Diagnosis and Management of Traumatic Salivary Gland Injuries
Trauma to the facial soft tissues and fractures of the maxillofacial complex may involve the salivary structures, but the relative incidence of injury to the salivary structures is low. Salivary gland injuries are usually associated with penetrating injuries or complex fractures of the facial bones.1,2 Salivary gland trauma can be classified as acute (blunt, lacerating, avulsion, or blast injuries) or chronic (inflammatory damage associated with infection, foreign bodies, sialoliths, or irradiation). Management of salivary gland injuries may vary according to factors such as the mechanism of injury, site of injury, degree of contamination, associated injuries, and general medical status of the patient. Lacerations in the cheek region posterior to the anterior border of the masseter muscle along a plane from the tragus of the ear to the middle of the upper lip (Fig. 24-1) may involve the parotid gland or duct, various branches of the facial nerve, and the facial artery and veins. Soft tissue injury in the floor of the mouth or beneath the mandible can damage the submandibular or sublingual glands, their associated ducts, or both. However, the incidence of injury to these salivary glands is lower than that for the parotid gland because of the protection of these salivary structures by the body of the mandible.
Salivary gland injuries can be serious and frequently associated with long-term morbidity. Delay or failure to diagnose may result in morbidity secondary to soft tissue scarring and disfigurement, sialocele, cutaneous fistula, or gustatory sweating associated with Frey’s syndrome.3,4 Surgical and nonsurgical approaches are used in the treatment of salivary gland and ductal injuries. Nonsurgical approaches are generally used only when the gland parenchyma is contused but the ductal structures remain intact. Surgical techniques are used to repair extensive injuries. Unfortunately, injuries to the salivary glands and/or supporting structures are often overlooked or underestimated in patients who have suffered significant or massive facial trauma. Thorough assessment and proper management of these injuries can prevent costly and unpleasant sequelae as acute treatment is usually much less difficult than late management.5,6
Anatomy
Parotid Gland and Duct
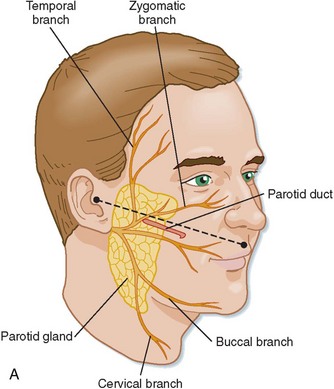
The parotid gland is a unilobar structure with superficial and deep portions. These two segments of the gland are connected by a small isthmus, within which lies the facial nerve. The gland is encapsulated by a fascia formed by a splitting of the superficial layer of the deep cervical fascia. The bulk of the parotid gland overlies the ramus of the mandible and is bounded superiorly by the zygoma and anteriorly by the masseter while posteriorly abutting the external auditory canal and the anterior superior aspect of the sternocleidomastoid muscle. The parotid tail curves posteriorly around the mandibular ramus and is rarely involved in traumatic injury. The parotid duct, or Stensen’s duct, exits from the anterolateral portion of the gland and passes beyond the anterior border of the masseter muscle, parallel with a plane drawn from the tragus of the ear to the midpoint of the upper lip. Approximately 1 cm anterior to the anterior border of the masseter muscle, the duct turns medially and penetrates the buccal fat pad and buccinator muscle, opening into the mouth at the level of the maxillary second molar. The facial nerve emerges from the stylomastoid foramen, passes into the substance of the gland, and subdivides into multiple branches that emerge anteriorly from the gland substance. Stensen’s duct is divided into the glandular portion, the proximal (masseteric) portion and a distal (buccal) portion.7 Generally, the buccal branch of the facial nerve can be found 5 to 10 mm below the parotid duct as it exits the gland. The nerve and duct are especially vulnerable to injury as they pass relatively unprotected over the superficial surface of the masseter muscle and exit the anterior portion of the parotid gland before descending within the fibers of the orbicularis oris and buccinator muscles.4,8 Several vascular structures are associated with the parotid gland, including the retromolar and external jugular veins and superficial temporal, external carotid, and facial arteries.
Submandibular Gland and Duct
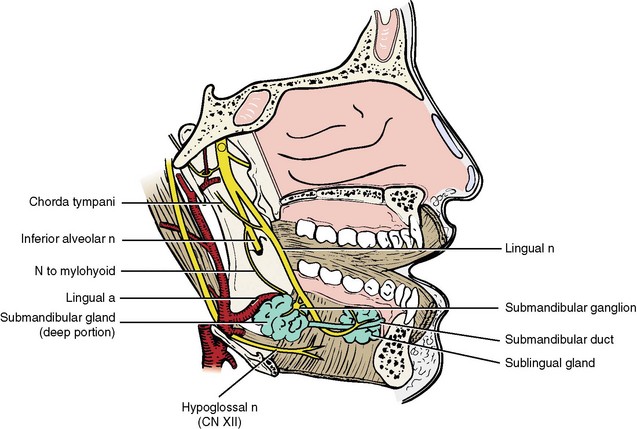
The submandibular gland lies below and in front of the angle of the mandible and occupies most of the posterior portion of the submandibular triangle. The gland lies deep to the platysma muscle, bounded anteriorly and inferiorly by the digastric muscle, the myohyoid muscle deep, and the hypoglossus muscle posteriorly. The greater part of the gland is superficial, but it folds around the posterior border of the mylohyoid muscle so that a small portion of the gland is found in the posterior floor of the mouth. The facial artery is intimately associated with the superficial portion of the gland. The submandibular duct, or Wharton’s duct, arises from the deep portion of the gland, is about 5 cm long, and has relatively thin walls and a constricted orifice. The duct leaves the submandibular triangle by passing above the posterior border of the mylohyoid muscle traversing along the floor of the mouth and opening in the anterior floor of mouth. In the floor of the mouth, the duct passes from lateral to medial on its way to the sublingual caruncle. Here, the duct has an intimate relation to the lingual nerve, which crosses it twice on its forward path (Fig. 24-2).9,10 The facial vein and artery are in close association with the submandibular gland and generally lie just posterior to the gland. The marginal branch of the facial nerve provides function to the depressor muscles of the lower lip and runs over the fascia superficial to the facial artery, facial vein, and gland and can extend to the most inferior level of the gland.
Sublingual Gland and Duct
The sublingual gland is the smallest of the three major salivary glands. It is narrow and flattened and lies below the mucosa bilaterally in the floor of the mouth, above the mylohyoid muscle. About 12 small sublingual ducts (ducts of Rivinus) emanate from the superior border of the gland and open separately in the floor of the mouth.10–12
Minor Salivary Glands
A discussion of the anatomy of salivary glands would not be complete without mention of the minor salivary glands. Minor salivary glands provide the bulk of lubrication for the mucosal surfaces of the oral cavity. These glands are located throughout the oral cavity, with the majority in the palate, the labial and buccal mucosae, the ventral surface of the tongue (Blandin and Nuhn’s glands), and the alveololingual glands in the lateral floor of the mouth. These minor glands lack a well-developed ductal system. Instead, these glands, which are located in the submucosal layer, have short ducts that open directly on the mucosal surface.10,13
Mechanism of Salivary Gland and Ductal Injuries
Sharp penetrating trauma is the usual mechanism that results in acute injury to the salivary glands and surrounding anatomical structures. Lewis and Knottenbelt have reported the incidence of parotid ductal injury as 0.21% (33 of 15,419) of all trauma cases evaluated over a 6-month interval, with most of these injuries being assaults with a knife or bottle.1 The most common cause of parotid gland injury is penetrating trauma from assault weapons or broken glass from a bottle or an automobile windshield.3 The largest documentation of salivary gland injury in the literature was reported by Morestin, who published his World War I experience with 62 parotid gland injuries.14 Blunt or compressive injury to the salivary glands is rare, usually requires significant amount of force that results in injury to the facial bones and facial soft tissues, and typically is associated with motor vehicle accidents (MVAs), but also has been reported from sports-related injuries, strangulation, blows from fists or feet, and excessive manipulation.15,16 Blunt trauma may result in the formation of a parenchymal contusion, hematoma, and sometimes a sialocele or a mucocele. This type of injury usually involves the parotid gland because of the protective nature of the mandible body for the submandibular and sublingual glands.17 However, rupture of major salivary glands can occur after blunt force, even in the absence of a cutaneous defect or laceration.15,18 The demographics of salivary gland injury are similar to those of other maxillofacial injuries in that the incidence is greater for men in the third decade of life.1,3,19 In a collective review of 32 patients by Tachmes et al, 56.3% of ductal injuries were acute, whereas the remainder appeared several days following the injury with a sialocele, fistula, or both, often with associated superinfection.2
Diagnosis of Salivary Gland Injuries
The diagnosis of salivary gland injury starts with increased suspicion of a potential injury based on the location and mechanism of trauma. The history and physical examination often provide useful information in the workup of possible salivary gland injury. Questions should be directed toward the presence of any suspicious swelling or drainage from the wound that might represent saliva, as well as the effects of food if the patient is taking an oral diet. Any penetrating cheek injury has the potential to involve the parotid gland and duct, the facial nerve, or all these structures. Figure 24-3 demonstrates a useful anatomic classification of parotid duct injuries first described by Van Sickels.7 Site A represents the most proximal portion of the duct, where it emerges from the substance of the parotid gland to the posterior edge of the masseter muscle. Site B is directly over the masseter muscle. In this location, the duct is relatively straight, superficial, and unprotected by any other overlying structure. Consequently, site B is the most common location of duct injury and the easiest to repair.1 Lastly, site C represents the portion of the duct distal to the anterior border of the masseter muscle, which subsequently dives into the substance of the buccinator muscle to terminate in the mouth adjacent to the maxillary second molar.
Parotid duct injuries are not easily diagnosed and are often missed on initial examination.1,19 In addition, other severe traumatic injuries are often associated with parotid duct injuries. Thus, delay in diagnosis of salivary injury is common and, if diagnosis is made, immediate repair is often postponed until the patient is stable.2,3 When the patient’s condition permits, the optimal sequence of treatment for suspected parotid gland ductal injury should include the following20,21:
• Detailed history and physical examination.
• Complete otologic examination when injury to the parotid gland is suspected.
• Palpation of the skeletal support of the face and the temporomandibular joints.
• Functional testing of each branch of the facial nerve (the administration of local anesthetic should be delayed until this examination is completed).
• Control of hemorrhage with pressure until adequate exploration of the wound under general anesthetic can be attempted; blind attempts to control bleeding should be avoided because the main blood vessels to the parotid gland lie deep to the facial nerve.
• In deeply penetrating injuries to the parotid gland, one must rule out injury to the carotid artery and a thorough neurologic examination must be undertaken. Repeat examination is indicated if the patient is intoxicated or unable to participate with the examiner.
• Emergent exploration of the wound if nerve or ductal injury is suspected.
Inspection of the injury and surrounding structures should be compared with the contralateral side for symmetry. After control of hemorrhage, a complete examination consists of attempting to identify collections of clear fluid in the depths of the wound. The sensitivity of this examination can be improved by pressing on the gland to express saliva into the field. When injuries are suspected with the submandibular gland, an assessment of tongue sensation and mobility may be helpful. Facial nerve function can be assessed with a nerve stimulator to help determine if the nerve is intact. Ductal injuries can best be delineated by direct inspection following cannulation of the duct with a lacrimal probe from its distal oral opening. Retracting the cheek wall in an outward direction, which straightens the sharp bend in the distal duct, can facilitate cannulation of Stensen’s duct. Retrograde injection of methylene blue can be used to aid in the diagnosis of ductal injury when inspection and probing fail to locate the duct. The duct opening is located intraorally and cannulated with a small gauged angiocatheter. A small amount of methylene blue is injected retrograde while observing the wound. Areas of extravasation can then be explored for ductal injury. A small amount should be injected because an excessive amount of dye in the wound can make for difficult evaluation and identification of stained anatomic landmarks.6,22,23 Saline, sterilized milk,24 or propofol solution has been advocated to assess the integrity of the duct and avoid the staining problems associated with the use of methylene blue.
Radiographic imaging can been used to support the clinical suspicion of salivary gland and ductal injury. Magnetic resonance imaging (MRI) has been the standard technique for imaging soft tissue pathology, including infections, but is not the study of choice for salivary gland trauma because it is difficult to delineate the integrity of the ductal system. Sialography with a water-soluble contrast medium remains a highly sensitive test of ductal abnormalities, with or without (Fig. 24-4) computed tomography (CT) imaging.13,17,25–27 Direct visualization of ductal filling under fluoroscopy can be useful, particularly using digital subtraction techniques. Cannulation of the parotid duct is normally straightforward, but access to the submandibular duct, especially in the trauma patient, may be difficult and its use with possible sublingual gland injury is not possible. Several authors have argued that the study of sialography, although costly and time-consuming, is important because it can delineate the exact location of glandular and ductal injuries, which has significant prognostic implications.1,3,28 Patients with facial trauma may also have concomitant injuries that prohibit transferring the patient to the radiology department for a lengthy study. Sialography is best used in cases that present some time after the traumatic event or in which ductal injury may have been overlooked.23 Sialography is also useful in the postoperative period to evaluate the results of treatment. If cannulation of the duct is unsuccessful, salivary gland function may be quantified by time-activity curves with 99mTc-pertechnetate scintigraphy and may distinguish between the functioning, obstructed, and nonfunctional gland.29 MRI sialography is an imaging technique using heavily T2-weighted sequences that is performed without the injection of a contrast medium and is considered a noninvasive, painless, and safe technique. Ductal injuries can be demonstrated by MRI sialography, which is dependent on stimulated ductal salivary flow as the contrast medium, and correlates well with or even improves on conventional sialography.24,30
Treatment of Salivary Gland Injuries
Specific recommendations on the management of ductal injury remain controversial. There is a consensus in the literature that acute parotid injuries should be explored primarily and the injured structures repaired, if possible. The aims of primary repair of salivary gland injuries should be the reapproximation of anatomic structures and return of normal function. Nonsurgical management of parotid duct injuries has been supported by Lewis and Knottenbelt, who reported their experience with 19 patients with a confirmed parotid duct injury. Nine patients had an uncomplicated duct healing and the remaining patients developed a sialocele or fistula that eventually resolved without surgical management.1
Minor Salivary Gland Injuries
Most minor salivary gland injuries occur during penetrating intraoral trauma. Appropriate treatment during the closure of intraoral lacerations includes the removal of any traumatized minor salivary glands within the wound. Complications of such intraoral or labial injuries may result in mucus retention phenomena (or mucocele; Fig. 24-5) caused by extravasation of fluid into the surrounding tissue from injury to the duct of a minor salivary gland. The treatment of this complication is accomplished by aggressive removal of the involved and surrounding minor salivary glands and the associated fluid-filled cavity, followed by primary closure of the mucosa.9,13
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses