Diagnosis and Treatment of Midface Fractures
The midfacial complex is constructed of a series of vertical pillars that primarily provide protection from vertically directed forces. These include the nasomaxillary (nasofrontal), zygomaticomaxillary, and pterygomaxillary buttress.1 These vertical pillars are further supported by the horizontal buttresses—the supraorbital or frontal bar, infraorbital rims, and zygomatic arches.2,3 Contrary to claims of a lack of sagittal buttresses, the midface does have support, however weak, from the maxillary walls, lateral nasal wall, and nasal septum. Clearly, these weaker buttresses of the midface tolerate frontal or laterally directed forces poorly.4 Behind this buttress system sits the medial and lateral pterygoid plates inferiorly and the skull base superiorly. This framework results in a few anatomic sites of weakness, resulting in fairly predictable patterns of fracture.
Le Fort Classifications
Rene Le Fort’s cadaver studies in the early twentieth century defined the three weakest levels of the midfacial complex when assaulted from a frontal direction. He defined the three most common “linea minoros resistentiae,” which are classified as the Le Fort I, Le Fort II, and Le Fort III fractures. These fracture patterns are characteristic of a unidirectional, low-energy injury rather than the multivector, high-energy mechanisms commonly observed today. However, this system is popular because it provides a simple, anatomically differentiated system for the general classification of midfacial injuries.5
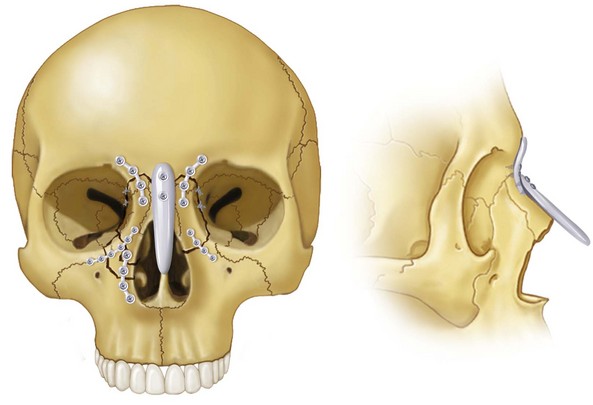
The Le Fort type I fracture pattern results from a force directed above the maxillary teeth, resulting in a floating palate (Fig. 17-1). The Le Fort type II fracture pattern results from a force delivered at the level of the nasal bone, resulting in mobility of the midface through the orbits and midfacial region (Fig. 17-2). The Le Fort type III fracture pattern results from a force directed at the orbital level, resulting in a craniofacial dysjunction or separation of the entire middle third of the craniomaxillofacial skeleton from the skull base (Fig. 17-3).
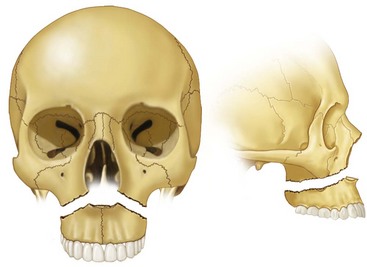
FIGURE 17-1 Le Fort I fracture.
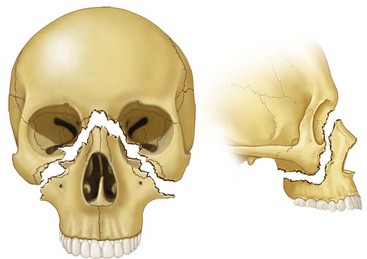
FIGURE 17-2 Le Fort II fracture.
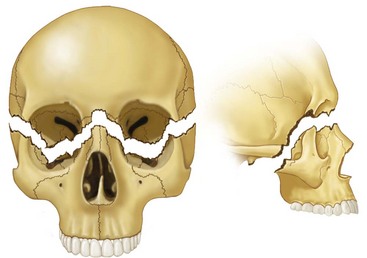
FIGURE 17-3 Le Fort III fracture.
Emergency Care
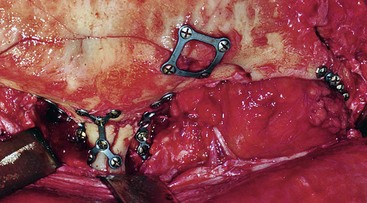
Initial evaluation of the severely injured midface can be an intimidating experience (Fig. 17-4). Emergency care should be immediately initiated, applying the principles of Advanced Trauma Life Support (ATLS). When dealing with midfacial injuries in the emergency setting, certain components of the examination and treatment deserve special attention (Fig. 17-5).
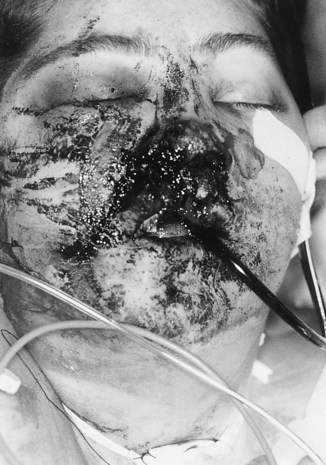
FIGURE 17-4 Compound comminuted midfacial fractures.
The airway is immediately evaluated for obstruction. The oral cavity may be full of secretions or debris, which may contribute to supraglottic obstruction and aspiration. The oropharynx must be manually cleared of any fractured teeth, dentures, and/or blood clots. If stable, the patient may be placed in a lateral decubitus position and mild Trendelenburg position to allow optimal drainage. If oral or nasal bleeding is encountered, these sites should be packed.6 If bleeding is uncontrollable, a definitive airway should be established immediately.
Any patient with facial trauma is presumed to have a cervical spine injury and should be stabilized with a rigid collar until ruled out by appropriate examination. Any motion of the head can be lethal because of bone fragment impingement or laceration of the spinal cord. The presence of cervical spine injuries have been reported as 1.0% to 1.8% to as many as 9.6% of patients with facial fractures.7–9
The safety of orotracheal intubation by various techniques in patients with cervical spine injuries has been shown to be safe if precise in-line immobilization is provided.10 A cricothyroidotomy is also an appropriate option for establishing an emergency definitive airway in this setting.11 If nonurgent airway control is needed in the setting of cervical spine fracture, an awake fiberoptic intubation is likely the safest option because no atlanto-occipital extension is required with this technique.12
Facial Examination
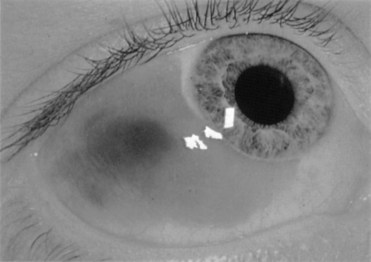
Periorbital edema and ecchymosis are often initial signs of orbital trauma (Fig. 17-6). The globe may protrude because of gross edema, making a complete examination difficult. Visual acuity is grossly examined and extraocular muscle function evaluated. The presence and direction of diplopia or strabismus are noted. Pupil size, shape, and reaction to light are recorded. The location and extent of subconjunctival hemorrhage are also recorded. A fundoscopic examination is carried out to evaluate for intraocular hemorrhage. If lid lacerations are present, they should be closed promptly to prevent contracture. A through and through laceration requires a three-layer closure. A 6-0 plain absorbing suture may be used on the conjunctiva, with care to prevent protruding knots that may injure the cornea. The orbicularis oculi muscle is closed with 5-0 resorbable suture; the skin is closed with a 6-0 nonresorbable suture. Exact approximation of the gray line of the lid margins is obtained with 6-0 resorbable suture (Fig. 17-7).
Ocular injury is present in most midfacial fractures and is common in midfacial trauma. Al-Qurainy et al, in a prospective study on orbital injury with midfacial fractures of any type, have reported that 90% of patients had an ocular injury to some degree, 16% had moderate ocular injuries, and 12% had severe injuries. Almost 15% of patients had a decrease in vision.13 In patients with naso-orbital-ethmoid fractures, ocular injury and subsequent loss of vision were reported in 30% of patients.14 Isolated orbital wall fractures have also been reported to present with an almost 30% incidence of ophthalmic complications.15 Current evidence supports the practice that facial fractures involving the orbit should be referred for ophthalmologic evaluation.13–18
Crepitation to palpation is indicative of orbital emphysema. This examination finding is most commonly observed when injuries result in communication with the ethmoidal or maxillary sinuses and requires no treatment. The patient should, however, be instructed to not blow his or her nose to prevent expanding subcutaneous emphysema. The attachment of the medial canthal ligament is evaluated by palpating the insertion of the medial canthal ligament for crepitus or instability and by lateral traction on the lateral canthus. Bimanual examination may also be performed by application of a Kelly clamp intranasally and a finger on the central fragment; this is followed by an attempt at lateral displacement of the central fragment.19 Physical findings of medial canthal ligament disruption include rounding of the lacrimal lake, epiphora, and increased intercanthal distance.
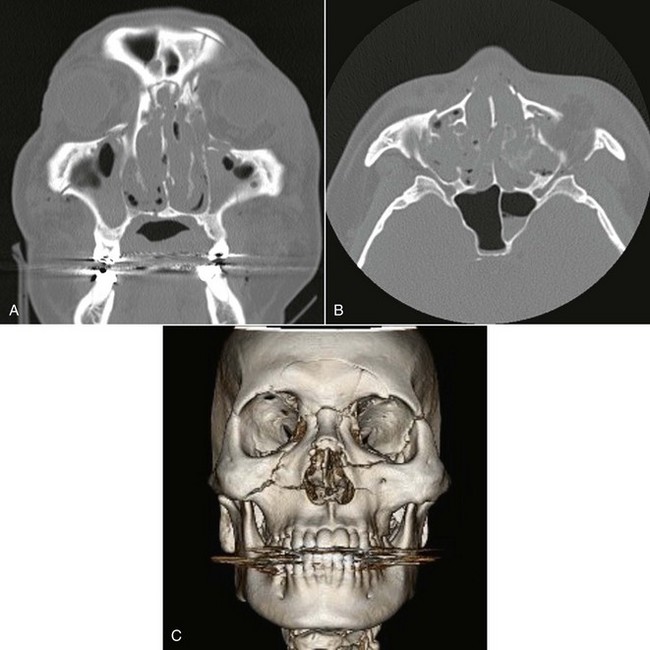
Once the patient is sufficiently stabilized, radiographic evaluation may proceed. The preferred radiologic modality for midfacial injuries is a maxillofacial computed tomography scan (CT).20–22 A maxillofacial CT scan will provide 2- to 3-mm axial cuts with coronal reformatting. If desired, sagittal or three-dimensional formatting may also be provided. The CT scan allows evaluation of bone, providing detailed information about fracture patterns. CT scans also provide characterization of soft tissues, including the extent of edema, presence of foreign bodies, formation of a retrobulbar hematoma, or entrapment of the extraocular musculature. Plain films, although necessary in the absence of CT scanning, provide little diagnostic information. The plain films obtained in the history include the Water’s, submentovertex, anteroposterior, and lateral skull views.
The maxilla, palatine bone, and nasal bones form the bulk of the midface. The maxillary bones are integral in the formation of the three major cavities of the face—the upper part of the oral cavity and the nasal and orbital fossa. The maxillary sinus, which is small at birth, expands inferiorly within the maxilla with maturity until it forms the major bulk of the midface. This factor adds to the distinct weakness of the region. Because of the many articulations between the surrounding bones, it is difficult at times to categorize fractures patterns. However, the classic Le Fort I and II classifications of midfacial fractures will be discussed here and the Le Fort type III and naso-orbital-ethmoid (NOE) fracture patterns will be discussed separately (Fig. 17-8).
Le Fort Type I Fractures
Treatment of Le Fort Type I Fractures
Incisions for the open reduction are made in the buccal vestibule in a circumvestibular fashion, from the first premolar to the first premolar on the opposite side. Wide buccal pedicles of the U-shaped incision are retained for maintenance of the vascular supply. This approach allows visualization of the lateral antral wall and zygomatic buttresses. A Rowe or Hayton-Williams forceps can then be used to complete the reduction, if necessary (Figs. 17-9 and 17-10).
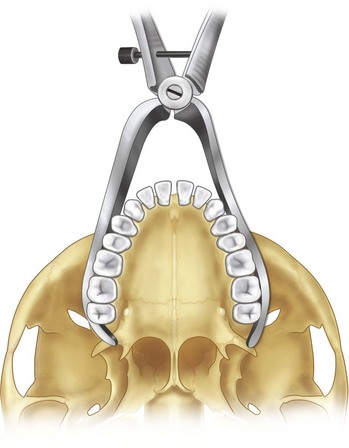
FIGURE 17-10 Positioning of the Hayton-Williams forceps when attempting to reduce a fractured maxilla.
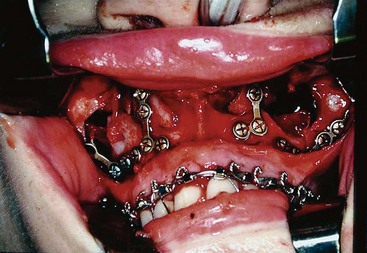
The patient is first placed in MMF to reestablish the pretraumatic occlusal relationship. The maxillomandibular complex can then be oriented in three dimensions as a unit, with special attention to the position of the condyles. Ensuring that the condyles are seated properly in the glenoid fossa will limit subsequent development of an open bite. Stabilization of a fracture must prevent translational and rotational motions in the x, y, and z axes.23 Four-point fixation along the pyriform and zygomaticomaxillary buttresses is routinely provided for stability of this fracture pattern. Occlusion should be immediately rechecked following release of MMF (Fig. 17-11).
Le Fort Type II (Pyramidal) Fractures
The Le Fort type II fracture pattern is also referred to as a pyramidal fracture; the apex of the pyramid is the nasofrontal suture (Fig. 17-12). This fracture pattern involves the nasofrontal suture, nasal and lacrimal bones, infraorbital rim in the region of the zygomaticomaxillary suture, maxilla, and pterygoid plates. This fracture is typically higher than the Le Fort type I fracture posteriorly. As with the Le Fort type I pattern, the nasal septum may also be involved.
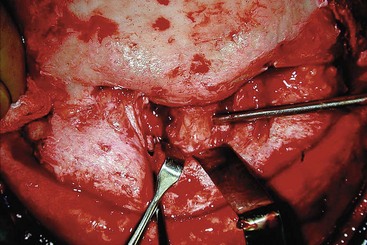
FIGURE 17-12 Le Fort II fracture.
Treatment
Infraorbital Incision
The infraorbital incision, first described by Converse et al in 1944,24,25 is made transcutaneously over the infraorbital rim in the natural crease, 4.5 mm inferior to the gray line. Advantages include excellent access to the floor and surrounding areas and ease of use. Disadvantages are potential poor healing, cicatricial distortion of the lower lid, and potential for development of lymphedema. More than 90% of the lymphatic drainage from the scalp, forehead, and upper lid passes lateral to the orbit.
Subciliary or Lower Blepharoplasty Incision
The subciliary or lower blepharoplasty incision is made 2 to 3 mm inferior to the gray line of the lower eyelid. The incision runs parallel to and along the length of the lower eyelid margin. The traditional method of pre–orbicularis oculi incision has fallen out of favor because of high rates of ectropion development, 38% to 42% temporary and 8% permanent.26 The post–orbicularis oculi dissection, or skin-muscle flap, is when the incision is made through both skin and muscle and dissection occurs superficial to septum. This modification has become popular because of ease of use and has been shown to have a lower rate of early ectropion, 6% in one study, with resolution typically within weeks.27
Transconjunctival Incision
The transconjunctival approach was popularized by Tessier in 1973.28 This approach is made through the conjunctiva parallel to the gray line and can be made anterior or posterior to the septum.29 The incision can also be extended laterally by lateral canthotomy and inferior cantholysis and medially by a transcaruncular incision to allow excellent access to the orbit (Fig. 17-13).
Palatal Fractures
Isolated fractures of the palate are rare, but up to 8% to 13% of Le Fort fractures are complicated by concomitant palatal fractures.30,31 Most patients will also have notable signs and symptoms of palatal fracture. Indications of palatal fracture on clinical examination include laceration of the lip and concurrent gingival and palatal lacerations. Often, a change in occlusion is also noted with the maxillary segment displaced anterolaterally.3 Diagnosis is confirmed by a maxillofacial CT with axial and coronal cuts.
Classification
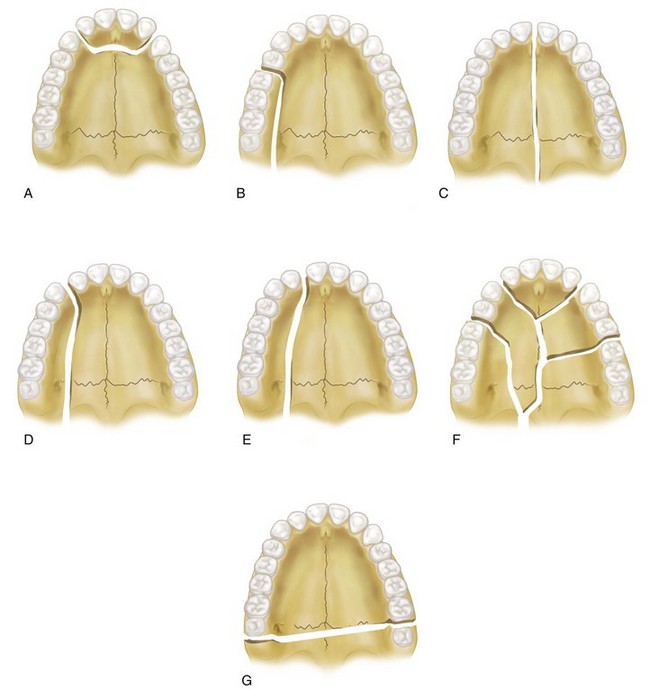
Several classification systems have been suggested30,31 for palatal fractures. Hendrickson et al30 have described six patterns based on the anatomic location of fracture (Fig. 17-14; Box 17-1).
Treatment
Surgical treatment planning depends on the type of fracture, presence or quality of the dentition, and concomitant facial fractures. Treatment incorporates the possible application of rigid internal fixation, arch bars, and palatal acrylic splints, depending on the clinical situation.3,30–33
Although there has been much discussion on the use of rigid fixation in palatal vault fractures, it is seldom clinically indicated. The first problem with this technique originates with the placement of transoral plates and screws to the palatal vault. This practice requires the mouth to be open and thereby excludes the application of ORIF and occlusal stabilization. This lack of occlusal control leads almost inescapably to error in the appropriate reduction of maxillary width and height. The second consideration is vascularization of the maxilla. Although techniques for making longitudinal palatal incisions are often described, vascular studies of the Le Fort I segment following osteotomy have shown that the blood flow in the severely fractured or osteotomized maxilla is dependent on the ascending pharyngeal and palatal mucosal blood supply.34 Because management of midfacial injury often require an anterior vestibular incision, if treated open, any palatal flap raised under these circumstances must be approached with caution.
An indication for the use of rigid fixation for sagittal palatal fractures in the edentulous or near-edentulous patient exists if the patient does not have preexisting dentures or no preoperative Gunning-type splint was fabricated. In these rare patients, special care must be taken to reduce the fractures as anatomically as possible from the facial vestibular approach. Additional stabilization of the palate can then be gained from transmucosal locking plate and screw fixation, as described by Pollock, which attempts to preserve the critical vascular supply.35
Naso-Orbital-Ethmoid Injuries
The naso-orbital-ethmoid (NOE) injury, often referred to as an NOE fracture, represents a significant diagnostic and reconstructive challenge.36,37 This region houses the lacrimal apparatus, medial canthal ligament, and anterior ethmoidal artery. CSF rhinorrhea is common following NOE fractures.38 In one series, Cruse et al have reported that central nervous injuries are present in 51% of cases and 42% have CSF drainage14 (Fig. 17-15).

FIGURE 17-15 Traumatic telecanthus following NOE injury showing measurement of intercanthal and interpupillary width..
Assessment of these injuries requires close attention to the soft tissue and osseous structures and an accompanying CT scan, with both coronal and axial views.39 Physical examination is likely to demonstrate a severely fractured nose, often with comminution and posterior displacement. The nasal bridge is widened and the nasal complex splayed. Epistaxis is common. Traumatic telecanthus (see Fig. 17-15) may occur because of disruption of the medial canthal ligament. The average intercanthal distance for a white adult is 28 to 35 mm, which is approximately half of the interpupillary distance. Halving the interpupillary distance is a useful tool on the preliminary physical examination because severe periorbital edema is preset in most cases. Traumatic telecanthus is suspected when the intercanthal distance is greater than 35 mm; a measurement more that 40 mm is diagnostic for this type of injury.40 Epiphora following trauma to this area is likely the result of damage to the lacrimal apparatus. Narrowing of the palpebral fissure, obliteration of the caruncle, and flatting of the base of the naso-orbital valley are more likely to be noted following the resolution of edema.
NOE fracture repair requires a broad knowledge of anatomy and should be based on anatomic reconstruction; the repair should be done early, when possible. Inadequate reconstruction or delay in treatment may result in a multitude of suboptimal results, generally including midface retrusion, blunted palpebral fissures, ocular complications, nasal deformities, and cerebrospinal fistula formation.14,41–44
These injuries may occur with other midfacial fractures, may be isolated or bilateral, and may have different patterns on either side of the midline, depending on the mechanism and velocity of impact.40,44–49 Repair of these fractures requires surgical approaches that provide wide exposure and allow an anatomic repair. Attention to the anatomy of this region, in particular the intercanthal distance, is essential to a satisfactory outcome.
Anatomy
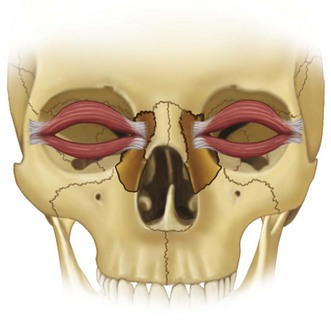
The NOE region is made up of the cranium, nose, orbit, and maxilla (Fig. 17-16). The frontomaxillary buttress provides structural support to this region and serves as the stabilization point for reconstruction. The associated lateral buttresses are the frontal bar superiorly and the zygoma and inferior orbital rims inferiorly. The medial portion of the buttress contains the perpendicular plate of the ethmoid, lacrimal ones, and lamina papyracea. These bones are thin, fragile, and form a so-called crumple zone that is predisposed to medially displaced comminuted fractures46 Reconstruction of the bony architecture is necessary in this area to control orbital volume.
The medial canthal tendon is a fibrous extension of the tarsal plates. It divides into two limbs, anterior and posterior. The anterior limb is larger and stronger, attaches to the frontal process of the maxilla, and functionally pulls the medial commissure of the eyelid forward and down.50 The posterior or deep limb is comparatively thinner, inserts into the posterior lacrimal crest of the lacrimal bone, and functions to maintain the eyelid’s position in relation to the globe. The posterior limb is also intimately associated with Horner’s muscle, which is responsible for the flow of tears through the lacrimal sac. A superior limb develops from an extension of fibers from the anterior and posterior limbs, which serves to encompass the lacrimal sac and functions to add the posterior and superior vector of the medial canthal tendon. The normal anatomic position of the medial canthal tendon is responsible for medial eyelid function, position, appearance, and lacrimal drainage. The degree of displacement varies significantly; the method of repair depends on whether an injury results in complete avulsion or continued attachment to variously sized bony fragments. In any situation, precise reconstruction of the osseous components and medial reattachment or stabilization of the medial canthal tendon are required to prevent telecanthus, enophthalmos, and dysfunction of the lacrimal system. When this condition is improperly managed on initial reconstruction, the ensuing deformity can be debilitating and extremely difficult to manage secondarily.
Diagnosis
Assessment of these injuries requires close attention to the soft tissue and osseous structures. An accompanying CT scan should be obtained, with both coronal and axial views.39
Physical Examination
The attachment of the medial canthal ligament is evaluated by palpating the insertion of the medial canthal ligament for crepitus or instability and by lateral traction on the lateral canthus, with evaluation of the medial canthal attachment. Bimanual examination may also be performed by application of a Kelly clamp intranasally and a finger placed externally on the central fragment; lateral displacement is then attempted.19 Indications of medial canthal ligament disruption include rounding of the lacrimal lake, epiphora, and increased intercanthal distance.
Measurement of the intercanthal and interpupillary distance is also completed at this time and compared with normal individuals of white, black, and Asian ethnicity to determine whether displacement is present and if it is unilateral or bilateral. Another excellent method of determining pretraumatic intercanthal width is to obtain preinjury photographs.51 Periorbital edema and ecchymosis will be present and must be taken into consideration when completing this examination.
Classification
A commonly used classification system developed by Markowitz et al identified NOE fractures based on their relationship to the central fragment at the site of medial canthal tendon attachment.52 The fractures are typically noted to be unilateral, bilateral, simple, or comminuted and are likely to have with different fracture presentations bilaterally. They may occur as an isolated injury or in conjunction with other major facial fractures.
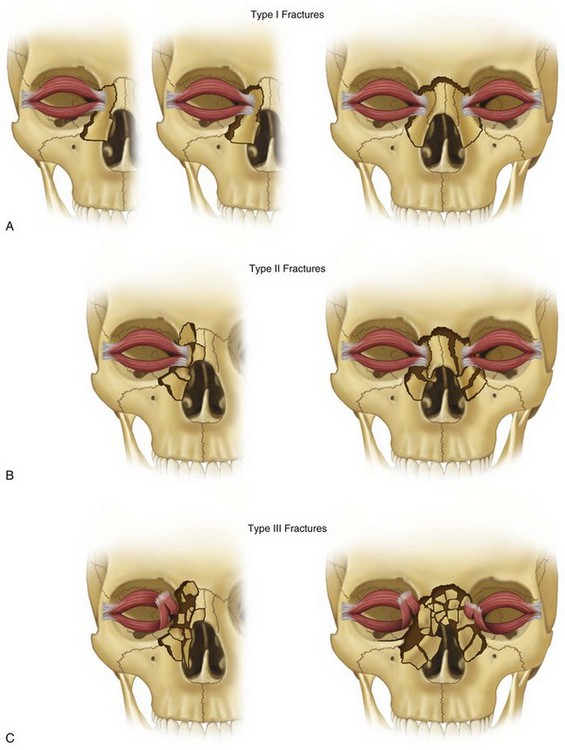
Type I
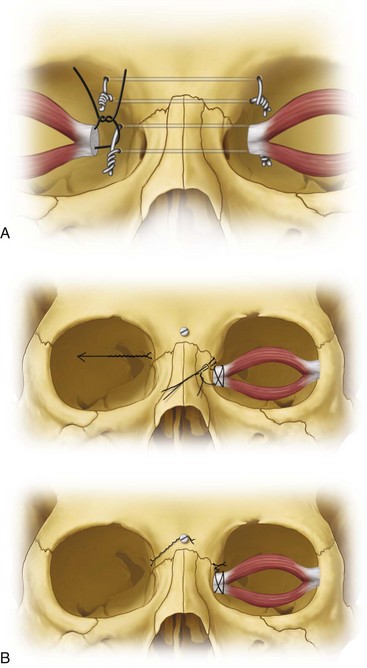
The simplest form of NOE fracture involves only one portion of the medial orbital rim, with its attached medial canthal tendon. It may occur in a bilateral or unilateral form. When the bilateral complete type I fracture occurs, there is no medial canthal tendon displacement and transnasal wiring is not required. Stabilization of the osseous segment is all that is usually necessary (Fig. 17-17A).
Type II
Type II NOE fractures may occur in a bilateral or unilateral form and may be large segments or comminuted. Most commonly the canthus remains attached to a large central segment. Reduction is usually best accomplished by control of the specific segment of bone that is associated with the canthal tendon (see Fig. 17-17B).
Type III
This fracture includes comminution involving the central fragment of bone where the medial canthal tendon attaches. The canthus is rarely avulsed completely but, on occasion, the fragments of bone are so small that reconstruction is not possible. In this circumstance, transnasal wiring of the canthus is required, as is osseous reconstruction (see Fig. 17-17C).
Treatment
Systematic Management
Systematic treatment of NOE fractures is necessary for a predictable outcome. A systematic approach of eight key steps in the sequencing of NOE fractures was described by Ellis.37 These steps include surgical exposure, identification of the medial canthal tendon and tendon-bearing bone fragment, reduction and reconstruction of the medial orbital rim, reconstruction of the medial orbital wall, transnasal canthopexy, reduction of septal fractures, nasal dorsum reconstruction and augmentation, and soft tissue adaptation.
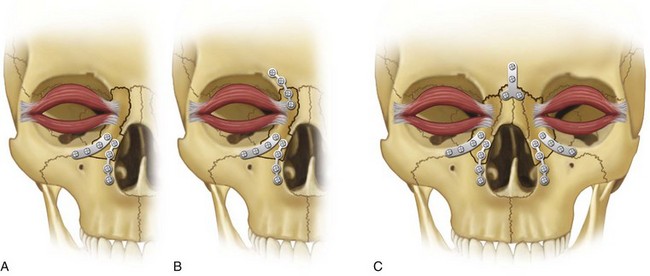
The type I fracture is best managed by three-point rigid fixation—reestablishing the relationships of the nasofrontal junction to the nasal complex, the nasal complex to the maxillary buttress, and the nasal complex to the infraorbital rim (Figs. 17-18 and 17-19). As noted, in this type of injury, medial canthal tendon detachment is rare.
The type III NOE fracture involves extensive comminution and displacement of the osseous structures, with apparent avulsion of the medial canthal tendon unilaterally or bilaterally from its osseous attachment. The principles of access and repair follow the same principles as for type I and II fractures, although establishing pretraumatic osseous and soft tissue contour is more challenging because of the level of comminution. Severe comminution of the nasal region may require a dorsal nasal cantilever-type bone graft to reestablish dorsal nasal support and nasal tip projection. This bone graft can be placed through the coronal incision and stabilized with intraosseous screws into the nasal process of the frontal bone (Fig. 17-20). Cranial bone grafts can be used for this technique and may also be needed for reconstruction of the facial buttresses. Other autogenous sites recommended for the procedure include the rib, ilium, and mandible.53 Canthoplasty, unilateral or bilateral, may be required. Direct transnasal wiring of the medial canthal tendon in a position slightly posterior and superior to the normal anatomic position will help overcome the forces of migration, relapse, and telecanthus (Fig. 17-21).
Transnasal Wiring Technique
Transnasal wiring or transnasal medial canthopexy is performed when necessary. This step follows surgical exposure, identification of the medial canthal tendon or tendon-bearing bone fragment, reconstruction of the medial orbital rim, and reconstruction of the medial orbital wall. This sequence of repair is important because reconstruction of the medial orbital rim is key to reestablishing the pretraumatic intercanthal distance,52 and reconstruction of the medial orbital wall is required to maintain an appropriate orbital volume.54–56
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses