Salivary Glands
In this chapter we will attempt to describe only the histology of salivary glands. For the description of size, location, and function of these glands, refer to Chapter 33.
COMPONENTS OF A SALIVARY GLAND
As discussed in Chapter 17, salivary glands arise from a cord of epithelium growing into the underlying connective tissue, and the cord later forms a tube. At the end of this tube a cluster of secretory cells forms, and these clusters, which look like bunches of grapes, will have end pieces that are either round or tubelike.
Acini
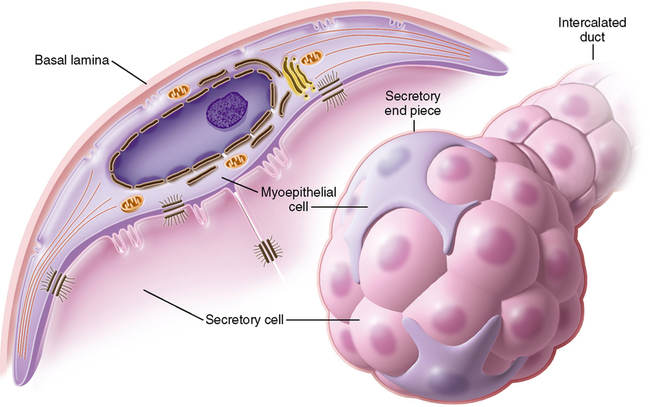
The secretory end pieces are known as acini. There are two kinds of acinar cells, mucous acini and serous acini. Although these cells form a grapelike or tubular endpiece, in cross section they are described as pyramidal cells (Fig. 25-1). The outer edge or base of the cells rests on a basement membrane between the cells and the connective tissue. Within this connective tissue are the nerves and blood vessels necessary for the various aspects of cellular activity. The apex of the cells faces the center of the tube or grapelike structure. The base of the cells is surrounded by connective tissue, and partially surrounding each secretory acinus is a myoepithelial cell (Fig. 25-2). This cell has long cellular projections, resembling a squid. It also has the ability to contract like a muscle. Hence the prefix myo, meaning muscle. These projections surround the acinus, and when the myoepithelial cell contracts, it squeezes the acinus and aids in the secretion of saliva that has accumulated in the hollow center of the acinus and helps move it out the duct system. All types of acini—mucous, serous, and seromucous—secrete their products through the process of merocrine secretion.
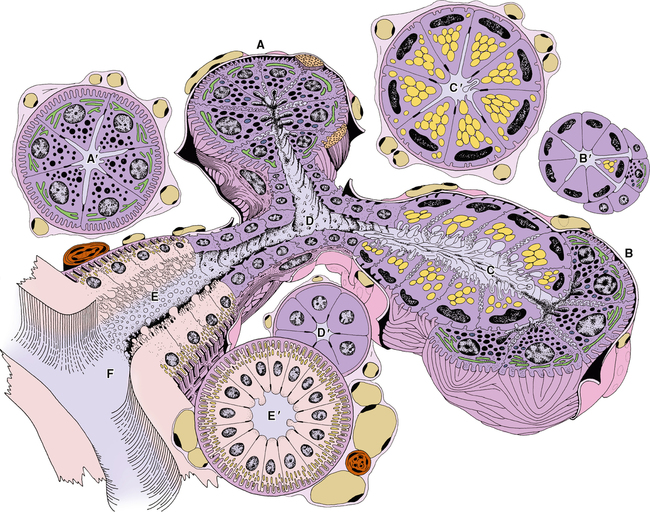
Seromucous acini
In glands that have both mucous and serous components, you can see the separate types of acini, and you can also see them joined together as mixed or seromucous acini. In a seromucous acinus, the mucous cells form a tubelike structure, and on the end of the tube a group of serous cells forms into a half-moon cluster. These are referred to as serous demilunes. The serous demilune cells secrete their product between the cell walls of the underlying mucous cells and their secretion enters the lumen of the gland. As the term seromucous suggests, these acini produce both mucous and serous secretions (see Fig. 25-1).
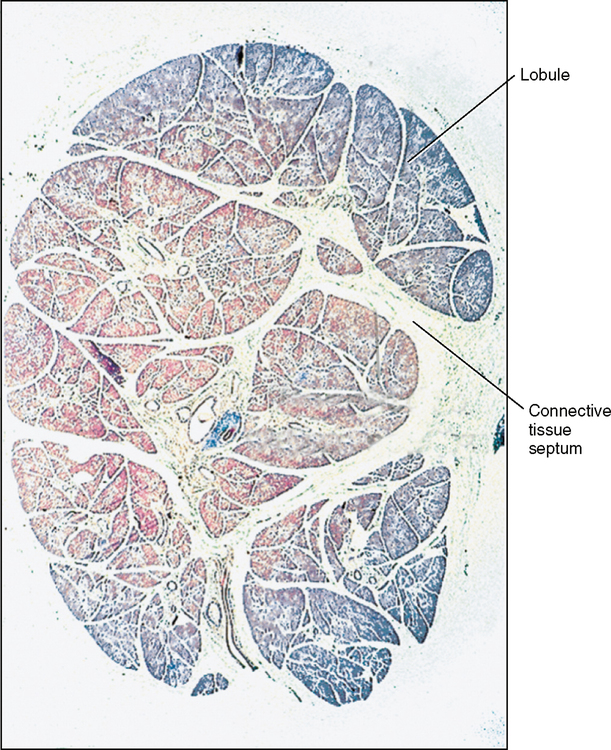
Connective Tissue Capsule
A salivary gland is surrounded by a connective tissue capsule. The connective tissue not only surrounds the gland but also sends partitions into the gland carrying nerves and blood vessels with it and dividing the gland into lobes and smaller units called lobules (Fig. 25-3).
Duct System
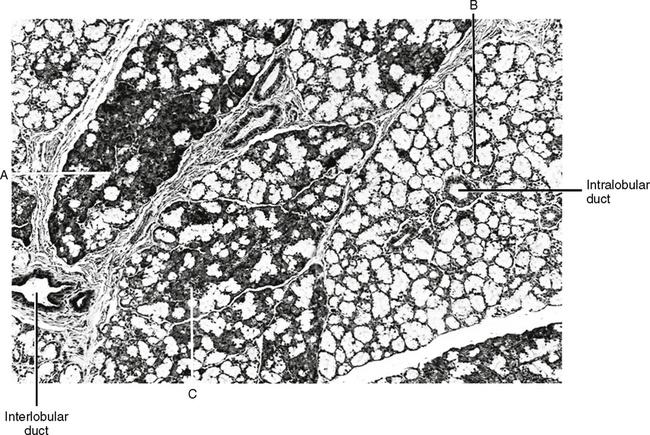
Intralobular ducts
Striated (secretory) ducts.
Intralobular striated ducts are so named because the bases of the cells within these ducts appear to be striped. The basal cell membrane has infoldings in which mitochondria become trapped and aligned between the infoldings. These mitochondria can be stained, causing a striped appearance. These ducts are also called secretory because, as the salivary fluid passes through them, their content is modified. Water and various substances such as sodium, potassium, chloride, and other ions are reabsorbed by being secreted out of the basal end of the cell where they are picked up again by the capillaries and lymphatic vessels. This function is important because it conserves water and electrolytes (see Fig. 25-1).
Interlobular ducts.
Interlobular ducts lie within the connective tissue between lobules of the gland. Some of these are striated like the striated intralobular ducts and generally are found only at the beginning of the interlobular ducts and are secretory, but most of them are nonstriated and large. These nonstriated ducts are generally referred to as excretory ducts. These ducts do not modify the salivary secretions but simply carry them out of the gland and to the surface tissues of the oral cavity (Fig. 25-4).
CONTROL OF SECRETIONS
Secretory control comes from the autonomic nervous system, particularly the parasympathetic nervous system (see Chapter 34). The control of secretion is tied to chewing, taste, and smell. Each of these is capable of modifying the amount and consistency of the salivary secretions.
FORMATION OF SALIVA
Saliva is formed within the endoplasmic reticulum of individual cells. If you remember from Chapter 17, the control of production within the endoplasmic reticulum comes from the DNA in the nucleus via the varying types of RNA. The future saliva is packaged by a membrane within the Golgi apparatus and moves out into the cytoplasm of the mucous or serous acini. The apical end of the cell accumulates these granules of future saliva, when the gland is stimulated by the parasympathetic nervous system, the granules move to the apical cell membrane, fuse with it, release their substance into the center lumen of the acini. From there the secretion moves out through the intercalated ducts into the striated, intralobular ducts and the striated, interlobular, and extrinsic ducts opening into the oral cavity.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses