CHAPTER 3
RADIOLOGICAL INVESTIGATION OF SALIVARY GLAND LESIONS
Imaging plays a major role in the management of patients with head and neck tumors, which includes tumors developing in the salivary glands. Imaging can define the location, origin, and frequently the nature of the mass lesion. It also aids in the staging of head and neck cancer.
3.2 OVERVIEW OF IMAGING MODALITIES
Currently, a variety of imaging modalities are often used for evaluating the major salivary glands. The most common in our practice is contrast enhanced computerized tomography (CT) of the entire neck obtained on a multidetector CT scanner. A volume of data at 0.6-mm isometric voxels is acquired from the level of sella turcica to the level of aortopulmonary window. Axial images are then reconstructed using soft tissue and bone window algorithms at 3-mm intervals. Reformations are obtained routinely in the coronal and sagittal planes at 3-mm intervals.
CT remains the modality of choice for the initial assessment of head and neck cancer. It provides valuable information about the location, margins, size, and extent of the tumor. Additionally, CT is the best available imaging modality for detection of calcifications and stones (Figure 3.1).
FIGURE 3.1. Sialoadenitis of right submandibular gland. Coronal CT scan shows enlarged right submandibular gland (long black arrows) with edema of the adjacent tissue planes. There are dilated ducts (short white arrows) with multiple stones (open arrow).

The second most common modality in our practice is magnetic resonance imaging (MRI). In a few situations, MRI is the modality of choice in evaluating salivary gland lesions. We may begin our initial evaluation with MRI if there is a high clinical suspicion of malignancy based on a hard, rapidly growing mass in an adult patient and especially when cranial nerve palsy is present. We tailor the MRI study according to the region of interest. Typically, we acquire axial and coronal T1 weighted images (T1WI) at 4-mm intervals with a 10% gap, coronal T2 weighted images (T2WI) with fat suppression at 4-mm intervals with a 10% gap, and axial T2WI at 4-mm intervals with a 10% gap; finally, we inject intravenous gadolinium-based contrast material and acquire fat-suppressed coronal and axial T1WI with a 10% gap. Diffusion weighted imaging (DWI) is advantageous in predicting malignant versus reactive lymphadenopathy in the neck.
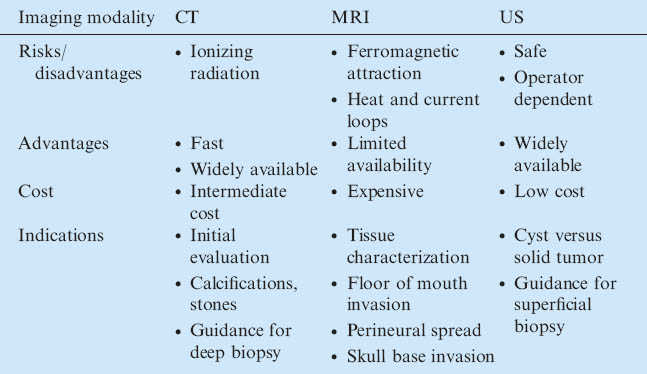
TABLE 3.1. Imaging modalities in common use
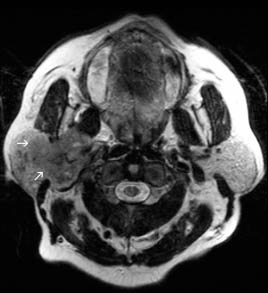
Because of its exquisite tissue contrast and multiplanar capabilities, MRI is the study of choice in evaluating the presence of perineural spread of tumor, violation of the adjacent tissue planes, and invasion of the skull base (Figure 3.2). Unenhanced T1WIs show a relatively dark tumor signal against a bright, fatty background especially in the parotid gland. Fat suppression techniques become necessary when contrast material (gadolinium) is used. T2WIs are useful in evaluating cysts and in detecting the cystic components associated with some solid tumors. Cysts appear well defined with a bright signal on T2WI and a dark signal on T1WI (Figure 3.3). Benign lesions tend to be well defined with a relatively bright signal on T2WI (Figure 3.4), which is in contradistinction to malignant tumors that tend to have a relatively dark signal on T2WI (Figure 3.5).
FIGURE 3.2. Adenocystic carcinoma of right ehmoid and shenoid sinuses. (a) Axial T2WI shows heterogeneous tumor with relative dark T2 signal (long white arrows). The tumor invades the right pterygopalatine fossa with intracranial extension along the trigeminal nerve. The right cavernous sinus is filled with tumor (double short white arrows). Notice normal contralateral pterygopalatine fossa (open arrow). (b) Postcontrast T1WI shows heterogeneous enhancement of the mass and better visualization of intracranial invasion.
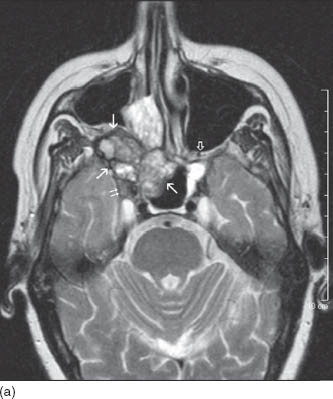
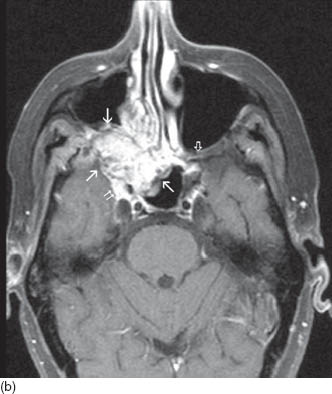
FIGURE 3.3. First branchial cleft cyst of parotid gland. (a) Axial T2WI shows a cystic lesion in the left parotid gland with bright contents (asterisk) and irregular dark capsule (black arrows). (b) Axial T1WI shows dark signal of the cyst (asterisk) in the background of bright fat containing normal parotid tissue. (c) Axial post contrast T1WI shows enhancement of the cyst wall (black arrows) while the cyst contents (asterisk) do not enhance.
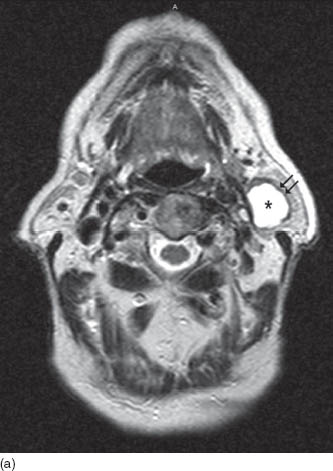
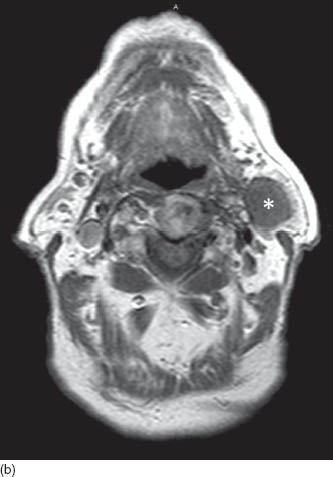
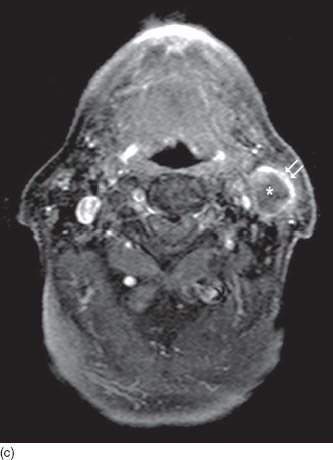
FIGURE 3.4. Pleomorphic adenoma. Axial T2WI shows a bright, lobulated, and well-defined tumor in the deep lobe of the parotid gland (white arrows).

FIGURE 3.5. Basaloid cell carcinoma. Axial T2WI shows a relatively dark and poorly defined tumor in the parotid gland (white arrows).
Ultrasound (US) is used in some practices as the initial modality in evaluating major salivary glands, reserving other modalities for subsequent assessment. US is useful in differentiating the solid versus cystic nature of accessible head and neck lesions. It might also provide guidance for needle aspiration biopsy. In our institutions, most deep neck and parotid masses are sampled under CT guidance.
Lymphatic spread is not a common path for metastasis in salivary gland malignancy. Positron emission tomography (PET) with or without CT is implemented commonly in our institution for staging and initial evaluation of distant metastatic disease (Figure 3.6). Nuclear medicine techniques have limited use in localized salivary gland disease. Sodiu/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


