Principles of Radiographic Interpretation
Mariam Baghdady
Dentists are expected to have basic skills in interpreting any intraoral or extraoral images that might be used in dental practice. This ability requires the mastery of two identifiable and nonseparable components of visual diagnosis: perception, the ability to recognize abnormal patterns in the image, and cognition, the interpretation of these abnormal patterns to arrive at a diagnosis. This chapter provides an overview of diagnostic reasoning in oral radiology. It also provides an analytic framework to aid in the interpretation of diagnostic images. This framework will equip the reader with a systematic method of image analysis.
Adequate Diagnostic Images
Any method of image analysis is limited by the information contained in the available diagnostic images. Ensuring that there are an adequate number of images of diagnostic quality that display the region of interest in its entirety is an essential first step. When using plain or projection images, multiple images at slightly different projection angles and images exposed at right angles to one another often provide significant additional information. When appropriate, the use of advanced forms of diagnostic imaging can also provide valuable diagnostic information (see Chapter 16).
Visual Search Strategies
The ability to find and identify abnormal patterns in the diagnostic image first involves a visual search of the entire image. An ability to recognize an abnormal pattern requires an in-depth knowledge of the variations of appearances of normal anatomy. This is especially true in searching panoramic images. It is likely that experienced radiologists use a free search pattern when analyzing a diagnostic image. However, more recent research has shown that the employment of a systematic search strategy by novice clinicians improves their ability to detect abnormalities in panoramic images. A systematic search strategy involves the identification of a list of normal anatomic structures that would be contained within the image. In a panoramic image, this strategy might involve identifying the posterior border of the maxilla, the floor of the sinus, the zygomatic process of the maxilla, and the orbital rim. In a periapical image, the list might include crown, root structure, pulp and pulp canal, periodontal membrane space, and lamina dura. In a data set of cone-beam computed tomographic (CBCT) images, the normal anatomy would be inspected through the whole image volume using axial, coronal, and sagittal image slices. When faced with a complex appearance of anatomic structures, having a systematic search strategy enables the novice clinician to search the complete image in a meaningful and more successful fashion. When an abnormality has been detected in an image, the clinician must focus on formulating an interpretation of the abnormality.
Diagnostic Reasoning in Oral Radiology
Clinical reasoning in diagnostic oral radiology can be considered unique in that the initial task requires the clinician to engage in a complex perceptual phase that involves differentiating normal and abnormal anatomic structures on two-dimensional images that represent three-dimensional structures. After the search process, if a finding is deemed abnormal, the clinician forms a mental three-dimensional image of the abnormality that includes the precise location, size, internal structure, and how the abnormality affects the surrounding normal structures. This complex perceptual step is a method of identifying features of the abnormality used to arrive at a plausible diagnosis.
A common method for a novice clinician is to memorize specific features of each type of abnormality and then attempt to use this information to interpret images. This approach has been shown to be ineffective in correct interpretation of radiographic abnormalities. However, it has been found that understanding the basic disease mechanism underlying the changes that each type of abnormality can render in the diagnostic image is more effective in enhancing a clinician’s diagnostic accuracy. The terms “disease mechanism” and “basic science” are used to represent the pathophysiologic basis of abnormalities at the cellular, tissue, and biochemical levels. More recent research suggests that the understanding of disease mechanisms plays an essential role in enhancing diagnostic accuracy in novice clinicians. Basic science knowledge apparently creates a coherent mental representation of diagnostic categories and their features. According to this theory, basic sciences may assist in “true understanding” of the diagnostic entities by creating coherent mental representations of different disease categories. Hence, when clinicians understand why certain features occur, they are able to make the diagnosis that “makes sense,” rather than simply focusing on feature counting and rote memory. Also, more recent research shows that teaching disease mechanisms and radiographic features in an integrated fashion produced novice clinicians with higher diagnostic accuracy than novice clinicians who were taught in a segregated manner.
Worth, a pioneer in diagnostic oral radiology, stated, “Radiographic appearances are governed by anatomic and physiologic changes in the presence of disease processes. Radiologic diagnosis is founded on knowledge of these alterations, the prerequisite being awareness of disease mechanisms.”
Analysis of Abnormal Findings
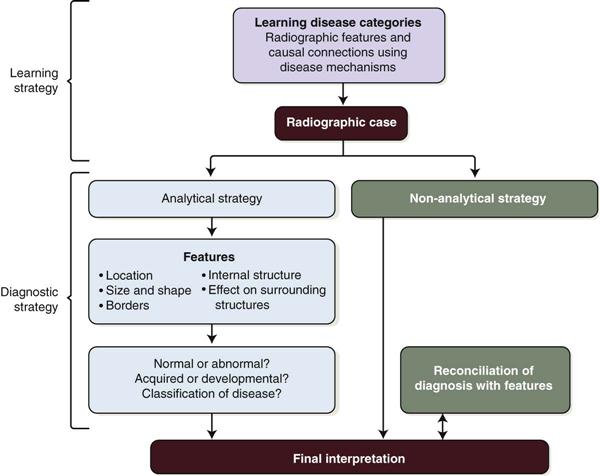
There are two main forms of diagnostic processing described in radiology; the first is the analytic or systematic strategy. This approach relies on a step-by-step analysis of all the imaging features of an abnormal finding so that a diagnosis can be made based on these findings (Fig. 17-1). This analytic process is believed to reduce bias and premature closure of the decision-making process.
The second form, a nonanalytic strategy, assumes that simply viewing an abnormal finding automatically leads to a holistic diagnostic hypothesis, which is followed by a deliberate search for features that support the initial hypothesis. The nonanalytic approach suggests that the clinician makes an automatic decision regarding the diagnosis without thorough feature analysis of the image. For example, expert radiologists may rely on pattern recognition as a nonanalytic diagnostic strategy.
There is some empirical evidence that nonanalytic reasoning can be successfully employed by novice clinicians. However, critics of teaching novices to rely on nonanalytic processing argue that the success of this diagnostic strategy is limited by the novice’s minimal experience and the varied appearances of both normal anatomy and pathologic disorders in images.
Although these two processes are viewed as separate mechanisms, research provides evidence that they are complementary and should not be viewed as being mutually exclusive. Students learning oral radiology could potentially benefit from specific training in the use of combined analytic and nonanalytic diagnostic strategies.
An analytic tool for the analysis of abnormal findings is presented in the next section. The main function of this tool is to collect all the available imaging characteristics of the abnormal finding. Once the information is assembled, it is useful in the diagnostic process.
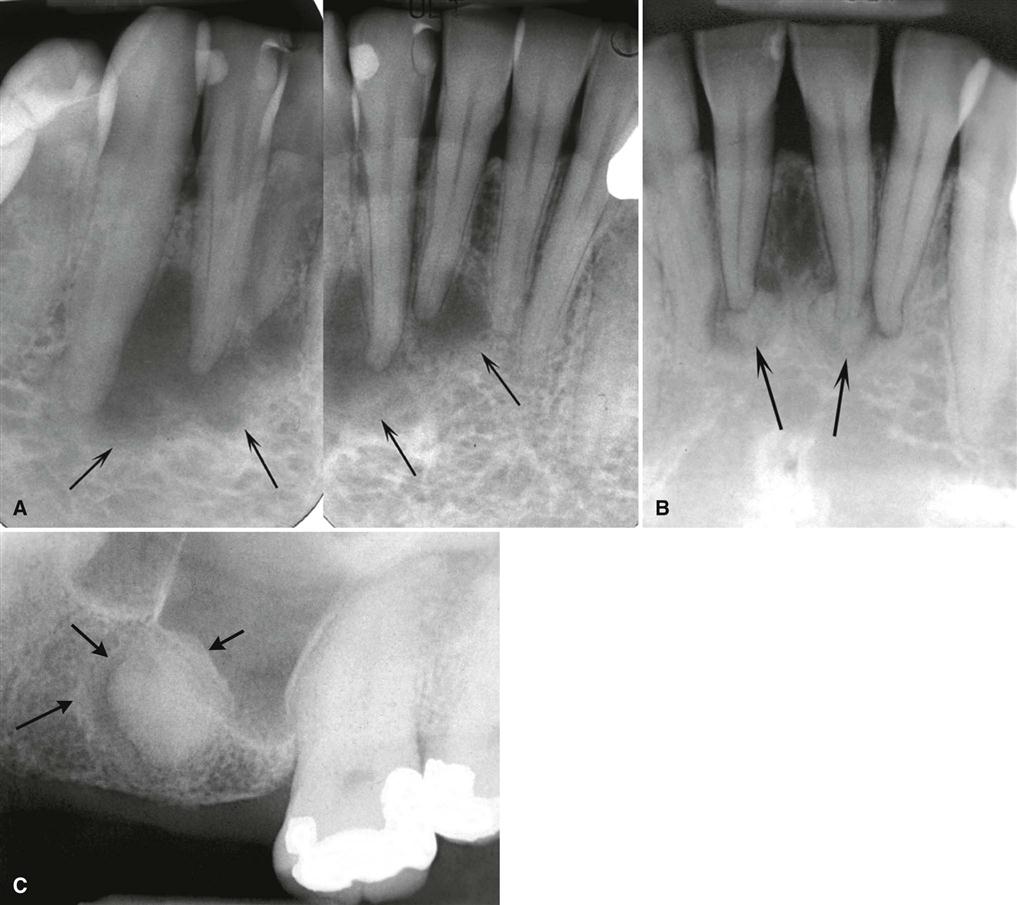
As the imaging characteristics are being collected, it is important to integrate the disease mechanism underlying these characteristics when possible. For instance, Figure 17-2 depicts the maturation of periapical osseous dysplasia (periapical cemental dysplasia). At the first stage (Fig. 17-2, A), the periapical bone is resorbed and replaced with fibrous tissue, and therefore it appears radiolucent in the image. In a later maturation stage, this abnormality produces amorphous bone in the center (Fig. 17-2, B), resulting in a radiopaque mass in the center surrounded by a soft tissue radiolucent rim. Knowledge of the disease mechanism allows for the correct diagnosis of a lesion of periapical osseous dysplasia in an unusual location in the maxilla and after the associated tooth has been extracted (Fig. 17-2, C).
Analytic or Systematic Strategy
Step 1: Localize Abnormality
Localized or Generalized
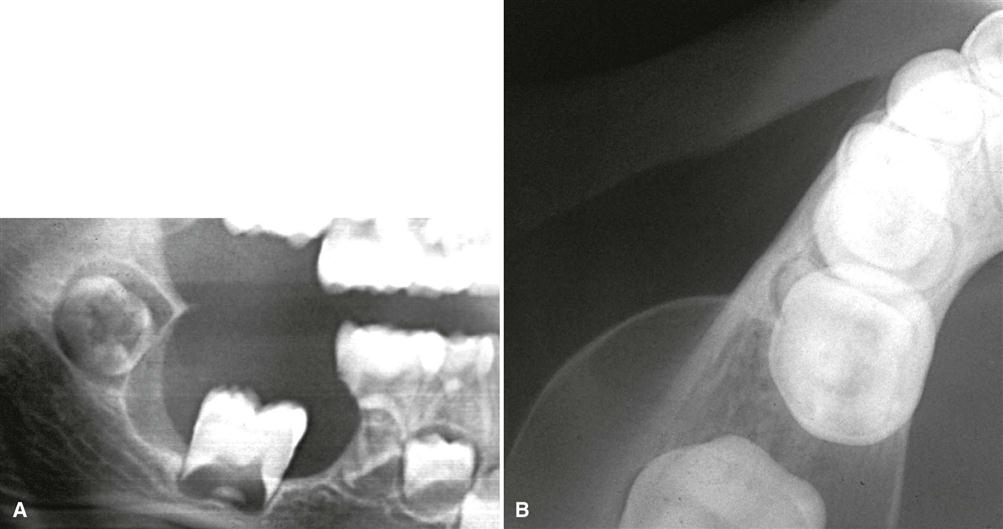
The anatomic location and limits of the abnormality should be described. This information aids in starting to select various disease categories. If an abnormal appearance affects all the osseous structures of the maxillofacial region, generalized disease mechanisms, such as metabolic or endocrine abnormalities of bone, are considered. If the abnormality is localized, one considers whether it is unilateral or bilateral. Variations of normal anatomy are more commonly bilateral. For instance, a bilateral mandibular radiolucency may indicate normal anatomy, such as extensive submandibular gland fossa. Abnormal conditions are more commonly unilateral. For instance, fibrous dysplasia commonly is unilateral. This is not to say that localized pathologic lesions cannot occur bilaterally in the maxillofacial region. A few abnormalities, such as Paget’s disease and cherubism, are always seen bilaterally in the jaws. Also, when cherubism involves the mandible, the first region to be involved is in the midramus region, and this is the mechanism behind the anterior displacement of molars (Fig. 17-3).
Position in the Jaws
Identifying the exact location of the lesion in the maxillofacial complex aids the diagnostic process in two ways: (1) it determines the epicenter and (2) some lesions tend to be found in specific locations.
Determining the epicenter of the lesion or the point of origin assists in indicating the tissue types that compose the abnormality in question. The epicenter can be estimated on the basis of the assumption that the abnormality grew equally in every direction. This estimation may become less accurate with very large lesions or lesions with ill-defined boundaries. Following are a few examples of relating the epicenter of the lesion to the tissue of origin:
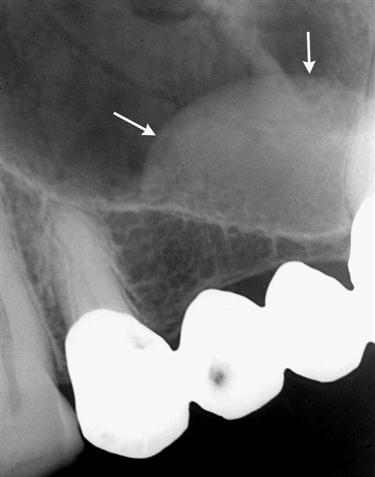
• If the epicenter is coronal to a tooth, the lesion probably is composed of odontogenic epithelium (Fig. 17-4).
• If it is above the inferior alveolar nerve canal (IAC), the likelihood is greater that it is composed of odontogenic tissue (Fig. 17-5).
• If the epicenter is below the IAC, it is unlikely to be odontogenic in origin (Fig. 17-6).
• If it originates within the IAC, the tissue of origin probably is neural or vascular in nature (Fig. 17-7).
• If the epicenter is within the maxillary antrum, the lesion is not of odontogenic tissue, as opposed to a lesion that has grown into the antrum from the alveolar process of the maxilla (Fig. 17-8).
The other reason to establish the exact location of the lesion is that particular abnormalities tend to be found in very specific locations. Following are a few examples of this observation:
Single or Multifocal
Establishing whether an abnormality is solitary or multifocal aids in understanding the disease mechanism of the abnormality. Additionally, the list of possible multifocal abnormalities in the jaws is relatively short. Examples of lesions that can be multifocal in the jaws are periapical cemental dysplasia, keratocystic odontogenic tumors, metastatic lesions, multiple myeloma (Fig. 17-9), and leukemic infiltrates. Exceptions to all these points may occur occasionally. However, these criteria may serve as a guide to an accurate interpretation.
Size
Finally, the size of the lesion is considered. There are very few size restrictions for a particular lesion, but the size may aid in the differential diagnosis. For instance, when differentiating between a dentigerous cyst and a hyperplas/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses