Nasal Fractures
Evaluation and Management
Nasal trauma is a common occurrence in pediatric and adult patients because of the exposed and central position of the nose on the face.1–4 There is a broad spectrum of primary and secondary nasal trauma deformities that the craniomaxillofacial surgeon must be able to address. This chapter reviews the evaluation and treatment of nasal trauma and secondary nasal deformities.
Epidemiology
Nasal fractures are the most common facial fractures seen and occur at least twice as often in males as in females.1–6 The high frequency of nasal fractures can be attributed to its prominent location in the facial skeleton and the comparatively smaller amount of force needed to produce a fracture when compared with other facial bones. Athletic injuries, interpersonal altercations, falls, and motor vehicle accidents (MVAs) account for the greatest proportion of causes. In the children and adolescents, sports and falls are the major causes of isolated nasal bone fractures.2–4,7,8 For example, a study of sports-related fractures in U.S. high schools has found a 10.1% rate of fractures with the highest rate in football, basketball, and soccer.4 The investigators found that when facial fractures occurred, nasal fractures were the most common injury and resulted in more than 3 weeks of time lost or medical disqualification from participation in sports, in addition to incurring substantial costs to the patient’s family and health care system.
Regional differences in the presentation of nasal fractures can be observed. In a retrospective study of Brazilian children aged 5 to 17 years, Cavalcanti and Melo have found that facial injuries were 3-fold more frequent in males aged 13 to 17 years; the most common causes of these injuries were falls and MVAs.3 Among facial injuries in that study, nasal fractures were also most common, 51.3%, followed by the zygomatic-orbital complex, 25.4%. In another retrospective study, Hwang et al have reviewed and analyzed the medical records of 236 patients with facial bone fractures caused by athletic activity who were treated at one institution between 1996 and 2007.9 The investigators noted that the age group with the highest frequency of these injuries was 11 to 20 years (40.3%), with a significant male predominance across all age groups (13.75 : 1). There were 128 isolated nasal fractures, with soccer accounting for 39%, followed by other sports, including martial arts.
Anatomy
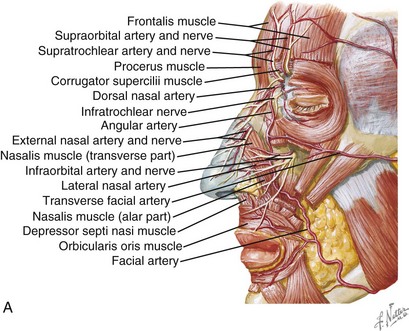
The nasal bones are paired and joined at the midline; they articulate with the frontal bone superiorly and the frontal process of the maxillary bones laterally. Caudally, they interact with the upper quadrilateral cartilages. Basally, they articulate with the nasal septum, which is formed by the perpendicular process of the ethmoid and the vomer inferiorly (Fig. 20-1).
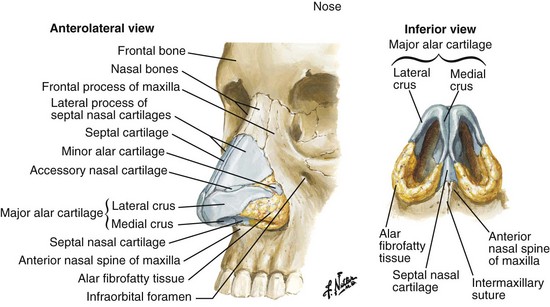
FIGURE 20-1 Bone and cartilage structures of the nose. (Netter illustration from www.netterimages.com, © Elsevier Inc., All rights reserved.)
Nasal air passage may be affected by a variety of conditions. Anatomically the internal and external nasal valves must be patent, with the former having an angle of at least 10 to 15 degrees. A deviated nasal septum, nasal spurs, concha bullosa, nasal polyps, and inflammatory sinonasal disease represent examples of altered anatomy that potentially become sources of nasal obstruction and may contribute to nasal airflow obstruction (Fig. 20-2).
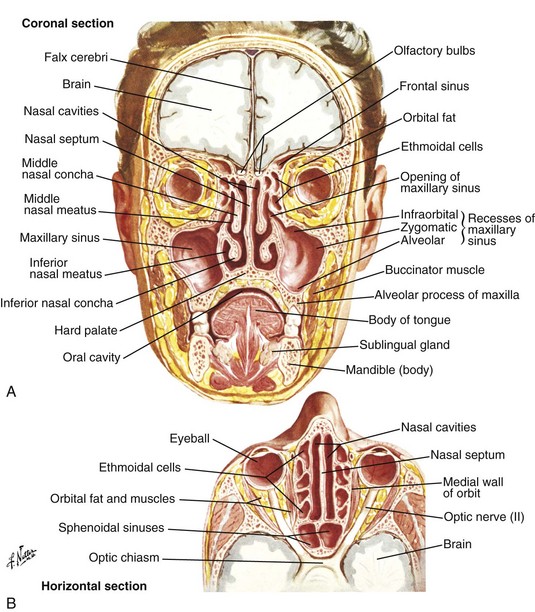
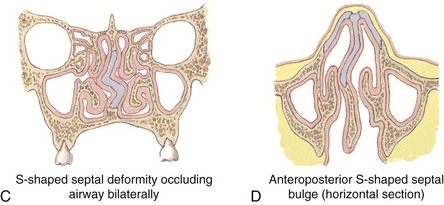
FIGURE 20-2 Internal structures of the nose. A, B, coronal and axial sections of the nasal region. C, D, Coronal and axial sections of the deviated septum that is S-shaped and obstructing both nasal cavities. (Netter illustrations from www.netterimages.com, © Elsevier Inc., All rights reserved.)
The neurosensory innervations of the nose are rich and complex (Fig. 20-3). The overlying nasal skin receives its innervation from the dorsal nasal and external nasal nerves, branches of the anterior ethmoidal and ophthalmic (to infratrocheal) nerves, respectively. Intranasally, the septum and lateral walls are innervated by branches of the sphenopalatine and anterior and posterior ethmoidal nerves. The nasal floor receives some fibers from the nasopalatine nerve and from the greater palatine nerve. The parasympathetic supply originates from the superior salivatory nucleus in the medulla, travels with the nervus intermedius and cranial nerve VII to the geniculate ganglion, and continues along the greater petrosal nerve and through the vidian canal to reach the pterygopalatine ganglion. The postganglionic fibers travel to the sinonasal mucosal, including the septum and turbinates.
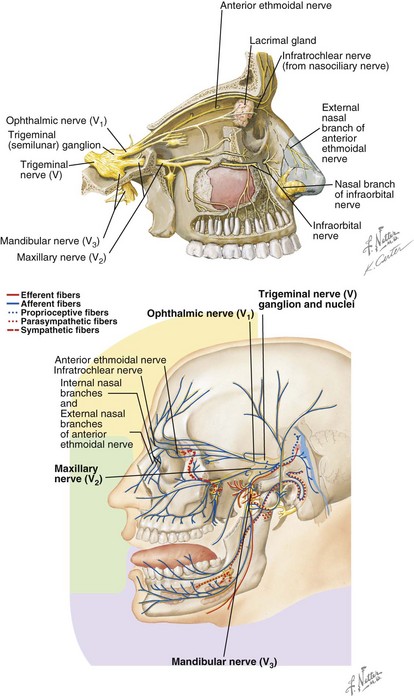
FIGURE 20-3 Neuroanatomy of the nasal complex. (Netter illustrations from www.netterimages.com, © Elsevier Inc., All rights reserved.)
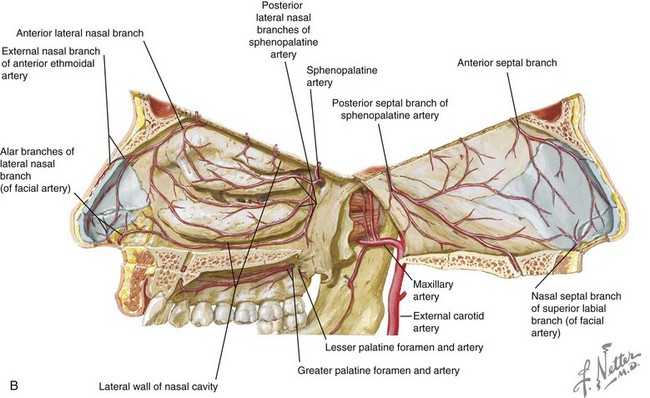
Although concerns exist among clinicians about nasal tip edema or vascular insufficiency resulting from operative management of nasal injuries and the use of vasoconstrictors, this has not been substantiated by research studies. Lymphoscintigraphy, along with cadaver dissections and histologic studies, have revealed that the primary blood supply for the nasal tip arises from the lateral nasal branches of the facial artery (Fig. 20-4). Other arteries supplying the nasal tip include the columellar branch of the superior labial artery and the external nasal branch of the anterior ethmoid artery. Moreover, it was found that the major arterial, venous, and lymphatic vessels course at or superficial to the musculoaponeurotic layer of the nose. Therefore, open approaches must limit dissection deep to this musculoaponeurotic layer to maintain nasal tip blood supply and drainage conduits.10
Evaluation of Injury to the Nose
Nasal Patency and Airflow Dynamics
The internal nasal valve primarily determines nasal resistance to airflow because this is typically the narrowest zone.11–14 This valve is triangular in shape and is formed by the junction of the caudal upper lateral cartilages and nasal septum.15–23 Inferiorly, it is bound by the nasal floor and posteriorly by the inferior turbinates. It has a cross-sectional area of approximately 55 mm2, with an angle of 10 to 15 degrees in whites. Fixed and dynamic causes of valve obstruction may be responsible. For instance, dynamic obstruction on inspiration may be seen with post-traumatic weakness of the upper or lower lateral cartilage. The Cottle test, in which the cheek is pulled laterally, may improve nasal airflow by pulling the upper lateral cartilage laterally and opening the internal valve area.24 Imaging modalities such as computer tomography (CT) may demonstrate the presence of contributing factors such as sinonasal disease, concha bullosa, and a posterior septal spur or septal deviation.
Radiographic Examination
A variety of options are available for imaging and categorizing nasal fractures and the surrounding region.25–30 Many isolated nasal injuries with no loss of consciousness and a clear history of the mechanism can be diagnosed and treated without the need for exposing the patient to radiation. Plain radiographic films may be adequate to assess the extent and displacement of nasal bone fractures when no other injuries are suspected, but they are used less often with the advent of CT.
Treatment of Nasal Injuries
For most routine nasal fractures, operative management of nasal fractures requires consideration for the timing, anesthetic, setting in which treatment is rendered, and details of the operative approach.31–33 The recommended time frame to repair nasal fractures is within the first week after injury. It is acceptable to perform immediate treatment, but at times it may be helpful to allow swelling to decrease prior to definitive treatment. Some recommend delaying surgery because it is may sometimes be difficult to judge the adequacy of reduction in the presence of significant edema. However, surgeons must remember that the elastic cartilaginous framework may be difficult to reduce as fibrin organization and fibrosis ensues; thus, delayed repairs beyond 1 week may become increasingly more difficult to treat with closed reduction alone. Children have a tendency to heal the bony tissue more quickly, which may make it more difficult to achieve a detailed repositioning. Treatment within the first several days facilitates the healing process, limits patient disability, and decreases the patient’s time spent away from school, work, or other activities.34
Cook et al compared the manipulation and reduction of nasal fractures under local anesthesia (LA) and general anesthesia (GA). In this study, LA was administered with 0.5% bupivacaine blocking the infraorbital, infratrochlear, and external nasal nerves.35 Patients in the LA group rated how painful the combined anesthesia administration and fracture manipulation had been on a scale from 1 to 5 at the 4-hour and 8-week time point after reduction. They also rated nasal airway patency and the surgeon rated the cosmetic result. After manipulation, the patency of nasal airways was comparable between the LA and GA groups. The local anesthesia group rated their median pain score as 3 out of 5. Pain was attributable to the infiltration of LA solution. When asked about their choice of anesthesia in case they would require nasal manipulation in the future, 24 of 25 patient in the LA group and 16 of 25 in the GA group indicated that they would opt for LA. There were no reported cases of perioperative airway compromise documented in these patients.
The same investigators also randomized two LA techniques among 50 consecutive adult patients with clinically displaced nasal fractures.36 One group received blocks of the infraorbital, infratrochlear, and external nasal nerves by intranasal infiltration and the other group was given generalized infiltration of the nasal dorsum by an external route. All patients received intranasal cocaine. Postoperatively, patients recorded their overall discomfort level and subjective nasal airway patency. The surgeon also recorded the cosmetic result. They found the internal route to be significantly more painful (p < .001) and with no advantage to the patient with respect to postoperative ai/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses