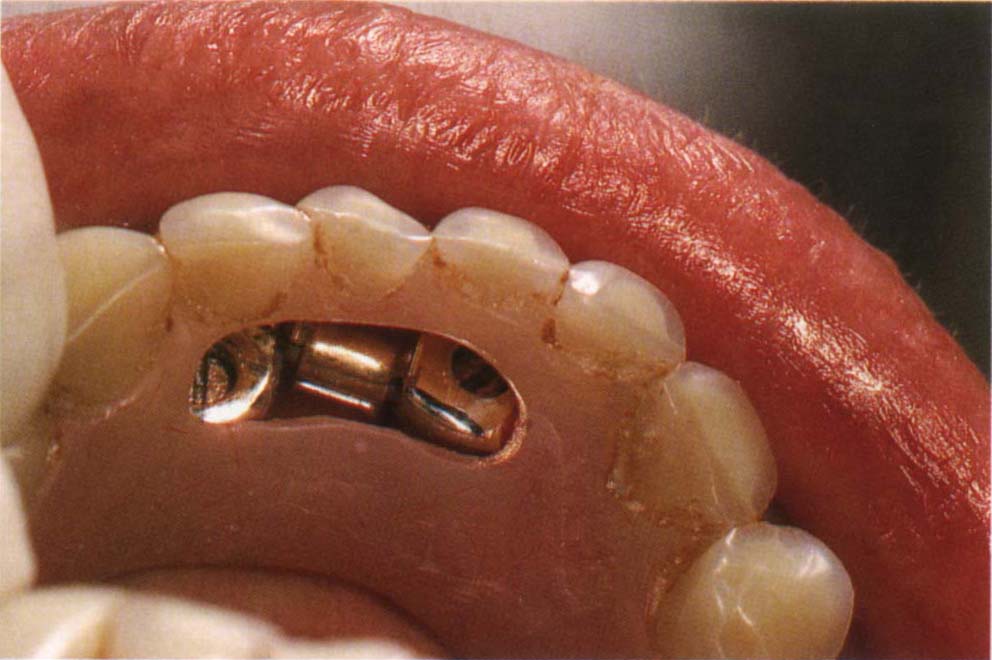
Fig. 31-3b Overdenture. There is a lingual access cavity to lock the clip to the denture intraorally. The saddles are adjusted to even contact under firm finger pressure. The clip is attached to the denture intraorally using a bead on technique.
Disadvantages
- The clips have very small areas for attachment to the denture.
- The acrylic around the clips can easily break away.
- If sufficient care is not exercised, acrylic can polymerize around the clip when attaching it in the mouth, preventing removal of the denture since the clip will not open. The clips must be suitably ‘blocked out’ (Fig 31-6r).
- If the bars are not placed parallel to the potential axis of rotation of the denture, the denture cannot rotate around the bar.
Outline of Procedure for Bar and Clip Attachments (Fig 31-4)
1) Make an immediate denture.
2) Remove failed restorations.
3) Fit immediate denture and ensure even mucosal contact using pressure relief cream. Relieve the mid-palatal bony areas.
4) Insert osseointegrated fixtures for the fixture supported denture.
5) Prepare abutment teeth or for fixtures, perform second stage surgery and connect abutments.
6) Impression for retainers.
7) Reline the denture if necessary.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


