Paranasal Sinus Diseases
Axel Ruprecht and Ernest W.N. Lam
The paranasal sinuses are the four paired sets of air-filled cavities of the maxillofacial complex, and they consist of the maxillary, frontal, and sphenoid sinuses and the ethmoid air cells. The maxillary sinuses are of particular importance to the dentist because of their proximity to the teeth and their associated structures. Abnormalities arising from within the maxillary sinuses can cause symptoms that may mimic diseases of odontogenic origin; conversely, abnormalities that arise in and around the teeth may affect the sinuses or mimic the symptoms of sinus disease. Because the paranasal sinuses may appear on many diagnostic images used in the practice of dentistry, the dentist should be familiar with variations in the normal appearances of the sinuses and the more common diseases that may affect them.
Normal Development and Variations
The paranasal sinuses develop as invaginations from the nasal fossae into their respective bones (maxillary, frontal, sphenoid, and ethmoid) and continue to enlarge until skeletal maturity. Consequently, the mucosal lining of the paranasal sinuses is similar to the lining found in the nasal cavity but with slightly fewer mucous glands. The epithelial cilia move these sinus secretions toward their respective communications, the ostia, with the nasal fossae.
The maxillary sinuses or antra are the first to develop in the second month of intrauterine life. An invagination develops in the lateral wall of the nasal fossa in the middle meatus, and the sinus cavity enlarges laterally into the body of the maxilla. At birth, each sinus is a thin, small slit, no more than 8 mm in length in its anteroposterior dimension. With time, the maxilla becomes progressively more pneumatized as the air cavity expands further into the bone both laterally under the orbits toward the zygomatic process and inferiorly into the alveolar process. Enlargement of the air space, or pneumatization, into the alveolar process superimposes the maxillary sinus and floor over the roots of the premolar or molar teeth to varying degrees on plain images.
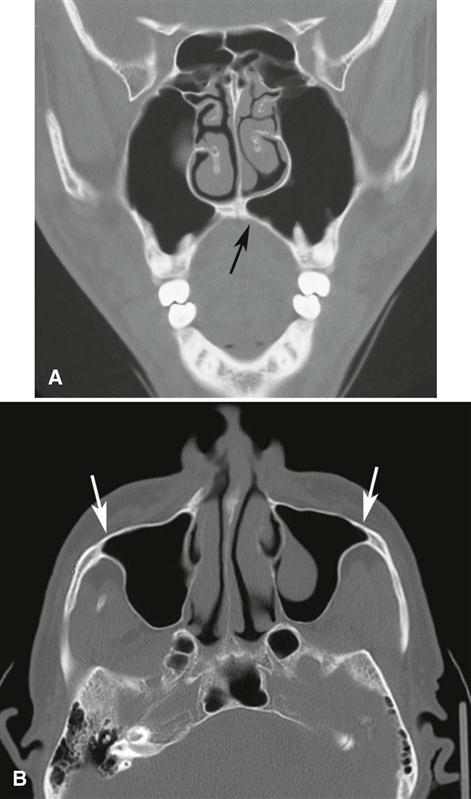
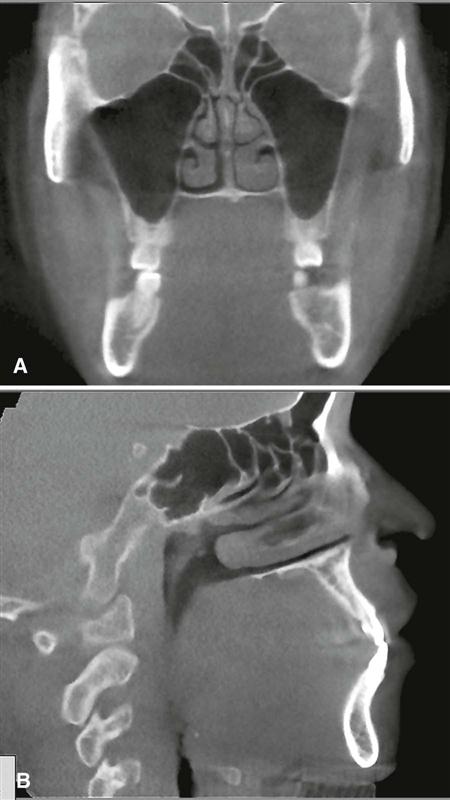
The radiographic appearance of the floor of the maxillary sinus is a thin, radiopaque line. Where the alveolar process of the maxilla is not well pneumatized, the floor of the sinus may not be visible on periapical images (Fig. 26-1, A), or it may be seen superior to the roots of the maxillary premolar or molar teeth (Fig. 26-1, B). With greater pneumatization of the alveolar process, the floor of the sinus may appear to undulate or drape over or around the roots of the teeth or be superimposed over the roots of the adjacent teeth, giving the false impression that the tooth roots have penetrated the sinus floor (Fig. 26-1, C and D). Closer examination of the periapical areas of the teeth in such instances reveals intact laminae durae and periodontal ligament spaces. In patients with considerable pneumatization of the alveolar process of the maxilla, the lamina dura of a premolar or molar tooth may form a portion of the sinus floor. Maxillary pneumatization may also extend into the palatal, zygomatic, and frontal processes of the maxilla, and this can be appreciated on plain images and advanced imaging examinations such as cone-beam computed tomographic (CBCT), computed tomographic (CT), or magnetic resonance (MR) imaging (Fig. 26-2). In some instances, the appearance of the normally pneumatized maxilla may be mistakenly confused with a benign space-occupying lesion, particularly on plain images (Fig. 26-3).
Hypoplasia of the maxillary sinuses occurs unilaterally in about 1.7% of patients and bilaterally in 7.2%. In these patients, the images of the affected sinus may appear more radiopaque than normal because of the relatively large amount of surrounding maxillary bone. The configuration of the maxillary sinus walls frequently helps to distinguish between a hypoplastic sinus and a sinus that is pathologically radiopaque. An occipitomental (Waters) view shows an inward bowing of the sinus wall resulting in a smaller than normal air cavity. In contrast, extensive enlargement of the maxillary and other paranasal sinuses is a well-known feature of acromegaly.
The development of the frontal sinus does not usually begin until the fifth or sixth year of life. This sinus either develops directly as extensions from the nasal fossae or develops from the anterior ethmoid air cells (see Fig. 26-4, B). In about 4% of the population, the frontal sinuses fail to develop. As with the other paranasal sinuses, the right and left frontal sinus cavities develop separately, and as they expand, they approach each other in the midline. In such instances, a thin bony septum may partially or completely separate the two asymmetric cavities. In adults, frontal sinus pneumatization may also extend posteriorly into the orbital roofs.
The sphenoid sinus begins growing in the fourth fetal month as invaginations from the sphenoethmoidal recesses of the nasal fossae. Located in the body of the sphenoid bone, the sinuses may be separated by a partial or complete bony septum that may result in sinus cavities that are asymmetric in size and shape. Similar to the other sinuses, the sphenoid sinuses may extend beyond the body of the bone into the dorsum sella, the clinoid processes, the greater or lesser wings, and the pterygoid processes. The ostium of the sphenoid sinus is a relatively large-diameter opening, which may explain why blockages of the sphenoid sinus ostium are uncommon (see the section on mucoceles later in this chapter).
The ethmoid air cells extend into the developing ethmoid bones during the fifth fetal month. They consist of multiple separate or interconnected air-filled chambers that border the medial and sometimes inferior aspects of the orbital cavities (Fig. 26-4, A and B). The number of air cells varies considerably, with each ethmoid bone containing 8 to 15 cells. In some cases, the ethmoid air cells may encroach into the neighboring maxillary, lacrimal, frontal, sphenoid, and palatine bones.
The function of the paranasal sinuses has been controversial. However, many authorities now believe the role of the paranasal sinuses is to insulate or protect deeper vital structures from external trauma.
Diseases Associated with the Paranasal Sinuses
The maxillary sinuses are of greatest concern to the dentist because of their proximities to the teeth and supporting structures. Therefore, the emphasis in this chapter is on diseases related to the maxillary sinus.
Definition
Diseases associated with the maxillary sinuses include diseases that originate primarily from tissues within the sinus (intrinsic diseases) and diseases that originate outside the sinus (most commonly diseases arising from odontogenic tissues) that either impinge on or infiltrate the sinus (extrinsic diseases). These types of diseases include inflammatory odontogenic disease, odontogenic cysts, benign and malignant odontogenic neoplasms, bone dysplasias, and trauma.
Clinical Features
The clinical signs and symptoms of maxillary sinus disease include a sensation of pressure, altered voice characteristics, pain on head movement, percussion sensitivity of the teeth, regional dysesthesia, paresthesia or anesthesia, and swelling and tenderness of the facial structures adjacent to the maxilla.
Applied Diagnostic Imaging
When maxillary sinus disease is suspected, it may be reasonable for the dentist to proceed with the initial radiologic investigation. A periapical image provides a detailed view of the periapical structures of the teeth and their relationships to the alveolar recess and floor of the maxillary antrum. Although this examination is limited, if the dentist suspects an abnormality, a maxillary lateral occlusal or panoramic image may be useful to obtain views of a greater region of the sinus as well as parts of the inferior, posterior, and anteromedial walls. In some cases, it may be difficult to compare the interior aspects of the right and left sinuses on the panoramic image because of overlapping of adjacent anatomic structures or ghost images.
If there are positive findings on these images, the patient should be referred to an oral and maxillofacial radiologist for a more comprehensive imaging examination. The occipitomental (Waters) skull projection is optimal for visualization of the maxillary sinuses, especially to compare internal radiopacities, and the frontal sinuses and ethmoid air cells. If the Waters view is made with the mouth open, parts of the sphenoid sinus may also be visualized.
Advanced imaging has become increasingly important for the evaluation of sinus disease and has virtually replaced plain images and conventional tomography for investigations of the paranasal sinuses. Because advanced imaging can produce multiplanar images through the sinuses, MDCT or CBCT examinations may contribute significantly to delineating the extent of disease, particularly in patients who have chronic or recurrent sinusitis. Coronal MDCT and CBCT imaging provide superior visualization of the ostiomeatal complex (the region of the ostia of the maxillary sinus and ethmoid air cells) and nasal cavities and for demonstrating any reaction in the surrounding bone to sinus disease. MRI provides superior visualization of the soft tissues, especially the extension of neoplasms developing or infiltrating into the sinuses or surrounding soft tissues, or the differentiation of retained fluid secretions from soft tissue masses in the sinuses.
Intrinsic Diseases of the Paranasal Sinuses
This section describes abnormalities that originate from tissues within the sinuses.
Inflammatory Disease
Inflammation may result from various causes, such as infection, chemical irritation, allergy, introduction of a foreign body, or facial trauma. The imaging changes associated with inflammation include thickened sinus mucosa, air-fluid levels, polyps, empyema, and retention pseudocysts. However, viral infections may not cause any imaging change in a sinus.
Mucositis
Synonym.
A synonym for mucositis is localized thickened sinus mucosa.
Disease Mechanism.
The mucosal lining of the paranasal sinuses is composed of respiratory epithelium and is normally about 1 mm thick. Normal sinus mucosa is not visualized on images; however, inflamed mucosa may increase in thickness 10 to 15 times, and this may be visualized with imaging. Localized inflammatory change is referred to as mucositis.
Clinical Features.
Many patients may be unaware of a change to their sinus mucosa, and these changes are often discovered as incidental findings on images made for other purposes. Consequently, the discovery of thickened mucosa in an individual who is otherwise asymptomatic does not imply that further investigations are warranted or that treatment is required.
Imaging Features.
Thickened mucosa is readily detectable in the image as a well-defined, noncorticated radiopaque band of increased radiopacity paralleling the bony wall of the sinus (Fig. 26-5).
Sinusitis
Disease Mechanism.
Sinusitis is a generalized inflammatory condition of the sinus mucosa caused by an allergen, bacteria, or a virus. Inflammatory changes may lead to ciliary dysfunction and retention of sinus secretions and sometimes blockage of the ostiomeatal complex. The term pansinusitis describes sinusitis affecting all the paranasal sinuses. In children with pansinusitis, the possibility of cystic fibrosis should be considered. Sinusitis is often categorized as acute or chronic based on the length of time that the disease is present. If the disease is present for 4 weeks or less, it is termed acute sinusitis; if it is present for more than 12 consecutive weeks, it is considered chronic. For sinusitis lasting from more than 4 weeks up to 12 weeks, the term subacute may be used.
Clinical Features.
Acute sinusitis is the most common of the sinus conditions that cause pain and is often a complication of the common cold. After a few days, nasal congestion accompanied by a clear discharge can increase, and the patient may complain of pain and tenderness to pressure or swelling over the involved sinus. The pain may also be referred to the premolar and molar teeth on the affected side and these teeth may develop sensitivity to percussion. In the case of a bacterial sinusitis, a green or greenish yellow discharge may accompany the other aforementioned signs and symptoms. In such circumstances, it is important that the teeth be ruled out as a possible source of the pain or infection.
Chronic maxillary sinusitis is a sequela of an acute infection that fails to resolve by 3 months. Generally, no external signs occur except during periods of acute exacerbations when increased pain and discomfort are apparent. Chronic sinusitis may develop with anatomic derangements, including deviation of the nasal septum and the presence of concha bullosa (pneumatization of the middle concha) that inhibit the outflow of mucus, or with allergic rhinitis, asthma, cystic fibrosis, and dental infections.
Imaging Features.
Thickening of sinus mucosa and the accumulation of secretions that accompany sinusitis reduce the air space of the sinus and cause it to become increasingly radiopaque. The most common radiopaque patterns that occur in the Waters view are localized mucosal thickening along the sinus floor, generalized thickening of the mucosal lining around the entire wall of the sinus, and near-complete or complete radiopacification of the sinus (Figs. 26-6 and 26-7). Such changes are best seen in the maxillary sinuses, but the frontal and sphenoid sinuses may be similarly affected. Scrutinizing the area around the maxillary ostium on plain images or CT images may reveal the presence of thickened mucosal tissue, which may cause blockage of the ostium. Mucosal thickening in just the base of the sinus may not represent sinusitis. Rather, it may represent the more localized thickening or mucositis that can occur in association with rarefying osteitis from a tooth with a nonvital pulp. However, this condition may progress to involve the entire sinus.
The image of thickened sinus mucosa may be uniform or polypoid. In the case of an allergic reaction, the mucosa tends to be more lobulated. In contrast, in cases of infection, the thickened mucosal outline tends to be smoother, with its contour following that of the sinus wall. The inability to perceive the delicate walls of the ethmoid air cells is a particularly sensitive sign of ethmoid sinusitis.
An air-fluid level resulting from the accumulation of secretions also may be present. Because the radiopacities of transudates, exudates, blood, and pathologically altered mucosa are similar, the differentiation among them relies on their shape and distribution. When present, fluid appears radiopaque and occupies the inferior or so-called dependent aspect of the sinus. The border between the radiopaque fluid and the relatively radiolucent air in the antrum is horizontal and straight, and a meniscus may be seen at the periphery where the fluid meets a sinus wall (see Fig. 26-6). Chronic sinusitis may result in persistent radiopacification of the sinus with sclerosis and thickening of the bony walls as the sinus periosteum is stimulated (Fig. 26-8).
The resolution of acute sinusitis becomes apparent on the image as a gradual increase in the radiolucency of the sinus. This can first be recognized when a small clear area appears in the interior of the sinus; the thickened mucous membrane gradually shrinks so that it begins to follow the outline of the bony wall. In time, the image of the mucous membrane is not visible, and the sinus appears normal. In chronic sinusitis, the changes to the sinus wall may persist.
Management.
The goals of treatment of sinusitis are to control the infection, promote drainage, and relieve pain. Acute sinusitis is usually treated medically with decongestants to reduce mucosal swelling and with antibiotics in the case of a bacterial sinusitis. Chronic sinusitis is primarily a disease of obstruction of the ostia; the goal is ventilation and drainage. Endoscopic surgery is often performed to enlarge obstructed ostia, or an alternative path of drainage is established.
Retention Pseudocyst
Synonyms.
Synonyms for retention pseudocyst include antral pseudocyst, benign mucous cyst, mucus retention cyst, mucus retention pseudocyst, mesothelial cyst, pseudocyst, interstitial cyst, lymphangiectatic cyst, false cyst, retention cyst of the maxillary sinus, benign cyst of the antrum, benign mucosal cyst of the sinus, serous nonsecretory retention pseudocyst, and mucosal antral cyst.
Disease Mechanism.
The term retention pseudocyst is used to describe several related conditions that result in the development of cystlike lesions that are not lined by epithelium. The pathogenesis of these lesions is controversial, but because their clinical and imaging features are similar, no attempt is made to distinguish between them. One etiology suggests that blockage of the secretory ducts of seromucous glands in the sinus mucosa may result in a pathologic submucosal accumulation of secretions, resulting in swelling of the tissue. A second theory suggests that the serous nonsecretory retention pseudocyst arises as a result of cystic degeneration within an inflamed, thickened sinus lining.
Clinical Features.
Retention pseudocysts may be found in any of the sinuses at any time of the year, although they may occur more often in the early spring or fall. This occurrence suggests that retention pseudocysts might be related to changes in seasonal allergies, colds, humidity, or temperature changes. Most studies have found that retention pseudocysts are more common in males.
A retention pseudocyst rarely causes any signs or symptoms, and the patient is usually unaware of the lesion. It often is noticed as an incidental finding on images obtained for other purposes. Retention pseudocysts may range widely in size—from the size of a fingertip to a size large enough to fill the sinus completely and make it radiopaque. However, when a pseudocyst completely fills the maxillary sinus cavity, it may prolapse (extrude) through the ostium and cause nasal obstruction or rupture as a result of abrupt pressure changes caused by sneezing or blowing of the nose, producing postnasal discharge; this may be the only clinical evidence of the presence of the pseudocyst. The pseudocyst may be present on an imaging examination of the maxillary sinus and be absent only a few days later, only to reappear on subsequent examinations.
The maxillary sinus is the most common site of retention pseudocysts. Pseudocysts occasionally are found in the sphenoid sinus and less often are found in the frontal sinuses and ethmoid air cells. Antral retention pseudocysts are not related to dental extractions or associated with periapical disease.
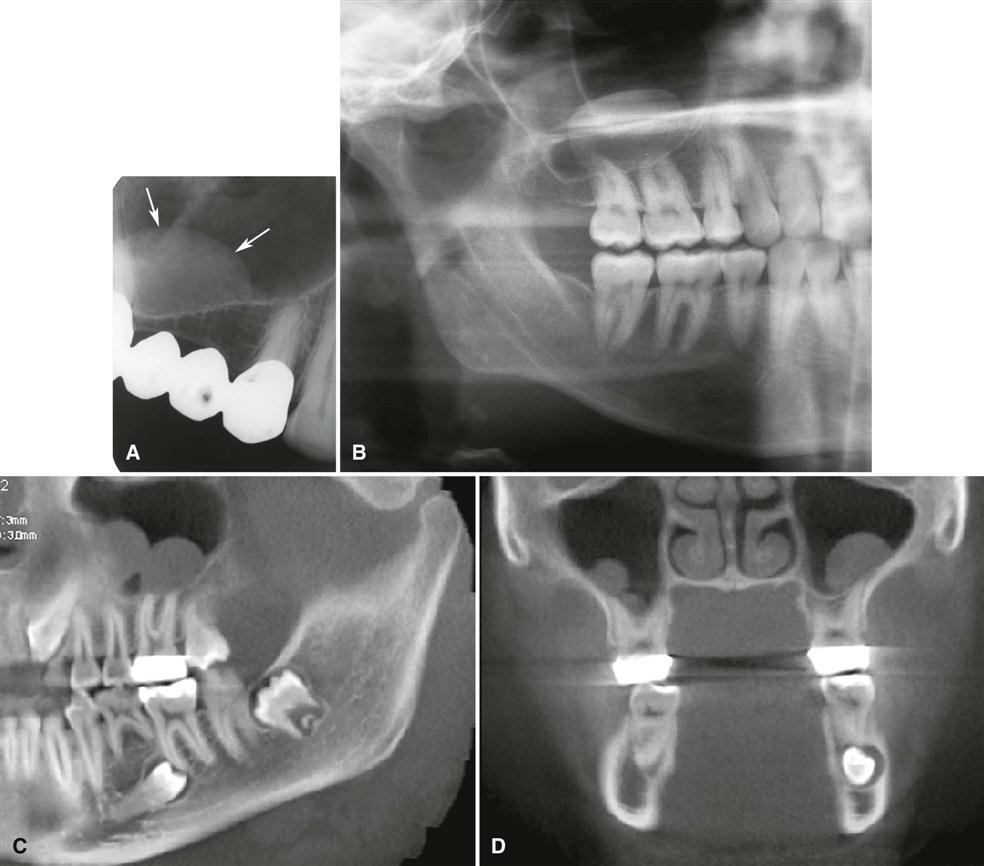
Imaging Features
Location.
Partial images of retention pseudocysts of the maxillary antrum may appear on maxillary posterior periapical images (Fig. 26-9, A), but they are best demonstrated on extraoral images (Fig. 26-9, B). One or more pseudocysts may occur within the same or different sinus cavities. These pseudocysts usually form on the floor of the sinus (Fig. 26-9, D), although they may form on any wall or the roof (Fig. 26-9, C).
Periphery and Shape.
Retention pseudocysts usually appear as well-defined, noncorticated, smooth, dome-shaped, mostly sessile radiopaque masses. Because the lesion originates from within the sinus, it does not have a radiopaque, corticated border.
Internal Structure.
The internal aspect is homogeneous and more radiopaque than the surrounding air of the sinus cavity (see Fig. 26-9, B). The radiopacity of the lesion is caused by the accumulation of fluid in the soft tissue lining of the sinus, which is relatively more radiopaque than air.
Effects on Surrounding Structures.
There are no effects on the surrounding structures. The adjacent sinus floor is always intact. When a retention pseudocyst occurs adjacent to the root of a tooth, the lamina dura surrounding the root is intact, and the width of the periodontal ligament space is unaffected.
Differential Diagnosis.
It is important to distinguish retention pseudocysts from antral polyps, odontogenic cysts, or neoplasms arising in the maxilla adjacent to the sinus; this can usually be done through imaging characteristics and by the patient’s history. The floor of the maxillary sinus may be displaced by a developing odontogenic cyst or neoplasm as the border of the lesion becomes coincident with the bony sinus floor. In some instances, periodic fenestrations can be seen through the bony sinus floor depending on the growth rate or aggressiveness of the cyst or neoplasm. The retention pseudocyst is dome-shaped but lacks the thin marginal radiopaque line representing the corticated border characteristic of the odontogenic cyst or neoplasm. For example, in the case of a radicular cyst, the lamina dura of the involved tooth or teeth is not intact in the apical area.
Antral polyps of infectious or allergic origin may be difficult to distinguish from retention pseudocysts, but when there is concurrent mucositis and multiple soft tissue masses, the possibility of polyps should be considered. Benign neoplasms may also mimic retention pseudocysts. If benign neoplasms originate from outside the sinus, they are separated from the cavity of the sinus by a radiopaque border, similar to odontogenic cysts. Malignant neoplasms may destroy the osseous border of the sinus, whether they arise from within the sinus or from the alveolar process. However, a malignant neoplasm is less likely to appear as dome-shaped as a retention pseudocyst.
Management.
Retention pseudocysts in the maxillary sinus usually require no treatment because they customarily resolve spontaneously without any residual effect on the antral mucosa.
Polyps
Disease Mechanism.
The thickened mucous membrane of a chronically inflamed sinus frequently forms into irregular folds called polyps. Polyposis of the sinus mucosa may develop in an isolated area or in many areas throughout the sinus.
Clinical Features.
Polyps may cause displacement or destruction of bone. In the ethmoid air cells, polyps may cause destruction of the medial wall of the orbit (lamina papyracea of the ethmoid bone) and an ipsilateral proptosis.
Imaging Features.
A polyp may be differentiated from a retention pseudocyst on an image by noting that a polyp usually occurs with a thickened mucous membrane lining because the polypoid mass is no more than an accentuation of the mucosal thickening. In the case of a retention pseudocyst, the adjacent mucous membrane lining is not usually apparent. If multiple retention pseudocysts are seen within a sinus, the possibility of sinus polyposis should be considered.
The image of the bone displacement or destruction associated with polyps may mimic a benign or malignant neoplasm. Because many />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses