Complementary and alternative medicine
Traditional medicine is widely practised across the world, particularly in Asian and African cultures. In the developed world, therapies that are not currently considered an integral part of conventional allopathic medical practice are termed complementary (when used in addition to conventional treatments) and alternative (when used instead of conventional treatments). Such therapies (complementary and alternative medicine – or CAM) include, but are not limited to, acupuncture, aromatherapy, chiropractic, colonic irrigation, diet fads (Ch. 27), faith healing, folk medicine, herbal (natural) medicine, homoeopathy, meditation, naturopathy, new-age healing, massage and music therapy.
During 2007, almost 40% of adults in the USA used CAM, the most commonly used therapies being non-vitamin, non-mineral, natural products and deep breathing exercises (http://www.cdc.gov/nchs/data/nhsr/nhsr012.pdf; accessed 30 September 2013). Over the preceding 5 years, there was increased use of acupuncture, deep breathing exercises, hypnotherapy, massage therapy, meditation, naturopathy and yoga, but use for colds showed a marked decrease. However, there is only limited evidence of efficacy for many CAM therapies. For instance, PubMed, the National Library of Medicine journal database, identified 40 systematic reviews involving acupuncture, massage therapy, naturopathy or yoga, only 10 of which (25%) provided sufficient evidence to conclude that a given therapy was effective for a given condition. These were acupuncture for knee pain, insomnia and nausea or vomiting, and acupuncture and yoga for back pain; both acupuncture and massage therapy are included among recommended therapies for back pain. CAM is taken increasingly seriously in the West and there is a National Centre for Complementary and Alternative Medicine (NCCAM) in the USA.
Since there is some evidence of increasing use by the public and of efficacy, this chapter focuses on forms of traditional medicine, acupuncture, herbal medicines and probiotics. Herbal alternatives to hormone replacement therapy are discussed in Chapter 25; omega-3 and omega-6 are discussed in Chapter 27.
Traditional Chinese Medicine
Traditional Chinese medicine (TCM; http://nccam.nih.gov/health/whatiscam/chinesemed.htm, accessed 30 September 2013) views how the body works, what causes illness and how to treat illness, differently from Western views. TCM is typically delivered by a practitioner who uses acupuncture, herbs and other methods to treat a wide range of conditions. Other TCM practices include cupping, dietary therapy, massage, mind–body therapy and moxibustion (the burning of mugwort, a small herb). Acupuncture has the largest body of evidence and is considered safe if practised correctly. Some Chinese herbal remedies may be safe; others may not be.
Acupuncture
A limited number of randomized controlled trials (RCTs) support acupuncture as a possible treatment for a range of conditions that include anxiety, cancer and chemotherapy-induced nausea, depression, insomnia, migraine, musculoskeletal pain and postoperative pain. However, there is inadequate evidence of benefit in conditions such as asthma, dysphagia, epilepsy, schizophrenia, smoking cessation or stroke.
Dental aspects
There are several publications but few RCTs on acupuncture used for orofacial conditions (Table 26.1). Efforts have been made to clarify mechanisms but consensus has yet to be reached. Any efficacy may be explained by possible release of endogenous opiates (beta-endorphin, enkephalin, endomorphin and dynorphin; Ch. 10) during acupuncture. The serotoninergic descending inhibitory pathway is an alternative suggested mechanism. The autonomic nervous system and resultant inflammatory reflex might be part of antihyperalgesia elicited by acupuncture.
Table 26.1
Acupuncture in orofacial conditions (benefit proved)
| Probably | Possibly | Inconclusive |
| Dental pain | Dental local anaesthesia – reduced time to onset | Bell palsy |
| Postoperative or chemotherapy-induced nausea/vomiting | Gag reflex | Burning mouth sensation |
| Postoperative pain | Hyposalivation | Mouth ulceration |
| Temporomandibular joint pain | Neck pain | Sensory loss |
| Sinusitis |
Ayurvedic Medicine
Ayurvedic medicine (Ayurveda; http://nccam.nih.gov/health/ayurveda/introduction.htm; accessed 30 September 2013) originated in India. Its aim is to integrate and balance the body, mind and spirit because it is believed that this helps prevent illness and promote wellness. Many therapies employed in Ayurvedic medicine are also used on their own as CAM – for example, herbs, massage and specialized diets. Some of the products may be harmful (causing adverse effects or interacting with conventional medicines). Different systems used to treat oral diseases, individually or in combinations, include Acacia chundra Willd, Adhatoda vasica Nees, Mimusops elengi L., Piper nigrum L., Pongamia pinnata (L.) Pierre, Quercus infectoria Olivier, Syzygium aromaticum L., Terminalia chebula Retz and Zingiber officinale Roscoe.
Cam in other Cultures
Details of African, American Indian, Latin American, Caribbean and other important CAM can be found at: http://www.ncbi.nlm.nih.gov/pmc/journals/970/ and http://americanindianhealth.nlm.nih.gov/ (both accessed 30 September 2013).
Herbal Medicines
Many conventional drugs that have been proven to be effective originated from plant sources. Examples include aspirin (from willow bark), digoxin (foxglove), morphine (opium poppy) and quinine (cinchona bark). However, natural does not signify safe. Some plant products (e.g. opioids, cocaine and peyote) are addictive (Ch. 34) and many are highly toxic; for example, some Chinese weight-loss herbs are nephrotoxic, and kava-kava (Piper methysticum) is hepatotoxic. Chamomile, liquorice root, quassia and red clover all contain coumarin derivatives and can provoke a bleeding tendency. Some other herbal products may impair platelet aggregation, thus prolonging bleeding (Table 26.2). Herbals that pose a risk for cardiac patients are shown in Box 26.1.
Table 26.2
Herbal products that may inhibit haemostasis
| Herbal | Source |
| Bilberry | Vaccinium myrtillus |
| Bromelain | Anas comosus |
| Cat’s claw | Uncaria tomentosa |
| Devil’s claw | Harpagophytum procumbens |
| Dong quai | Angelica sinensis |
| Evening primrose | Oenothera biennis |
| Feverfew | Tanacetum parthenium |
| Garlic | Allium sativum |
| Ginger | Zingiber officinale |
| Ginkgo biloba | Ginkgo biloba |
| Ginseng | Panax ginseng |
| Grape seed | Vitis vinifera |
| Green tea | Camellia sinensis |
| Horse chestnut | Aesculus hippocastanum |
| Turmeric | Curcuma longa |
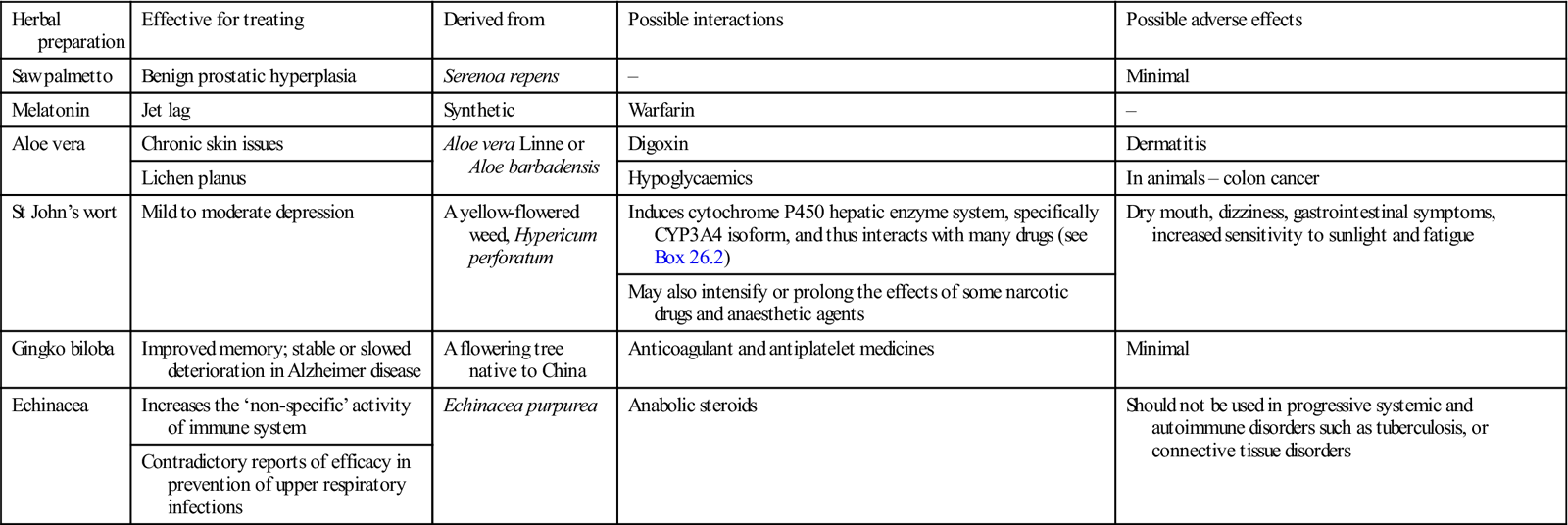
Some herbal drugs appear to be effective and fairly safe, and there are reliable published data supporting a potential medicinal role for aloe vera, melatonin, saw palmetto and St John’s wort (Table 26.3). Reliable published data on efficacy are weaker for gingko biloba and alpha-lipoic acid, and are contradictory for valerian and echinacea. Research into the safety and efficacy of most herbals has been limited because of product variability, lack of controlled studies and few legal controls (Appendices 26.1 and 26.2).
Table 26.3
Herbal preparations and supplements of proven efficacy
< ?comst?>
| Herbal preparation | Effective for treating | Derived from | Possible interactions | Possible adverse effects |
| Saw palmetto | Benign prostatic hyperplasia | Serenoa repens | – | Minimal |
| Melatonin | Jet lag | Synthetic | Warfarin | – |
| Aloe vera | Chronic skin issues | Aloe vera Linne or Aloe barbadensis | Digoxin | Dermatitis |
| Lichen planus | Hypoglycaemics | In animals – colon cancer | ||
| St John’s wort | Mild to moderate depression | A yellow-flowered weed, Hypericum perforatum | Induces cytochrome P450 hepatic enzyme system, specifically CYP3A4 isoform, and thus interacts with many drugs (see Box 26.2) | Dry mouth, dizziness, gastrointestinal symptoms, increased sensitivity to sunlight and fatigue |
| May also intensify or prolong the effects of some narcotic drugs and anaesthetic agents | ||||
| Gingko biloba | Improved memory; stable or slowed deterioration in Alzheimer disease | A flowering tree native to China | Anticoagulant and antiplatelet medicines | Minimal |
| Echinacea | Increases the ‘non-specific’ activity of immune system | Echinacea purpurea | Anabolic steroids | Should not be used in progressive systemic and autoimmune disorders such as tuberculosis, or connective tissue disorders |
| Contradictory reports of efficacy in prevention of upper respiratory infections |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Aloe Vera
Aloe vera, derived from Aloe barbadensis Miller, contains many constituents, some of which purportedly have anti-inflammatory, antiseptic and/or analgesic properties. These include:
■ vitamins: A (beta-carotene), C, E, B12, folic acid and choline
■ minerals: calcium, chromium, copper, selenium, magnesium, manganese, potassium, sodium and zinc
■ sugars: monosaccharides (glucose and fructose) and polysaccharides (glucomannans/polymannose)
■ fatty acids: cholesterol, campesterol, beta-sitosterol and lupeol
Aloe may have healing and protective effects against radiation damage, and anti-inflammatory, antiviral and antiseptic properties. There are reports of efficacy in seborrhoeic dermatitis, psoriasis, herpes, burns, wound healing, pressure ulcers, mucositis, radiation dermatitis, acne, lichen planus and aphthous stomatitis.
Aloe may cause redness, burning, a stinging sensation and, rarely, dermatitis. Abdominal cramps, diarrhoea, red urine, hepatitis, dependency or worsening of constipation are also possible. Its laxative effect may cause electrolyte imbalances (low potassium levels). Prolonged use (in animals) has reportedly increased the risk of colorectal cancer.
Oral aloe is not recommended during pregnancy due to theoretical stimulation of uterine contractions, and if taken by breast-feeding mothers it may sometime causes gastrointestinal distress in the nursing infant. Aloe reduces the effectiveness and may increase the adverse effects of digoxin and digitoxin, due to its potassium-lowering effect. It decreases blood sugar levels and thus may interact with hypoglycaemic drugs and insulin. Aloe should not be taken for 2 weeks prior to any surgical procedure, as it may cause increased bleeding.
Further information on aloe is available at: http://umm.edu/health/medical/altmed/ (under ‘Herb’ and ‘Herb Interaction’) and http://nccam.nih.gov/health/aloevera (both accessed 30 September 2013).
Gingko Biloba
The flavonoids found in ginkgo may help prevent or reduce retinal problems and age-related macular degeneration; they may also enhance neuropsychological/memory processes, and possibly are effective in Alzheimer disease, improving cognitive performance, global function and activities of daily living, and, at least in vitro, inhibiting amyloid-beta aggregation and caspase-3 activation (Ch. 13). Meta-analyses comparing ginkgo with acetylcholinesterase inhibitors in Alzheimer disease have shown similar clinical efficacy, with an additional safety benefit for ginkgo. Ginkgo might cause early labour; it might also interfere with diabetes management, provoke seizures or cause a bleeding disorder.
Ginkgo can interact with some medications, including anticonvulsants, antidepressants (SSRIs – may increase the risk of serotonin syndrome), antihypertensives, and drugs such as warfarin, clopidogrel, aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs). It is recommended that ginkgo be stopped at least 2 weeks before surgery.
More information is available at: http://umm.edu/health/medical/altmed/herb/ginkgo-biloba and http://www.nlm.nih.gov/medlineplus/druginformation.html (both accessed 30 September 2013).
Melatonin
Melatonin taken in the evening in the new time zone will reset the biological clock and alleviate (or prevent) symptoms of jet lag. Melatonin helps determine when a woman starts to menstruate, the frequency and duration of menstrual cycles, and when a woman stops menstruating (meno/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


