Examination, Diagnosis, and Treatment Planning
1. Preventive considerations related to tooth sealants, nutrition, and fluoride intake. The eruption of permanent teeth may require that a decision be made about sealant application. Entry into the more heterogeneous, less controlled environment of school places the child at risk for increased carbohydrate exposure. The child’s access to fluoride in school, diet, and other sources makes regular reevaluation of fluoride exposure a necessity. Preventive issues must be reviewed as caries risk factors change during this dynamic period.
2. Prevention and management of trauma. The school-aged child may be active in sports. For a period in the school years, the permanent maxillary incisors are at greater risk for traumatic injury, especially if they protrude.
3. Development of skills in personal oral hygiene. The child emerging from the middle school years should have acquired the skills and knowledge to conduct effective personal oral hygiene.
4. Participation in health care decisions. Classically, dentists are taught to see the school-aged child as a passive recipient of care. Unfortunately, the result may be poor compliance and a tendency for the child to consider the dentist and parent rather than himself or herself as responsible for his or her own health. Usually sometime during this period, children begin to develop an image of themselves, some of which will relate to their facial and dental esthetics. This will be apart, although influenced to some extent, by their parents.
The History
Elements of history taking and recording are discussed in Chapter 18. The parent remains the historian of choice, yet the older school-aged child can provide corroborative information. An important aspect of history taking in this group should be the involvement of the child, whose role initially may be that of listener but can evolve into that of participant. By adolescence, the child can provide accurate, valuable information. Some instances in which this involvement may have profound benefits for both health care provider and patient are (1) when antibiotic premedication for heart disease is required, (2) when there is a history of illness that accompanies a complicated medical history, and (3) when there is a history of a positive reaction to the hepatitis antigen. The payoff for imparting this knowledge to the young patient through a good physician-patient relationship may not be evident until the child seeks care as an adolescent. A health history form should address issues similar to those applicable to the younger child but with different expectations. The differences in patient history for children in this age group in general include the following:
1. Medical intervention has usually occurred. Most children have a physician and may have experienced an emergency visit or some invasive procedure. School enrollment has required a physical examination and other treatment for the majority of children.
2. A health history has evolved. The coagulation and immunologic systems have been tested, and a developmental profile is available. Most childhood-onset disorders manifest themselves at some time during this period, but some have not been noted. Therefore symptoms remain an important aspect of history taking. Because more children are surviving early childhood cancer, more attention should be given to determine the types of treatments they have encountered. Full body or smaller field radiation therapy, chemotherapy, and the use of bisphosphonates all carry risks related to tooth development, eruption, and bone quality related to potential surgical interventions and tooth movement.
3. A dental history should be evolving, and caries experiences and prevention, care delivery, and dental development should be established. Children usually have undergone a dental visit as part of school enrollment.
4. The history should capture those children early on the curve of health experiences. We would be naive to presume that children are not exposed to different environmental, social, and other issues than a generation ago. The history form, unfortunately, should address substance use and pregnancy.
The Examination
Behavioral Assessment
Another advantage for the dentist is the child’s emergence into a period when few children experience behavioral problems that cannot be resolved with a simple tell-show-do method. Even early in this period, most children can be reasoned with to accept dental treatment. The child who resists attempts at careful and compassionate explanations of care may be suffering from a more significant emotional or psychological problem. Significant behavior problems in the presence of normal intelligence signal a serious deviation from normal. The diagnostic process for behavioral problems is clearer in this age group because so few children resist care. The dentist’s diagnostic approach should include ruling out major behavioral problems by a history and general appraisal. The next step is to “chair-test” the child, using the dentist’s proven techniques of managing children. The technique used may be tell-show-do, positive reinforcement, voice control, or some other method that has worked consistently in the past. Remember that consent must be obtained from the parent if the behavior management technique used is not one that a reasonable parent would expect.1 If behavioral intervention fails, the dentist should consider further evaluation or referral. Some causes of extreme behavior problems in this age group include substance abuse, physical or sexual abuse, family problems, or a learning disability.
General Appraisal
One advantage available to the dentist who treats children in this age group is the host of health professionals with whom he or she can work if problems are noted. School placement often has identified problem areas, and the appropriate therapy usually has been initiated. These professionals can assist in clarifying findings made during the dental visit. Box 30-1 lists some characteristics of the school-aged child that are important in the diagnostic process.
Determination of Developmental Status
A series of measurements, which may be available from the patient’s physician or school nurse, provides much more information. The measurements can be plotted in one of two ways. The first way is to plot the measurements on a cumulative growth chart (Figure 30-1). This provides information about the patient’s total amount of growth up to the last measurement. The normal growth curve is sigmoidal, and the pubertal growth spurt corresponds to the steepest portion of the slope. Because growth charts are based on mean growth rates, the individual patient may show an accelerated or delayed growth spurt if his or her growth rate is not coincident with the mean growth rate. More importantly, some concern should be expressed if the patient is not following the percentiles (e.g., dropping from the 50th to the 40th to the 30th percentile over time). This suggests there may be a physical or psychological problem requiring medical attention.
Height and weight measurements can also be plotted as yearly growth increments rather than as total growth achieved up to that point (Figure 30-2). By plotting measurements this way, changes in the growth rate can be easily identified. A sharp rise in height usually signals the start of the pubertal growth spurt, and growth modification treatment should be initiated immediately if it is required.
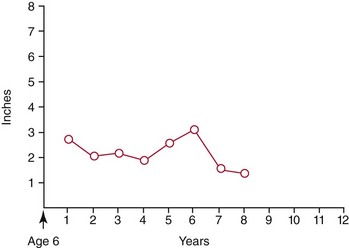
 FIGURE 30-2 Growth information also can be plotted as yearly growth increments rather than as total growth achieved to a certain point. The growth data for the female patient described in Figure 30-1 are plotted here incrementally, beginning at age 6 years. By plotting measurements this way, changes in the growth rate can be easily identified. A sharp rise usually signals the start of the pubertal growth spurt.
FIGURE 30-2 Growth information also can be plotted as yearly growth increments rather than as total growth achieved to a certain point. The growth data for the female patient described in Figure 30-1 are plotted here incrementally, beginning at age 6 years. By plotting measurements this way, changes in the growth rate can be easily identified. A sharp rise usually signals the start of the pubertal growth spurt.
Hand-wrist radiographs have been used by some investigators to judge the skeletal age and development of the patient. The size and maturational stage of certain hand and wrist bones are compared with published standards of normal bone development and skeletal age.2 Unfortunately, the correlation between the appearance of reliable bone markers (skeletal growth status) and mean maximal mandibular growth velocity is not perfect and should not serve as the only index of facial growth. There are several problems with this method of determining developmental status by the dentists. First, it requires an additional radiograph. Second, the ability to reliably read hand-wrist radiographs requires consistent practice that is rarely gained in routine patient care.
Another radiographic method that does not require additional radiation exposure is the use of cervical vertebral maturation from routine cephalometric radiographs (Figure 30-3). This method uses the maturation stages of the second through fourth cervical vertebrae (Figure 30-4) to evaluate mandibular growth potential. It is claimed that the peak mandibular growth occurs between stages 2 and 3 in the 5 stage method.3 Timing treatment for growth modification during this period of growth, according to some, could enhance the treatment effects.4 There is some disagreement regarding the reliability of this method, but is has been shown to be highly reliable for making the determination whether a patient’s mandibular growth rate is still increasing or has passed its peak (i.e., stage 1 or 2 versus stage 3, 4, or 5). That is the clinically relevant determination for the patient being considered for growth modification.5

 FIGURE 30-3 Another method used to gauge growth status is evaluation of the shape of cervical vertebrae 2, 3, and 4. These images are available on routine cephalometric radiographs and require no additional radiation. It appears they can be reliably read and are interpreted according to the stages described in Figure 30-4.
FIGURE 30-3 Another method used to gauge growth status is evaluation of the shape of cervical vertebrae 2, 3, and 4. These images are available on routine cephalometric radiographs and require no additional radiation. It appears they can be reliably read and are interpreted according to the stages described in Figure 30-4.
Secondary sexual characteristics provide some information about the amount of growth the patient has yet to experience. In females, breast stage development and menarche are markers that can be used to assess developmental status. Breast development determination as an objective clinical evaluation is obviously not practical in the dental office and is of little clinical use. Menarche, however, can be determined from the health history questionnaire or from an interview at the initial patient examination. Unfortunately, the pubertal growth spurt precedes menarche by more than 1 year.6 Therefore menarche is basically used to decide whether growth modification is still feasible.
For a person with an obvious skeletal problem, more than one cephalometric head film of the patient may be available. These head films can be superimposed to provide information about the amount and direction of growth that has occurred over time (see later discussion on cephalometric analyses and Figure 30-52). Although past growth tendencies do not guarantee that the patient will continue to grow or will grow according to the same pattern, comparing head films provides a great deal of information about the patient. However, it is unlikely for the average patient to have a series of head films available for pretreatment review.
The patient’s developmental status can also be judged from the developmental stage of the dentition. Panoramic or periapical radiographs can be used to determine the stage of development of individual permanent teeth. The results can be compared with standards relating dental development to chronological age.7 However, studies indicate that the relationship between dental age and skeletal maturation is weak and clinically useless.8
Head and Neck Examination
The head and neck examination should be completed in a manner similar to that outlined in Chapter 18.
Facial Examination
Facial examination of the 6- to 12-year-old child is a systematic examination of the face in three planes of space. It is essentially the same as the facial examination described in Chapter 18, and the reader should review that information if necessary. This section comments on findings that are particularly important for the 6- to 12-year-old.
In examination of the profile, one notes the anteroposterior and vertical dimensions of the face and the position of the lips and incisors relative to the face. The ideal soft tissue profile is slightly convex (Figure 30-5), practically speaking a bit straighter with more mandibular contribution than that of the preschool-aged group. Most clinicians find that detection of anteroposterior skeletal problems is somewhat easier in this age group, possibly because of reduced soft tissue thickness. A mild mandibular deficiency in a 4-year-old child may have been difficult to diagnose initially, but it is more apparent at age 8 years and even more obvious at age 12 years. In most cases, skeletal relationships can be confirmed by the dental relationships (molar and overjet). That means that if the facial form (convex, straight, or concave) matches the dental relationships (respectively, class I molar and moderate overjet, class II molar and 5- to 6-mm overjet, or class III molar and zero or negative overjet) there is usually not much doubt about the skeletal relationships. If a skeletal problem exists, the source of the discrepancy is identified by comparing the position of the maxilla and mandible with a vertical reference line through soft tissue nasion (see Chapter 18, Figures 18-1 to 18-3). This helps to direct treatment, if indicated, to the skeletal component at fault.
Again in this age group, vertical profile assessment continues to concentrate on the proportionality of the middle and lower facial thirds. At this point, growth has increased the vertical linear facial dimensions, and the proportionality of the well-balanced face remains basically the same, but the lower facial third is slightly larger than the middle facial third. Research has indicated that vertical dysplasia usually is confined to the lower facial third in this age group.9 Therefore the middle third can be compared with the lower facial third (see Figure 30-5).
Incisor and lip position should be examined carefully in this age group. The child is entering the mixed dentition period, and the position of the erupted permanent incisors generally is reflected in the position of the lips. The upper lip gives a good indication of the underlying position of the maxillary incisor. The position of the lower lip also depends on the position of the maxillary incisor because the lower lip normally covers 1 to 2 mm of the maxillary incisal edge at rest. Therefore lip posture is a strong indicator of maxillary dental protrusion. Lip and incisor position should always be considered in the context of the nose and chin. A large nose and chin are more able to accommodate protrusive incisors and lips than are a small nose and chin. As a general rule for white children, the lips should be positioned on or slightly behind a line connecting the tip of the nose with the chin (Figure 30-6). Most Asian and African-American children have more incisor and lip protrusion than white children. When the incisors are fully erupted it is possible to begin to consider their vertical position relative to the lips. This gives an indication of some critical esthetic relationships. Lips tend to grow vertically throughout the early adolescent years. It is not uncommon to see children early in this age group with incompetent lips (lips that do not approximate or have more than a couple of millimeters of separation at rest). The maximum display of incisors at rest and maximum lip incompetence occurs around 11 years in females and 12 years in males.10 Most children become more lip competent as they mature. Ideally, a child shows about 2 mm of tooth below the relaxed lip line. At full smile, they show nearly the full tooth with the upper lip retracting to a couple of millimeters below the cervical area of the tooth. Gingival exposure of not more than 2 mm is considered esthetically acceptable for this age group. Of course, there can be much variation while still maintaining good esthetics, but these are generally accepted guidelines.
Intraoral Examination
Periodontal Evaluation
1. Selective probing of anterior teeth and permanent first molars. A periodontal probe is necessary to evaluate the health of the tissues properly (Figure 30-7). The probe measures the depth of the sulcus and the amount of free marginal and attached gingiva. Bleeding upon probing is also an indication of active gingival disease. Sulcular depths of greater than 3 mm and attached gingiva of less than 1 mm indicate possible periodontal problems, and further evaluation is warranted. The likelihood of bone loss and apical migration of the attachment is low, but some children in this age group experience aggressive periodontitis. Erupting teeth usually have a deep sulcus until the crown is fully erupted. Gingival inflammation in early puberty may also confound pocket-depth measurements.
2. Evaluation of tissue attachments, especially those of the lower anterior teeth. Facial clefts as a result of malpositioning of teeth and inflammation, if identified early, can be successfully managed with grafting, tooth movement, or a combination of both (Figure 30-8). The amount of attached gingiva also should be considered in the context of the type of tooth movement being planned. Facial movement of a lower incisor with minimal attached gingiva may cause further loss of attachment, and a periodontal evaluation is indicated. Often simply proceeding cautiously will be acceptable, but in other instances a gingival grafting procedure may be considered. Lingual movement of the same incisor does not involve the risk of loss of attachment and may even contribute to an increase in attached tissue. Last, the position of the frena and their height of attachment on the alveolar ridge should be determined via gentle manipulation of the lips and cheeks. Occasionally, frenal attachments near the crest of the ridge must be repositioned before or after orthodontic treatment because they pull on attached marginal tissue and compromise gingival health or prevent space closure.
3. Identification of problem areas, such as mandibular and maxillary anterior teeth. Calculus accumulation, inflammation secondary to anterior crowding, poor cleaning, and eruptive gingivitis are examples of localized problems that require specialized attention.
Numerous gingival indices exist to assess inflammation.11 The gingival index (GI)12 can be adapted for pediatric use. The GI uses the following scoring system: 0 = normal gingiva; 1 = mild inflammation: slight change in color, slight edema, no bleeding on probing; 2 = moderate inflammation: redness, edema, and glazing, or bleeding on probing; 3 = severe inflammation: marked redness and edema, tendency toward spontaneous bleeding, ulceration.
Occlusal Evaluation
The occlusal evaluation is organized around a systematic approach to alignment and the anteroposterior, transverse, and vertical planes of space.13
Tooth Number
After the form and symmetry of each arch have been characterized, it is imperative to count the number of permanent and primary teeth. A clinical examination and appropriate radiographs allow the practitioner to determine which teeth are present, developing, or missing. Disturbances in the initiation and proliferation stage of tooth development may lead to an abnormal number of teeth. Teeth that do not form are referred to as congenitally missing (Figure 30-9). The most common missing teeth in the permanent dentition, with the exception of the maxillary and mandibular third molars, are the mandibular second premolar, maxillary lateral incisor, and maxillary second premolar in that order.14 In general, the most distal tooth in a class of teeth is most liable to be congenitally missing. Some have looked at whether there is a genetic component to missing and impacted teeth. It is reported that patients with palatally impacted canines exhibit a higher incidence of missing permanent teeth than the general population and that several generations in the family will exhibit the same palatal impaction15 (Figure 30-10). Recent evidence suggests there are specific genes that cause specific tooth loss when there is a mutation.16 It is apparent that future genetic study may identify more genes that affect tooth development. The practical implication of a missing anterior tooth is to look elsewhere in the mouth for more eruption or tooth development issues (additional missing teeth, impaction or transpositions).
Another cause of missing or malformed teeth is radiation therapy or chemotherapy. This can affect the formation and eruption of the teeth forming at the time or those in the field of the therapeutic beam. Generally those patients treated with radiation as part of the regimen and before age 5 years have more anomalies of dental development, but patients receiving chemotherapy and older patients who still have developing teeth are likely affected (Figure 30-11).17
Supernumerary teeth are teeth added to the normal complement of teeth. These teeth are found in about 2% of the population and are most often found in the maxillary midline region.18 Midline supernumerary teeth are also called mesiodens (Figure 30-12). Supernumerary teeth are also found distal to the maxillary molars and in the mandibular premolar regions.
Although not a tooth in the strictest sense, the odontoma is discussed in this section on tooth number. The odontoma is a benign mixed tumor of enamel and dentin that is diagnosed radiographically. Two types of odontomas are identified. Odontomas that resemble teeth are called compound odontomas; those that are irregularly shaped are labeled complex odontomas. Both types may interfere with normal tooth eruption and are usually treated by surgical removal before eruption problems arise but late enough to avoid surgical trauma to adjacent developing teeth (Figure 30-13).
Tooth Structure
Disturbances in the morphodifferentiation and histodifferentiation stages of tooth development result in alterations of tooth size and shape. Each arch should be examined for generalized large (macrodontia) or small (microdontia) teeth and for localized tooth size discrepancies. Generalized large or small teeth usually can be aligned so that there is a compatible occlusal relationship if the teeth in both arches are equally affected. However, localized tooth size problems make it difficult to establish good dental relationships. Again, the most distal tooth in the dental class is the one most often affected. Undersized maxillary lateral incisors and mandibular second premolars are the most common isolated problems in tooth size (see Figure 30-10, A). These also appear to be genetically linked anomalies, so evaluating patients with peg laterals should include evaluation for palatally displaced canines, additional missing teeth, and transpositions. Sometimes complex orthodontic and restorative treatment is necessary to achieve a harmonious occlusal relationship and satisfy aesthetic requirements when local tooth size problems exist. This type of treatment usually amounts to distributing space between the teeth so that when the teeth are restored to normal size and contour, they fit in a good occlusal relationship with good anterior esthetics (Figure 30-14). Other times, treatment may mean reducing the mesiodistal dimension of oversized crowns through interproximal reduction (Figure 30-15).
Teeth with abnormal crown and root morphologic characteristics may create occlusal problems. Careful clinical and radiographic examination is necessary to diagnose these problems. If the abnormality involves the crown (maxillary peg lateral or talon cusp), either the crown should be recontoured by addition of restorative material to increase its size or the talon cusp should be reduced in size by selective equilibration to eliminate occlusal interference (Figure 30-16). Both conditions usually require tooth movement before definitive restorative care to obtain an aesthetically pleasing and functional result. Root structure abnormalities such as significant dilaceration may make orthodontic movement of teeth difficult (Figure 30-17). Often the portion of the root apical to t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline Box 30-1
Box 30-1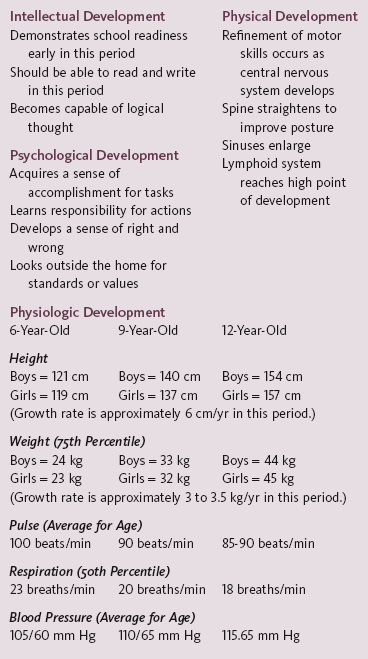
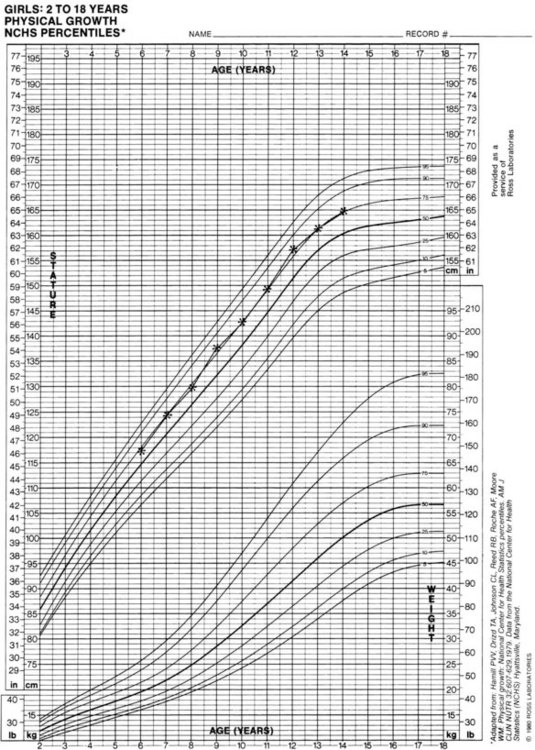
 FIGURE 30-1
FIGURE 30-1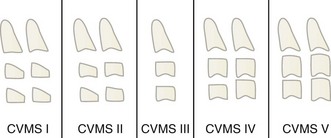
 FIGURE 30-4
FIGURE 30-4
 FIGURE 30-5
FIGURE 30-5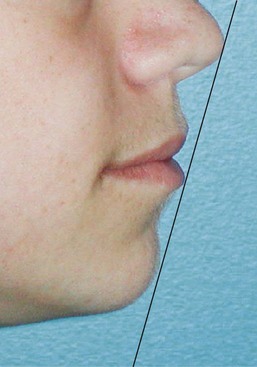
 FIGURE 30-6
FIGURE 30-6
 FIGURE 30-7
FIGURE 30-7
 FIGURE 30-8
FIGURE 30-8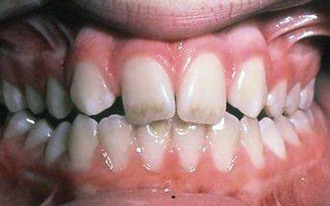
 FIGURE 30-9
FIGURE 30-9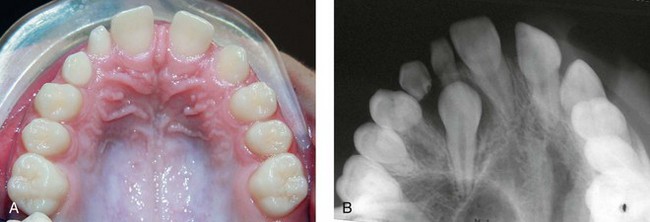
 FIGURE 30-10
FIGURE 30-10
 FIGURE 30-11
FIGURE 30-11
 FIGURE 30-12
FIGURE 30-12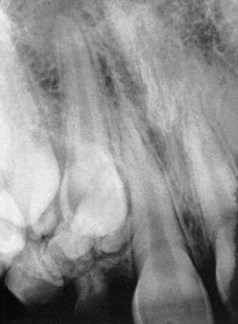
 FIGURE 30-13
FIGURE 30-13
 FIGURE 30-14
FIGURE 30-14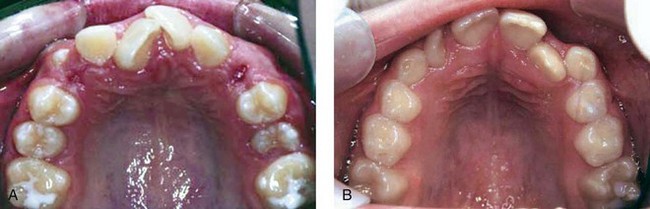
 FIGURE 30-15
FIGURE 30-15