Dental Caries
Ann Wenzel
Disease Mechanism
Caries is a multifactorial disease with interaction among three factors: (1) the tooth, (2) the microflora, and (3) the diet. If not disturbed, bacteria accumulate at specific tooth sites to form what is known as bacterial plaque or biofilm. The development of caries requires both the presence of bacteria and a diet containing fermentable carbohydrates. Caries is an infectious disease; because it is the lactic acid produced by bacteria from the fermentation of carbohydrates that causes the dissolution, or demineralization, of the dental hard tissues. The Streptococcus mutans group plays a central role in demineralization. In the initial stages of the disease, bacteria are located on the tooth surface. It is only after severe demineralization or cavity formation has occurred that bacteria penetrate into the hard tissues. The demineralized area in the tooth surface, called the carious lesion, is not the disease but a reflection of continuing or past microbial activity in the biofilm.
The initial carious lesion is a subsurface loss of mineral in the outer tooth surface. It appears clinically as a chalky white spot (indicating present activity) or an opaque or dark, brownish spot (indicating past activity). A lesion beneath active bacterial plaque will progress, slowly or quickly, but if the biofilm is removed or disturbed, the lesion will arrest. However, an arrested lesion may become reactive and progress any time there is activity in the biofilm. Alternatively, remineralization in the outermost parts of an arrested lesion can occur, such as after the use of fluorides. Caries is an ever-dynamic process.
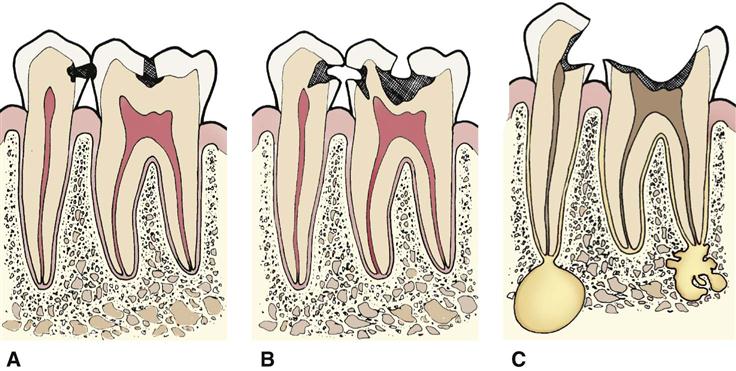
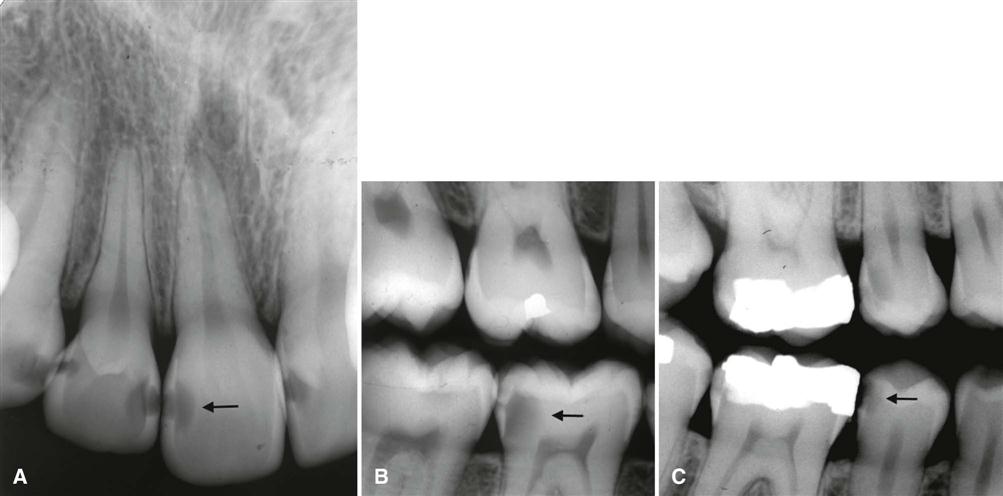
The rate and extent of mineral loss depend on many factors. Mineral loss occurs faster in an active lesion when intercrystalline voids form. Demineralization may extend well into dentin before a breakdown of the outer surface (cavitation) occurs, resulting in a clinically visible cavity. With lesion progression and no intervention, demineralization may progress through the enamel and the dentin and eventually into the pulp and may destroy the tooth (Fig. 18-1).
Role of Radiography in Detection of Carious Lesions
Radiography is useful for detecting carious lesions because the caries process causes demineralization of enamel and dentin. The lesion is seen in a diagnostic image as a radiolucent (darker) zone because the demineralized area of the tooth does not absorb as many x-ray photons as the unaffected portion.
Radiography is a valuable supplement to a thorough clinical examination of the teeth for detecting caries lesions. A careful clinical examination assessing the carious activity on the tooth surface may be possible for smooth surfaces and to some extent for occlusal surfaces. However, when the surface is clinically intact (i.e., no breakdown leading to cavitation has occurred), even the most meticulous examination may fail to reveal demineralizations beneath the surface, including occlusal surfaces. Clinical access to proximal tooth surfaces in contact is limited. Numerous clinical studies have shown that a radiologic examination can reveal carious lesions that would otherwise remain undetected both in occlusal and in proximal surfaces.
The lesion detected in the diagnostic image is merely a result of the bacterial activity, past or present, on the tooth surface, and radiography cannot reveal whether the lesion is arrested or active. An old inactive lesion would still appear as a demineralized “scar” in the hard tissues (Fig. 18-2). The reason is that remineralization takes place only in its outermost surface because mineral-containing solutions from saliva cannot diffuse into the body of the lesion. Because the image mirrors only the current extent of demineralization, one radiograph alone cannot distinguish between an active and an arrested lesion. Only a second image taken at a later time can reveal whether the disease was active.
There has been a dramatic decline in the prevalence of caries in Western countries in recent decades, leaving a smaller fraction of the population with rapidly progressing carious lesions. Therefore, the interval between examinations should be customized for each patient on the basis of the perceived caries activity and susceptibility. For caries-free individuals, the interval may be lengthened, whereas the interval should be shorter for individuals with active caries. When a decision is made to monitor a lesion, factors such as oral hygiene, fluoride exposure, saliva flow, diet, caries history, extent of restorative care, and age should be considered in determining the time interval between radiologic examinations (see Chapter 16).
Examination with Conventional Intraoral Film
The bitewing projection is the most useful image for detecting carious lesions (see Chapter 7). The use of a film holder with a beam-aiming device reduces the number of overlapping contact points and improves image quality, minimizing interpretation errors. Periapical images are useful primarily for detecting changes in the periapical bone. Use of a paralleling technique for obtaining periapical images increases the value of this projection in detecting carious lesions of both anterior and posterior teeth, especially with heavily restored teeth.
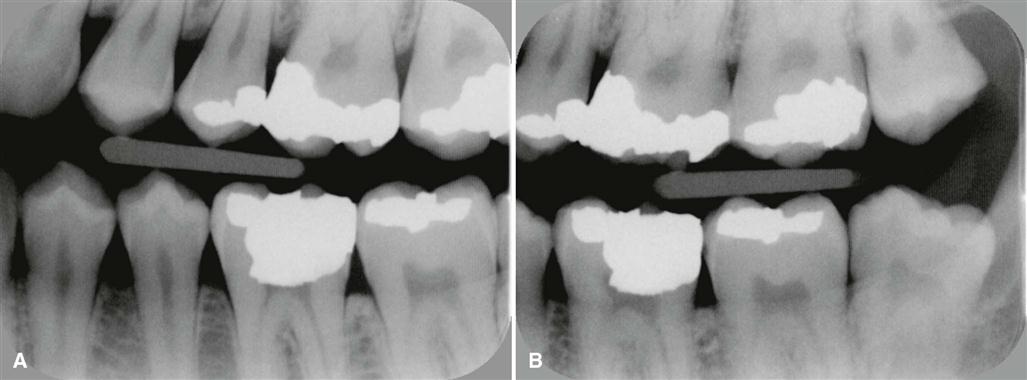
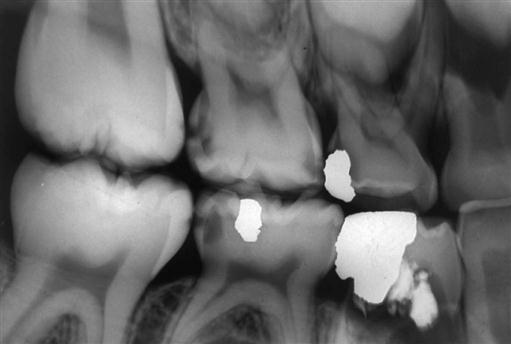
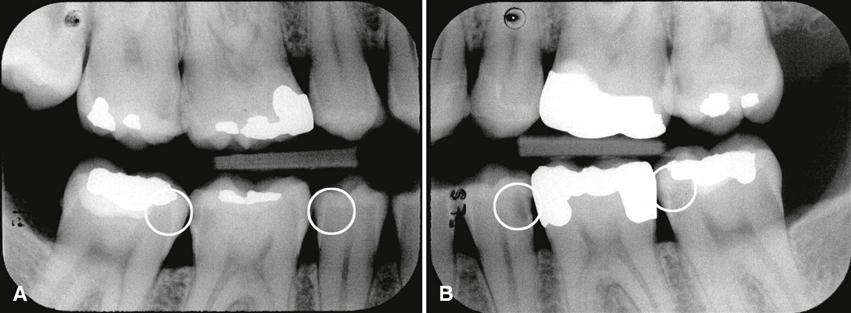
Traditionally, No. 2 “adult” films are used for a bitewing examination from the age of approximately 7 to 8 years onward. When it is necessary to examine all the contact surfaces from the cuspid to the most distal molar, one or two bitewing images per side are required, depending on the number of teeth that are present (Fig. 18-3). The use of a single No. 3 film often results in overlapping contact points and “cone-cut” images and is not recommended. In small children, No. 0 or “child” film may be used instead of No. 2 film (Fig. 18-4).
Conventional radiographs used to detect carious lesions should be mounted in frames with dark borders and interpreted with use of a light box with sufficient luminance and a magnifying viewer. Figure 18-5 shows a series of radiographs showing early lesions with and without magnification.
Examination with Digital Intraoral Receptors
Digital image receptors may replace film for intraoral radiography. Two different methods are available: (1) solid-state sensors (charge-coupled device (CCD) and complementary metal oxide semiconductor technology (CMOS)) with a cord that connects the receptor to the computer or without a cord (signal is transferred by radio wave) and (2) storage phosphors (photostimulable phosphor plates (PSP) that use a filmlike plate that is processed (scanned) after exposure (see Chapter 4). The holders available for bitewing examinations with phosphor plates appear similar to those for film; universal sensor holders are also available. However, there may be some problems when solid-state sensors are used for bitewing examinations. First, the surface area of the sensor is smaller than the surface area of a No. 2 film, resulting in the display of fewer interproximal tooth surfaces per bitewing image than with film. Second, the stiffness and increased thickness of these sensors create more discomfort for the patient and may result in more projection errors and retakes. When digital bitewing images are used, they should be displayed on a quality monitor in their full resolution for interpretation and viewed in a room with subdued light.
Detection of Carious Lesions
Proximal Surfaces
Typical Appearance
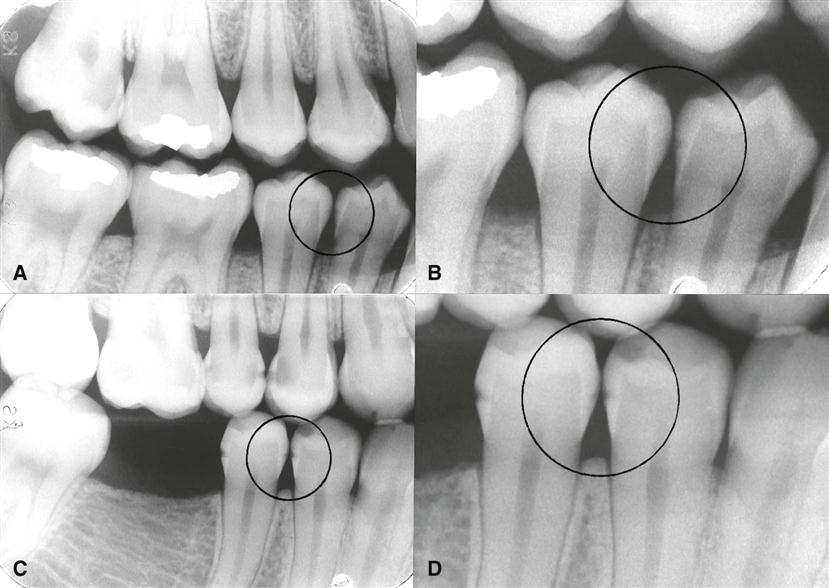
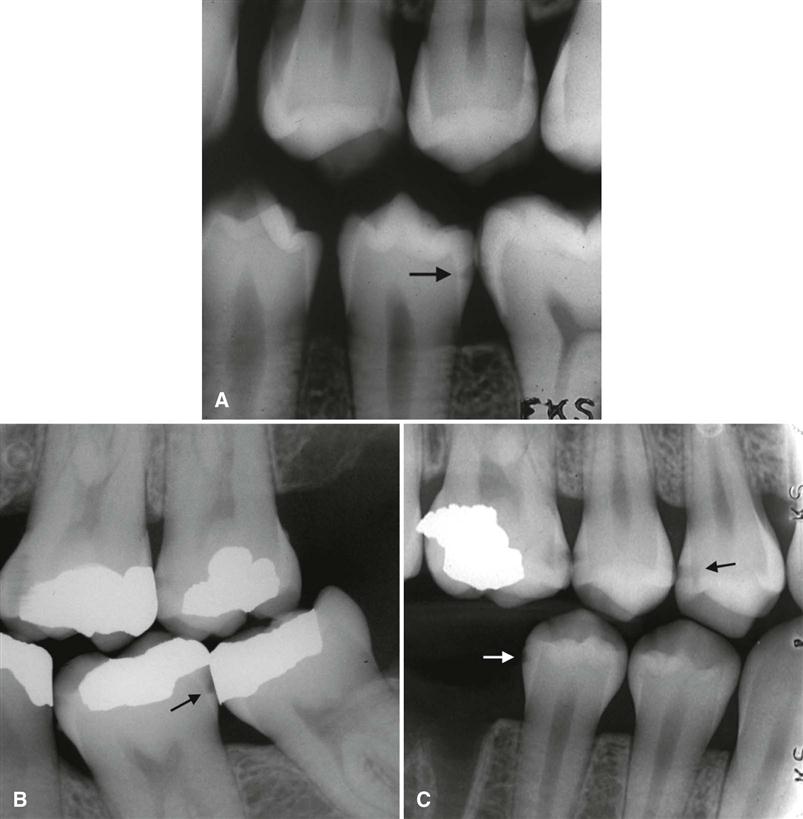
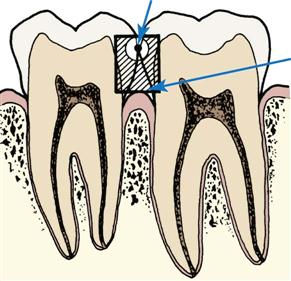
The shape of the early radiolucent lesion in the enamel is classically a triangle with its broad base at the tooth surface (see Fig. 18-5) spreading along the enamel rods, but other appearances are common, such as a “notch,” a dot, a band, or one or more thin lines (Fig. 18-6). When the demineralizing front reaches the dentinoenamel junction (DEJ), it spreads along the junction, frequently forming the base of a second triangle with apex directed toward the pulp chamber (Fig. 18-7). This triangle typically has a wider base than in the enamel and progresses toward the pulp along the direction of the dentinal tubules. More irregular shapes of demineralization may be seen.
Lesions involving proximal surfaces are most commonly found in the area between the contact point and the free gingival margin (Fig. 18-8). The fact that this type of lesion does not start below the gingival margin helps distinguish a carious lesion from cervical burnout. Close attention should be paid to intact proximal surfaces adjacent to a tooth surface with a restoration because occasionally this surface is inadvertently damaged during the restorative procedure and is at greater risk for caries (Fig. 18-9).
Because the proximal surfaces of posterior teeth are often broad, the loss of small amounts of mineral from incipient lesions and the advancing front of active lesions are often difficult to detect in the image. Lesions confined to enamel may not be evident until approximately 30% to 40% demineralization has occurred. For this reason, the actual depth of penetration of a carious lesion is often deeper than seen in the image.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses