Maxillofacial Ballistic and Missile Injuries
Epidemiology
Fatal and Nonfatal Firearm Injuries
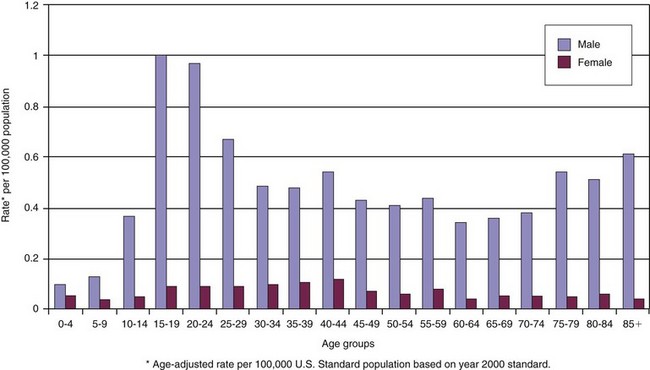
The most current comprehensive analysis of fatal and nonfatal firearm injuries in the United States was accomplished by Gotsch et al in 2001.1 In excess of 115,000 firearm-related injuries occur annually in the United States, with firearms involved in over 58% of homicides and 57% of suicides. Approximately 30,000 of them sustained fatal wounds from these incidents, but more than twice this number survived their injury, many with significant injuries and permanent disabilities.2 Coben, in 2003, reported the average hospital length of stay for a firearm-related wound was 6 days, with 7% of hospitalized firearm wound patients expiring from their injuries, and estimated hospital costs to be in excess of $800 million.3 Because 29% of these patients were uninsured, and the estimated cost of firearm-related injuries per incident in the United States is in excess of $17,000 (over $2.3 billion aggregate lifetime medical costs for firearm injury survivors), the societal impact and payment implications for hospitals, local government, and taxpayers are immense.4,5 Black males are disproportionately more likely to suffer firearm-related injuries than any other ethnic group or gender1 (Fig. 27-1). According to Logan et al, the homicide rate for black males aged 10 to 19 years (1999 to 2002) was 17.8/100,000, a rate 10 times that of whites (1.8/100,000), three times that of Native Americans (6.0/100,000), and more than double the rate for Hispanics (8.0/100,000). 6 The Federal Bureau of Investigation (FBI) and Centers for Disease Control and Prevention (CDC) reported in 2003 that firearms were used in 66.9% of homicides in the United States, so the logical conclusion would be that the acute management of these conditions in the American health care system would be an expected event7 (Fig. 27-2). In 2007, homicide was the sixth leading cause of death for blacks, regardless of age, while it ranked as the fifteenth leading cause for death when all races were included.8 A 1999 report indicated that over 32,000 deaths resulted from firearm injuries in 1997, making it the second leading cause of death after motor vehicle accidents (MVAs). This article highlighted the positive efforts by the medical community to effect change in treatment protocols and the educational outreach programs by law enforcement, government, and the community to reduce the impact of firearms in the United States. There was a reduction in firearm fatalities since 1995 by 29.3% and the number of nonfatal injuries by 46.9%9,10 (see Fig. 27-2D and E).
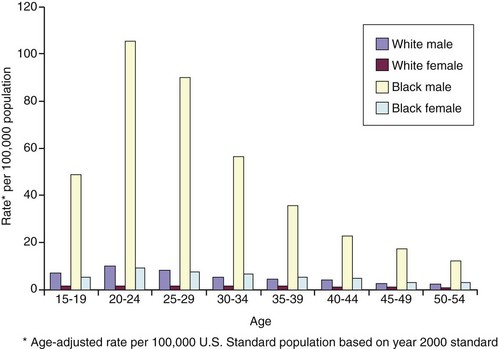
FIGURE 27-1 Demographics of firearm homicides for ages 15-54 by race and gender in the United States, 2002. (Data from National Center for Injury Prevention and Control: WISQARS leading causes of death reports, 1999-2007 [http://webappa.cdc.gov/sasweb/ncipc/leadcaus10.html]).
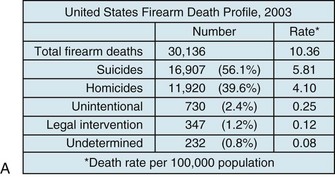
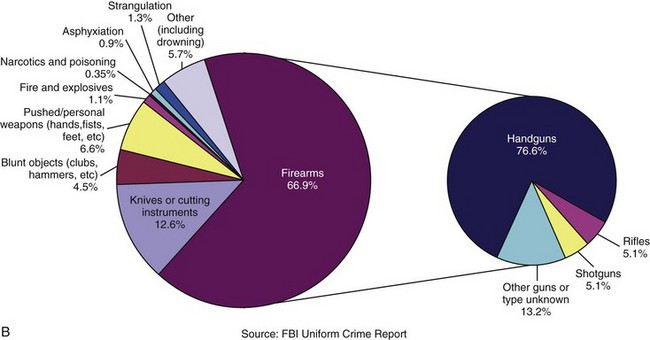
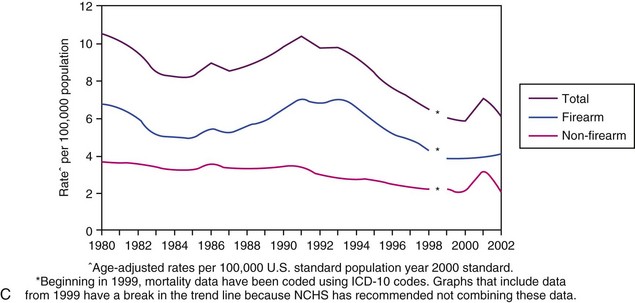
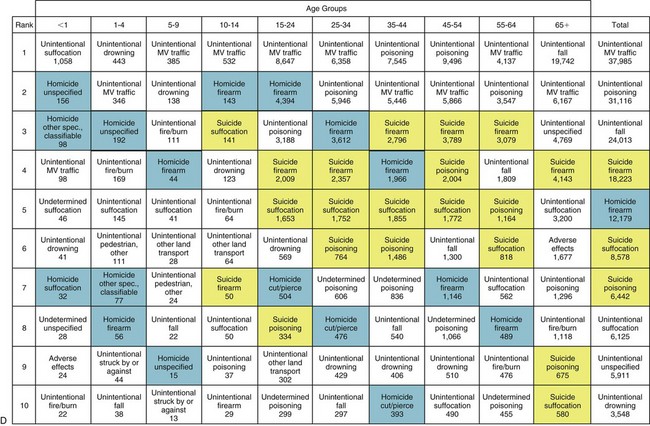
FIGURE 27-2 A, Firearm death rates in the United States by intent, 2003. B, Homicide weapons in the United States by type, 2003. C, Firearm and non-firearm homicide trends in the United States,1980-2002. Note the peak in the early 1990s followed by a steady trend downward. D, Top 10 leading causes of violence-related injury deaths in the United States, 2008. (A, C, Data from National Center for Injury Prevention and Control: WISQARS leading causes of death reports, 1999-2007 [http://webappa.cdc.gov/sasweb/ncipc/leadcaus10.html]; B, Data from Federal Bureau of Investigation: Crime in the United States, 2003 [http://www.fbi.gov/about-us/cjis/ ucr/crime-in-the-u.s/2003/toc03.pdf]; D, Data from National Center for Health Statistics: Top 10 leading causes of violence-related injury deaths in the United States, 2008, [http://nchspress room.wordpress.com/2009/10/21/10-leading-causes-of-violence-related-injury-deaths-suicide-is-leading-killer].)
Risk Factors for Firearm Injuries
Unintended Firearm Injuries
Unintentional firearm injuries and deaths represent a very small proportion of the total number of firearm injuries and have steadily declined since the 1930s.11,12 Ismach et al evaluated unintended shootings in the Atlanta area from May 1996 through June 2000 in an effort to determine the proportion of accidental injuries that might be prevented by safer storage, handling, or firearm design.13 Of the 216 unintentional firearm injuries recorded during this period, most victims were 15 to 34 years of age; 25% of the shootings involved victims younger than 18 years. Handguns were involved in 87% of the incidents. Of the 122 cases for which details of causation could be established, 74% of the incidents were associated with mishandling of the firearm, 14% were associated with child access to the firearm, and 32% were associated with perceived deficiencies in firearm design. It was concluded the incidence of unintended shootings could be decreased by improving the safety of firearm storage and limiting access, improving available firearm safety mechanisms, and educating owners about the safe handling of firearms, policies confirmed by additional studies conducted by Kochanek et al and the CDC.8,14
Pediatric Firearm Injuries
As noted by Kochanek et al, the pediatric population is at a disproportionately higher risk for firearm-related injuries.14 Paris et al have evaluated risk factors associated with nonfatal firearm injuries among inner city adolescents in the United States and found that children living with less than two parents, with frequent school absences, with a previous arrest history, and being black were factors placing them at increased risk for being the victim of firearm injury.15 Nance et al have evaluated demographics and contrasting urban versus rural firearm injury trends for Pennsylvania and found that the rate of serious firearm injury in children was 10 times higher in urban areas than in rural areas.16 Urban firearm injuries tended to be assaults, whereas rural injuries tended to be nonintentional. Of these injuries, 90.7% were in male adolescents, with an average age of 16.5 years. Unintended injuries predominated in children 5 to 9 years of age (61.4%), with 56.7% of these injuries occurring in rural areas. Handguns were the most commonly involved firearms, regardless of geographic region, age, or injury circumstances. Nance et al have appropriately that concluded that prevention strategies must be region- and situation-specific, taking these demographic variations into account.16 Heninger and Hanzlick have reported similar results in 2008, with firearms being used in 88% of homicides and 61% of suicides in adolescents and teenagers in the Atlanta metropolitan area17 (Fig. 27-3).
Alcohol and Drug Abuse
An intuitive and well-demonstrated risk factor for firearm-related injury is the use or abuse of alcohol or other recreational or prescription drugs. Madan et al have reported on the blood and urine analyses of 126 traumatically injured patients, regardless of the cause of injury, younger than 21 years, with 42% of them testing positive for alcohol or drugs.18 When the grouping was narrowed to gunshot wounds in patients younger than 18 years, 72% of victims demonstrated evidence of substance use, with the 14- to 15-year old age group showing the highest association. Studies conducted by McLaughlin, Shuck, and Johnson et al have demonstrated an association between drug or alcohol use and the risk of firearm injury.19–21
Other Risk Factors
Although this is not a complete listing of all factors associated with an increased risk of firearm injury, known influences include the following19–27:
1. Previous or current involvement in the justice system
4. Suicidal ideation or active psychiatric disease (Fig. 27-4)
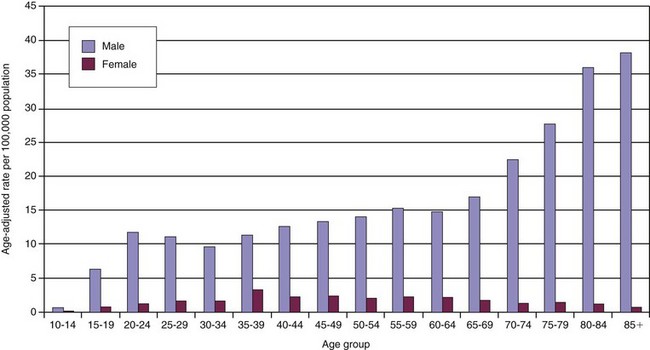
FIGURE 27-4 Firearm suicide by gender and age in the United States, 2002. (Data from National Center for Injury Prevention and Control: WISQARS leading causes of death reports, 1999-2007 [http://webappa.cdc.gov/sasweb/ncipc/leadcaus10.html).)
5. Presence of firearms in the home
6. Ethnic minority status (particularly black)
Characteristics of Maxillofacial Ballistic and Missile Injuries
The management of ballistic injuries to the craniomaxillofacial zone is predicated on a basic understanding of the two mechanisms whereby projectiles cause tissue damage, crushing and stretching. As the recent conflicts in Iraq and Afghanistan have highlighted, missile injuries to the maxillofacial region may not only be caused by conventional weaponry, with a bullet fired from a cylindrical chamber, but devastating projectile collisions with the facial skeleton may be caused by massive bomb blasts and shock wave impacts from improvised explosive devices (IEDs).28 Although a comprehensive analysis and discussion of the physics of energy transfer and ballistic theory is beyond the scope of this chapter, a brief review of the basic concepts of ballistics and kinetic energy is warranted.
Categorization of Gunshot Injuries
Gunshot injuries have been categorized in the literature as penetrating, perforating, or avulsive.10 Penetrating wounds are caused by the projectile striking the victim but not exiting the body. Perforating injuries have entrance and exit wounds, classically described as being without appreciable tissue loss. Avulsive injuries have entrance and exit wounds, generally presenting with an acute loss of tissue associated with passage of the projectile out of the victim. Rifles, handguns, and submachine guns have rifled barrels—essentially, spiral grooves cut into the length of the interior of the bore of the barrel.29 The grooves are separated by segments of metal, called lands, which project into the middle of the barrel. The diameter of the barrel measured between the lands represents the caliber of the projectile.
Caliber specifications based on nomenclature used in the United States can be difficult to comprehend. The .30-06 and Winchester .308 cartridges are both loaded with bullets that have a diameter of .308 inches.29 The “06” in this term describes the year, 1906, when the cartridge was introduced to the market. The term grains originally was applied to black powder charges and refers to the weight of the powder in the cartridge, not the number of granules contained in the cartridge case. A .30-30 cartridge has a .308-inch diameter bullet propelled by 30 grains of smokeless powder. As newer forms of gunpowder were developed, this powder charge was no longer used, but the terminology persists to this day. Additional confusion regarding caliber exists because North Atlantic Treaty Organization (NATO) and United States military projectiles are described using the metric system (7.62- or 9-mm rounds), while United States civilian firearm munitions are generally referred to in measurements relating to inches (.357 or .38). Although the question regarding caliber is commonly asked by medical personnel in the management of ballistic injury, the reality is that caliber has minimal practical impact on the care of the patient.30–32
The terms high velocity and low velocity as they relate to projectiles can be somewhat misleading. There is no consensus between United States and European research in the literature, with varying definitions correlating to where the study was performed. The U.S. literature designates high velocity as being between 2000 and 3000 feet/second (610 to 914 m/second), whereas studies from the United Kingdom designate the line between low- and high-velocity projectiles as being 1100 feet/second (335 m/second), which is the speed of sound in air.33 The earliest recognized entry of high-velocity projectiles having an association with increased wounding potential occurred during the Vietnam War. In 1967, Rich et al have reported that bullets fired from the M16 rifle inflict tremendous tissue destruction and injuries on enemy combatants.34 The muzzle velocity of the projectile shot from the M16 was 3100 feet/second. When coupled with erroneous information published by Rybeck in 1974, and in the 1975 edition of the Emergency War Surgery manual regarding the size of the temporary cavity caused by the missile, this information led to the common misperception that high-velocity projectiles cause more significant injuries.35
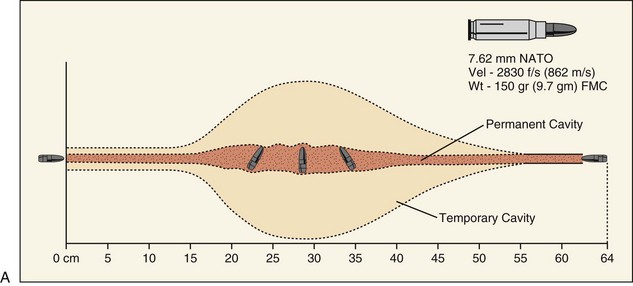
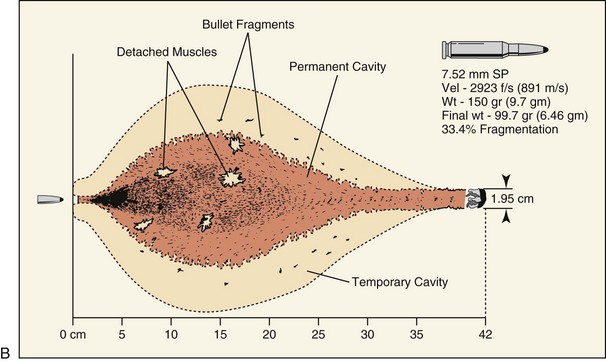
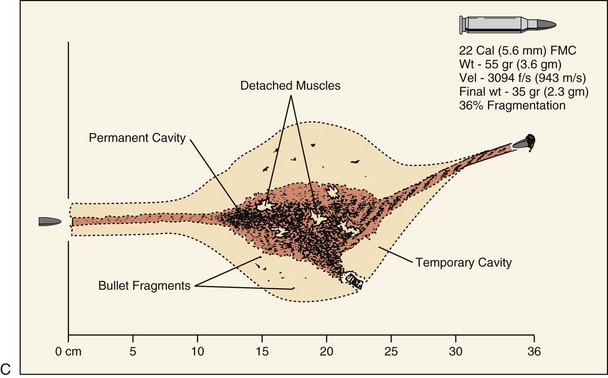
Part of the confusion regarding the wounding potential of high-velocity projectiles is becsause of misinterpretation of ballistic gelatin model studies. Ballistic gelatin is 10% to 20% gelatin refrigerated to 4° to 10° C (39° to 50° F) and is used as the tissue model for ballistic studies.36,37 The wound profile diagrams included in this chapter represent the findings of these studies. The validity of the ballistic gelatin model has been confirmed by comparison with human autopsies, although there is confusion in correlating these studies to living patients, because the human body is more resistant to deformation than gelatin The effects of skin resistance, clothing, and opposition to separation of the fascial planes cannot be replicated in gelatin.38,39
Harvey et al evaluated the two types of pressure waves produced by penetrating objects in 1947, the sonic pressure wave and temporary cavity.40 The first wave is the sonic pressure wave, sometimes referred to as the shock wave. This relates the sound of the projectile striking the target. This wave transmits at the speed of sound (i.e., ≈4750 feet/second [1450 m/second]) and is traveling considerably faster than the projectile entering the target. No temporary cavity is formed with the sonic pressure wave; in that regard it is analogous to the lithotripsy devices used for renal calculi destruction, with corresponding minimal risks for tissue injury.31 Although American and Swedish researchers have tried to disprove Harvey’s conclusions, no definitive evidence suggests that his findings are in error, and additional studies by French and American researchers have supported the original findings.32,41–45
The secondary pressure wave, referred to as the temporary cavity, is formed when the penetrating projectile strikes tissue and the wave radiates away laterally away from the permanent cavity of the projectile path. After being struck by the projectile, the ballistic gelatin or tissue displays an obvious temporary cavity, which potentially injures tissues such as muscle, vessels, and organs. The clinical significance of this cavity is variable, with no real consensus in the literature. The temporary cavity caused by the M16 in animal laboratory models is much smaller than the approximately 18-cm temporary cavity seen in ballistic gelatin.30 Dog models have indicated that acute tissue injury secondary to temporary cavity formation sustained with high-velocity projectile strikes were no more than 5 cm and were able to resolve within 72 hours.46,47 The U.S. military has conducted extensive research into the wounding patterns of projectiles (see Fig. 27-5). The unique anatomic differences of the craniomaxillofacial skeleton, a relatively thin soft tissue layer overlying a dense foundation of bone, mitigate some of the expected responses of the temporary tissue stretch, because the overall thickness of the soft tissue envelope is generally less than the required total distance needing to be traveled prior to exhibiting secondary cavitation. Although sequential soft tissue necrosis and small vessel damage can occur, it is much more likely to be in response to the exaggerated permanent cavity of the projectile, which is greatly enhanced after striking the underlying facial skeleton.31–33,48 The key point for understanding the management of ballistic injuries is the permanent cavity, which involves all the tissues that are pushed aside or destroyed during the flight of the projectile, and is the site of the extent of the initial, or immediate, damage. The size and shape of the permanent cavity are determined by the density and anatomic characteristics of the tissue lying in the projectile’s path, velocity of the projectile, shape and characteristics of the projectile and, likely most importantly, the degree of deformation of the missile as it travels through the tissues.36–39
The type of firearm used has implications in regard to the wounding potential of the projectile. Generalized discussions of craniomaxillofacial wounding patterns center on handguns, rifles and shotguns. The wounding patterns of these weapons are unique and do not fall under the classic description of firearm-based injuries.28 The actual projectiles expelled by firearms are limited in type only by time and the imagination for description, such as hollow point, round nose, full metal jacket, alloy-jacketed, and Teflon-tipped (Fig. 27-6A). The components of a bullet provide a basic understanding of the principles of firearm injury (Fig. 27-6B). The projectile is the portion of the bullet that is expelled and strikes the victim.49 The composition of the projectile (e.g., soft lead, hollow point, full copper covering) has a direct correlation with the wounding potential of the weapon. As a projectile deforms after striking the victim, either as a result of metallurgic composition during manufacture or as a direct consequence of striking the underlying bone, the energy transfer to the patient and potential injury to associated tissues is increased.
The case is the container in which the projectile, propellant (gunpowder), and primer are packaged as a single unit for placement into the firing mechanism of the weapon. Wads are generally plastic frameworks with a paper or felt insert that holds the various pellets (projectiles) together in relation to the propellant to allow for accurate and safe release of all the projectiles simultaneously from the barrel. The propellant, or gunpowder, is the accelerant that actually allows for expulsion of the projectile from the weapon. The more propellant in a cartridge, as is seen in Magnum and rifle rounds, the greater velocity the projectile exhibits. The primer is the only portion of the bullet with an explosive charge. As the primer is struck by the firing pin of the weapon, the explosive charge is activated, igniting the propellant and sending the projectile on its flight. Although traditional concepts of ballistics teach that impact kinetic energy (KE) is equal to half the mass (m) of the projectile times velocity (v) squared (KE =  mv2), the increased energy transmitted from a high-velocity projectile does not necessarily translate to increased wounding capacity. Cunningham et al have suggested that modifications need to be used to correct the kinetic energy estimate of wounding potential for the type of tissue being struck by the projectile.10,33,39,50 They indicated that softer tissues, such as brain and muscle, should be associated with a lower exponent of injury (0.5) than harder tissue, such as bone, which would have a higher exponent (2.5) and therefore a higher likelihood of permanent injury. The corrected formula for estimating wounding capacity by kinetic energy should be KE =
mv2), the increased energy transmitted from a high-velocity projectile does not necessarily translate to increased wounding capacity. Cunningham et al have suggested that modifications need to be used to correct the kinetic energy estimate of wounding potential for the type of tissue being struck by the projectile.10,33,39,50 They indicated that softer tissues, such as brain and muscle, should be associated with a lower exponent of injury (0.5) than harder tissue, such as bone, which would have a higher exponent (2.5) and therefore a higher likelihood of permanent injury. The corrected formula for estimating wounding capacity by kinetic energy should be KE =  mv0.5 to KE =
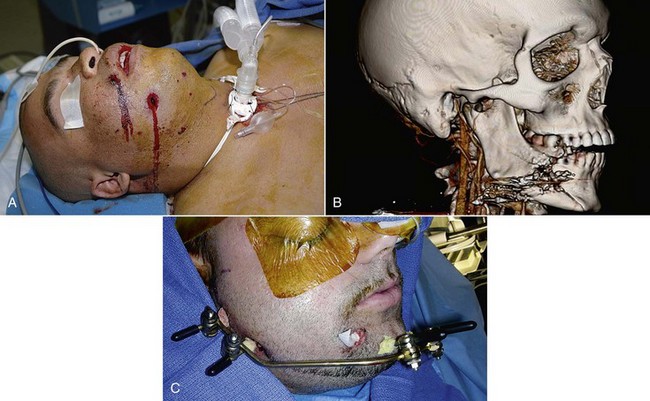
mv0.5 to KE =  mv2.5. Handguns are handheld firearms, with a barrel length generally 10.5 inches or less, which usually fire projectiles of a lower velocity and caliber.49 The characteristic low-velocity wound has a small rounded, or slightly ragged, entrance wound, causing fragmentation of teeth and bony comminution, often exhibiting no exit wound51,52 (Fig. 27-7). If an exit wound does occur, it is generally slit-shaped or stellate.
mv2.5. Handguns are handheld firearms, with a barrel length generally 10.5 inches or less, which usually fire projectiles of a lower velocity and caliber.49 The characteristic low-velocity wound has a small rounded, or slightly ragged, entrance wound, causing fragmentation of teeth and bony comminution, often exhibiting no exit wound51,52 (Fig. 27-7). If an exit wound does occur, it is generally slit-shaped or stellate.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses