16
Some Clinical Problems and Solutions
The topics that will be covered in this chapter are:
- Pain and instability
- Lack of saliva
- Hard and soft materials for modifying the impression surface of dentures
- The flabby ridge
- Denture breakages
- Gagging
- The burning mouth syndrome
- Disturbance of speech
Pain and instability
Table 16.1 Summary of the causes of pain (P) and looseness (L)
The most common problems associated with complete dentures are pain and instability of the dentures (Lechner et al. 1995). Many of the causes have been described in earlier chapters but to give a simplified picture they are summarised in Table 16.1. The most likely main complaints have been indicated in each case. However, it should be remembered that there is considerable overlap between the two columns, as any cause of instability may additionally give rise to a complaint of pain. It should also be stressed that there may be more than one cause of a complaint.
Persistent pain
This problem is more often seen in the lower jaw where the area available for distribution of the occlusal load is relatively small. As noted in Table 16.1, there are many possible causes of this complaint, which may be attributed to the denture design and to the patient.
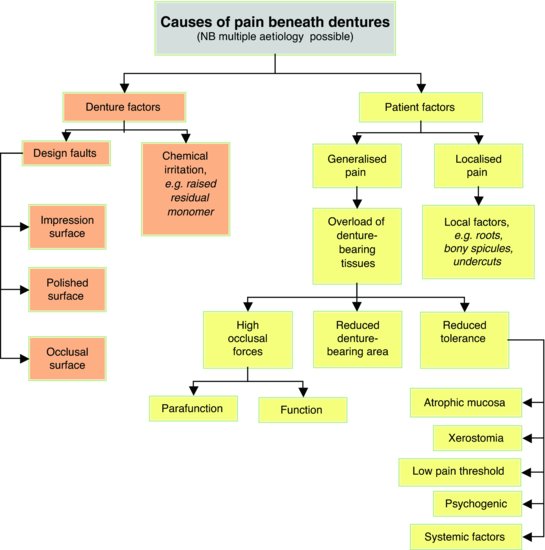
A diagnostic flow chart is shown in Fig. 16.1. The clinician may find it helpful to base the history and examination on this chart in order to arrive at a diagnosis. An example of the diagnostic process is presented in Table 16.2.
Discomfort can arise from overloading of the mucosa as a result of clenching or grinding the teeth. These occlusal habits are caused by increased activity of the masticatory muscles produced during stressful situations. Clues to such a diagnosis come from the absence of errors in denture design together with evidence of shiny wear facets on the occlusal surface of the teeth. It is helpful to ask the patient, ‘When you are not eating are your upper and lower teeth normally in contact or out of contact?’ It is not unusual for such patients to reply that their teeth are usually together and for them to assume that this is quite normal.
In treating parafunction, the patient must be made aware of the problem and should be told that teeth should be out of contact for most of the time. It is important to reassure the patient, describe the link between stress, parafunction and pain under dentures and point out that there is no sinister change in the oral mucosa. The importance of conscious relaxation should be emphasised and the patient should be strongly encouraged to leave both dentures, or at least the lower denture, out at night.
Figure 16.1 A diagnostic flow chart of the various possible causes of pain beneath dentures.
Lack of saliva
Functions of saliva
Saliva possesses the following functions in the edentulous patient (Lewis, 2009):
Table 16.2 The history taking and possible significance of the patientís answers are presented for an elderly person complaining of persistent pain in the lower denture–bearing area. The objective of the table is to stress that (1) many denture problems are multifactorial; (2) a seemingly simple complaint may have wider ramifications – especially with older patients; (3) a correct diagnosis is unlikely to be established unless a properly structured history and examination are undertaken.
- Denture retention – saliva is an essential component in the physical retention of complete dentures.
- Lubrication – the glycoproteins in saliva facilitate movement of the soft tissues during speech, mastication and the swallowing of food.
- Cleansing – saliva physically washes food and other debris from the soft tissues and from the polished surfaces of prostheses.
- Taste – flavours are perceived only when substances are in solution in saliva or other fluids.
- Digestion – digestion begins during mastication when salivary amylase starts to break down glucose.
- Antimicrobial – there are antimicrobial components, such as antibodies, in saliva which help to maintain a normal balance of the oral flora.
Problems of reduced salivary flow
A reduction or absence of saliva, known as xerostomia, is responsible for a range of symptoms resulting from an interference with some or all of the functions of saliva listed above. As a result, a general and significant reduction in the quality of life can result. Reduced retention of dentures can be a particular problem for edentulous patients. However, the literature is inconclusive about whether or not treating the hyposalivation has a beneficial effect on denture retention (Turner et al. 2008). There may also be an increased susceptibility to denture trauma resulting in complaints of pain and in some cases the burning mouth syndrome, discussed later in this chapter (Soh et al. 2007). A complaint of dry mouth can occur in the absence of the clinical signs of dryness (‘symptomatic xerostomia’). Under such circumstances the physical retention of the dentures would not be expected to be diminished.
Aetiology of reduced salivary flow
Old age per se probably does not result in reduced salivary flow rates (Scott & Baum 1990). The condition is more common in females than in males (Flink et al. 2008) and is relatively common in middle-aged and older people, the main candidates for complete dentures, with up to a third of adults complaining of a dry mouth (Locker 1995; Field et al. 2001; Marton et al. 2008; Johansson et al. 2009). This relatively high prevalence of xerostomia is likely to be due to the fact that older individuals are more likely to be suffering from systemic disease or to be taking drugs that can reduce salivary flow (von Bultzingslowen et al. 2007).
The most common causes of dry mouth (Niedermeier et al. 2000; Field et al. 2001; Guggenheimer & Moore, 2003) are:
- Adverse effects of drug therapy – over 500 medications have been implicated in xerostomia, e.g. tricyclic antidepressants, beta-blockers, diuretics, recreational drugs such as ecstasy.
- Auto-immune disease (Sjögren’s syndrome) – this affects 1-3% of the UK population, particularly middle-aged females.
- Poorly controlled diabetes – reduced salivary flow results from raised blood sugar, and increased micturition which can lead to dehydration.
- Radiotherapy – an increasing number of patients with malignant disease of the head and neck receive radiotherapy as part of their treatment. Salivary tissue is very sensitive to radiation and so, in spite of strategies to limit exposure of the salivary glands reduction in salivary flow often follows.
- Other causes – these include depression, chronic anxiety, dehydration, mouth breathing and smoking.
Management of dry mouth
In clinical xerostomia there are intra-oral signs of dryness such as a dry, atrophic mucosa and lack of saliva pooling in the floor of the mouth. The clinician can check the dryness of the buccal mucosa simply and quickly during the examination of the patient by carrying out the ‘mirror test’. For this the clinician lightly presses the face of the mirror against the buccal mucosa and then tries to remove it. If the mirror comes away easily the mucosa is still covered by a substantial film of saliva; if the mucosa adheres to the mirror then it is dry. Referral to the patient’s general medical practitioner or to a specialist in oral medicine is likely to be necessary if a more thorough investigation is indicated.
Measures for managing xerostomia may be local or systemic
Local measures
- Artificial saliva. In cases where the salivary flow rate cannot be improved, limited relief may sometimes be obtained by the use of artificial saliva (Ship et al. 2007; Oh et al. 2008). These preparations are usually based on either carboxymethylcellulose or mucin. But it should be remembered that as the mucin preparations are of animal origin, they may not be acceptable to vegetarians or to some religious groups. Some patients with dry mouth find that frequent sips of water or milk are equally, or even more, effective than artificial saliva in alleviating their symptoms.
- Denture and oral hygiene. It is very important for a denture patient with a dry mouth to maintain an excellent level of denture hygiene. The likelihood of the proliferation of Candida albicans and other microorganisms is increased in xerostomia and therefore unless denture hygiene is maintained at a high level the denture is likely to be rapidly colonised by the microorganism, increasing the likelihood of oral disease (Almstahl et al. 2008; Leung et al. 2008). Motivation and instruction of the patient, followed by monitoring the quality of denture hygiene, are essential.
- Denture retention. In cases where an intractable dry mouth gives rise to a persistent problem of loose dentures a denture adhesive will usually provide some improvement in denture function.
Systemic measures
- Treatment of an underlying disease. It might be possible, for example, to change an existing xerostomic drug to one less liable to reduce salivary flow. Also if the patient is diabetic, an improved glycaemic control will alleviate the xerostomia.
- Increasing fluid intake. As there is a relationship between fluid intake and secretory performance, it is essential that the patient is kept well hydrated.
- Sialogogues. Pilocarpine can stimulate salivary flow where some functional salivary tissue remains, particularly in drug-related xerostomia, but it commonly has unpleasant side effects such as increased sweating. The dry mouth may also be occasionally alleviated by sialogogues such as chewing gum or glycerine and lemon mouthwash.
Hard and soft materials for modifying the impression surface of dentures
In a chapter dealing with problems and solutions it is logical to consider materials which can be used to modify the impression surface of a denture to overcome some of these problems; these materials can be either applied by the clinician at the chair side or constructed by the dental technician in the laboratory.
The materials may be classified as follows:
- Hard materials
- Short-term soft lining materials
- Long-term soft lining materials
Hard materials
Recent years have seen the development of a group of useful materials, frequently described as chair side reline materials, which can be used to modify the impression surface of an existing denture.
Composition
Commonly these materials consist of a powder containing polyethylmethacrylate together with a liquid monomer, butylmethacrylate. The important point to make is that monomeric methylmethacrylate, a tissue irritant, is avoi-ded. Many of the products include a bonding agent to enhance the adhesion of the material to the existing denture polymer (Mutluay, 2005). The available materials vary in working time, setting time and viscosity.
Clinical applications
These materials can be immensely useful for relining dentures. As they can be used at the chair side a ‘one-stop’ reline technique can be employed. This has great benefits in the following situations:
- A laboratory reline would require the patient to be without any denture for an inconvenient length of time. This is likely to include patients who only have one set of dentures that they can wear and who find being without dentures for any period of time socially unacceptable. In particular, immediate denture patients usually fall into this category. The materials can be used to improve the fit of an immediate denture that has become loose as a consequence of bone resorption. This hard material is usually added after initial healing of the residual ridge has occurred. In the early days following the extraction of teeth it is more likely that a short-term soft lining material will be used (see below). The great advantage in changing from the short-term soft lining material to the hard material after the initial healing period is that the latter can be trimmed and polished for a high-quality finish and is much more durable. The ‘one-stop’ reline technique can also be very useful when treating older patients, particularly when a domiciliary service is being provided.
- A reline is required, but it is not necessary for it to last for much longer than a year. After this period of time the hard chair side relining material is likely to have deteriorated to the point when replacement is required. Again, the immediate denture patient is likely to fall into this category, as after a year the chair side reline will usually need replacing by a permanent rebase or by a replacement denture.
- Where a direct technique is indicated. A chair side reline is a direct technique that does not involve the intermediate stages of impression taking, cast pouring and laboratory processing. There are therefore fewer opportunities for errors to creep into the process and consequently there is the potential for greater accuracy.
Clinical performance
Clinical trials have shown that the best of this group of materials are convenient to use and provide immediate improvement of fit and comfort. Over a period of time there is a loss of material, especially at the borders of the denture; this loss is more apparent in the lower denture. However, the loss does not appear to cause marked deterioration of fit or comfort (Hayward et al. 2003). The better materials should be regarded as having a working life of about one year. The surface can be cleaned in the normal manner and there is relatively little discolouration (Hayward et al. 2003).
Short-term soft lining materials
Composition
Most materials are supplied in a powder/liquid form. An alternative presentation is in a ready-to-use sheet form which can be found in one product available to the dental profession and in several ‘over the counter’ products available directly to the general public. The method of self-treatment is to be discouraged, except as an emergency measure, as it is not based on a sound clinical diagnosis and can result in severe tissue destruction. It is essential that traumatised tissue is examined by the clinician and that rational, rather than empirical, treatment is prescribed. The composition of the powder/liquid types is as follows:
- Powder – polyethylmethacrylate, or copolymers of polyethyl/methylmethacrylate.
- Liquid – a mixture of an aromatic ester, such as dibutyl phthalate, which acts as a plasticiser, and ethyl alcohol.
The setting process
After the powder and liquid have been mixed, the ethyl alcohol causes swelling of the polymer particles and permits penetration by the ester so that a gel is formed. This is a physical change; there is no chemical reaction. The presence of ethyl alcohol is necessary to initiate this process and the amount present in the liquid is related to the particle size and molecular weight of the polymer; the higher the alcohol content, the shorter the gelling time (Murata et al. 1994). If particle size and molecular weight are low, then the ethyl alcohol content can be kept to a minimum. This state of affairs is desirable as large amounts of ethyl alcohol produce an unpleasant taste and sensation in the mouth.
Some materials suffer from dimensional change as a consequence of water absorption and solubility of the material (Murata et al. 2001). The ethyl alcohol and plasticiser are leached out reducing the flow of the material with time and causing the material to harden and shrink. The more ethyl alcohol there is in the formulation, the quicker is the rate of hardening. The rate can also be accelerated by dietary solvents found in fatty foods and foods containing alcohol (Jepson et al. 2000).
Clinical applications
Short-term soft lining materials are placed in existing dentures for the following reasons:
- Tissue conditioning. For tissue conditioning, the material is applied for a period of a few days to the impression surface of a denture when the denture-bearing mucosa is traumatised and inflamed. The tissue conditioner acts as a cushion absorbing the occlusal loads, improving their distribution to the supporting tissues and encouraging healing of the inflamed mucosa.
- Temporary soft reline. A short-term soft lining material can be used to improve the fit and comfort of a denture, typically an immediate restoration.
- Diagnosis. A short-term soft lining material can be used as a diagnostic aid where the clinician wishes to check the reaction of the patient and the tissues to an improvement in fit of a denture. If the patient is happy with the change made by the short-term lining material, the clinician has first-hand evidence of the degree of improvement that can be expected if a long-term soft reline is to be inserted. An important advantage of this approach is that the information has been obtained by a reversible procedure. If the patient is unhappy the lining can be removed and the denture returned to its original state.
- Functional impression. A short-term soft lining material can be used as a functional impression material applied to the impression surface of a denture for the purpose of securing an impression under functional stresses.
- Recording the neutral zone. The ability of these materials to be moulded by the oral musculature over an extended period of several minutes allows them to be used to record the neutral zone (p. 185).
It is probably true to say that these products are used less as functional impression materials than as tissue conditioners and temporary soft lining materials.
Relevant properties
The properties of soft lining materials which are of particular clinical relevance are:
- Softness. This property of the set material alters with time. The longer the powder/liquid types are left in the mouth, the harder they become. However, those with a low alcohol content remain softer for longer and are thus more effective as tissue conditioners.
- Viscoelasticity. The current range of available materials varies considerably with respect to viscoelastic behaviour and each material can be modified in this respect by altering the powder/liquid ratio, although the scope for doing this is limited. The gelling material should have sufficient flow to allow it to adapt accurately to the mucosal surface, but should not flow so readily that most of it is squeezed out when the patient occludes on the dentures. Those materials with a low alcohol content exhibit plastic behaviour for the first few hours after mixing. Elasticity increases as the materials age, but some of the powder/liquid materials are elastic from the start and are therefore unsuitable as functional impression materials.
- Dimensional stability. Those materials with a low alcohol content exhibit good dimensional stability for the first few hours after mixing. Thus they are the materials of choice if a functional impression is being obtained (see below). It is apparent that these properties vary from brand to brand, and the clinical importance of each varies with the particular use to which the material is being put. Therefore it is important for the clinician to be able to select the best material for the job in hand. This topic is discussed further in the next section ‘Clinical implications’.
Clinical applications
Tissue conditioning
A material used for this purpose should ideally be soft and elastic so that it provides a good cushioning effect.
If a tissue conditioner is applied to the impression surface of an old denture, it will help to resolve inflammation of the denture-bearing tissues. However, as the inflammation is reduced the traumatised mucosa will alter in shape so that the lining ceases to be accurately adapted to the mucosa, thus slowing the rate of healing. Of course, if the material remains soft and elastic, its deformation by relatively small forces in the mouth will adapt it to the tissues while it is under load. Nevertheless, it is a wise practice to replace the tissue conditioner with new material after a few days to ensure that the traumatised tissue reverts to a healthy state as rapidly as possible.
If one of the less viscous products is chosen, it is particularly important to instruct the patient to close on the dentures with the lightest possible contact while the material gels so that a thickness of at least 2 mm is maintained. Needless to say, it is essential to check that the freeway space of the dentures allows a lining of this thickness to be inserted.
It must be emphasised that a course of tissue conditioning will not be effective unless other traumatic factors, such as an unbalanced occlusion, under-extension and overextension of the base are corrected before applying the conditioning material to the impression surface.
Functional impression
A material used for this purpose should ideally:
- Exhibit plastic flow – so that it can be moulded to the denture-bearing tissues during function.
- Be dimensionally stable after the impression-taking period – so that it retains its shape while the cast is poured.
As many of the materials available for functional impressions exhibit elastic recovery even after several hours, there is the danger that in the time interval between removing the denture from the mouth and pouring the cast, the impression will change shape. The following regimen is suggested as the best way of minimising this potential problem:
i. The impression surface and borders of the denture are inspected. Where there is obvious over- or under-extension the borders are adjusted so that a gap of 1–2 mm is created between the acrylic border and the functional depth of the sulcus. This size of gap allows the functional impression material to be moulded by the sulcus tissues and at the same time provides adequate support for the impression when the cast is made.
ii. If an undercut ridge is present, it is wise to remove between 2 and 3 mm of the impression surface of the denture in the region of the undercut. This allows for an increased thickness of functional impression material so that the shape of the tissue undercut is recorded more accurately.
iii. The impression surface of the denture is cleaned and dried to ensure good adhesion. The functional impression material is mixed according to the manufacturer’s instructions and placed in the denture. After the denture is inserted into the mouth, the patient is instructed to close gently together so that the normal occlusal relationship is maintained. Natural movements of the tongue, cheek and lip musculature are encouraged to achieve border moulding of the impression.
iv. Once the material has gelled sufficiently for there to be little risk of it distorting, the denture is removed with care and excessive impression material is cut away from the polished surfaces with a scalpel, taking care to maintain the full border shape.
The functional impression material is applied to the denture approximately 1 hour before the patient is due to have a meal and the patient is asked to return to the surgery after that meal. If the patient’s report is favourable and the impression is satisfactory a cast is poured immediately. In this way, the risk of elastic recovery is reduced to a minimum, and a more accurate cast can be obtained (Murata et al. 2001). Attention to detail will lead to good results being obtained from this most useful technique.
Temporary soft lining
When a short-term soft lining material is used as a temporary reline to improve the fit of a denture it is essentially acting simply as a space-filler. Ideally the material should gel within a reasonably short time and be elastic so that it remains within the denture and can be inserted and removed over undercuts without resulting in significant permanent deformation. The available materials vary in their softness. If the lining is to be inserted into an immediate denture soon after the extraction of teeth, a relatively soft type should be selected as it will be more comfortable for the patient. On the other hand, if a reasonable amount of healing has occurred, a harder material can be chosen.
Cleaning
Beneath the surface the short-term soft lining materials are porous. If cleaning is ineffective plaque readily penetrates the lining which then takes on the unsavoury appearance of what has aptly been described as ‘an infected sponge’. Any tissue conditioning effect is rapidly lost and mucosal inflammation is aggravated as a result. Thus it is essential when using these materials to give the patient detailed instructions on how to keep them clean.
A brush should not be used on the lining as it is likely to damage the surface. Frequent swabbing and rinsing of the lining should be carried out together with daily soaking in a compatible immersion cleanser. Studies have shown that certain immersion denture cleanser/short-term lining combinations are compatible while others can be very damaging to the surface of the lining (Harrison et al. 1989). Alkaline hypochlorite cleansers, which are particularly efficient at removing plaque, are compatible with most of the soft materials and should normally be the type of cleanser recommended. Patients should be informed which specific cleansers will damage their particular lining and warned not to use them.
Long-term soft lining materials
Long-term soft lining materials distribute stress more evenly under dentures than do the hard denture base materials. They also absorb impacts that can arise from masticatory function (Kawano et al. 1997a). They can therefore be said to have a shock-absorbing or cushioning effect. Consequently it has been shown that the addition of a long-term soft lining to a complete lower denture improves the ability to bite and chew and provides general improvement in comfort when compared with hard relines (Bhat & Wright 2001; Kimoto, 2004; Mutluay et al. 2008); the lining has also been shown to improve masticatory performance (Hayakawa 2000). Heat-cured silicone materials seem to be particularly beneficial in these respects.
Indications for use
- Persistent pain under a denture
- Thin atrophic mucosa
- Parafunction
It is useful to consider the first three indications together, as a complaint of persistent pain may be due to the poor quality of the denture-bearing mucosa or to the patient’s inability to regulate gripping or grinding habits. The whole problem may be exacerbated by gross resorption of the mandible which results in the normal masticatory forces being distributed over a reduced area. It is important to make two points: first, the problem is almost always found in the lower jaw and, second, it is essential to ensure that all existing denture faults have been eliminated before deciding to proceed with a long-term soft lining:
- Replacing an existing denture which has a soft lining. Once a patient has successfully worn a lower denture with a soft lining and has got used to its ‘feel’ it is often wise to repeat the prescription. If this is not done and the new denture is made with a hard base the patient may have problems in adapting to it and reject the prosthesis as a result.
- Sharp bony ridges or spicules. The pattern of resorption of the mandible may result in sharp ridges or spicules of bone on which the denture-bearing mucosa, in essence, becomes impaled. The problem might be overcome, at least in the short term, by surgically smoothing the bone. However, there are often occasions where poor health or a strong preference by the patient to avoid surgery, are contraindications to this approach. There is also the danger that surgical interference with the mandible will speed up resorption of the bone, resulting in further destruction of the denture-bearing area. An alternative, conservative approach is to provide a soft lining, which often provides an acceptable level of comfort under these circumstances.
- Superficially placed mental nerve. Another consequence of advanced resorption of the mandible is that the mental foramen and mental nerve may become superficially placed within the denture-bearing area so that the nerve is traumatised during function. This typically gives rise to a complaint of a severe, sharp, stabbing pain from the area of the mental foramen which is brought on by biting. A soft lining restricted to the problem area may provide relief. However, it is not uncommon to find that a superficial mental nerve requires greater pressure relief than can be provided by a soft lining. If this is the case it may be necessary to cut the denture away in the area of the nerve to eliminate pressure on the nerve altogether.
Types of long-term soft lining materials
Soft linings are made either of silicone rubber or soft acrylic. The silicone materials may be cold-curing or heat-curing. The soft acrylics are heat-curing; cold-curing soft acrylics have a very limited lifespan and are best thought of as temporary soft linings.
Cold-curing silicone rubber materials
One of the most important variations in composition is the percentage of filler content. As the content increases, so does the level of water sorption with resultant worsening of dimensional stability. The rupture properties of these materials can be poor so that the soft lining is liable to tear and to become detached from the denture base. In isolated instances, the commonly used catalyst, dibutyltin dilaurate has been found to be a mucosal irritant. The abrasion resistance of these materials is poor.
Heat-curing silicone rubber materials
In contrast to the cold-curing silicones, the water absorption of these materials is low. As a result, the dimensional stability is improved and accuracy of fit is little affected by the oral environment. Improvements in rupture properties and adhesion to the denture base complete the picture of superiority.
Acrylic resin materials
Most of the materials use polyethylmethacrylate or polybutylmethacrylate as the basic polymer. The materials are heavily plasticised to create softness.
A comparison of silicone and acrylic long-term soft lining materials
The following properties are of particular clinical importance:
Figure 16.2 Penetration/recovery curves showing: (a) the gradual response of a heat-curing soft acrylic lining material; (b) the rapid response of a heat-curing silicone soft lining material to the application and removal of a load.
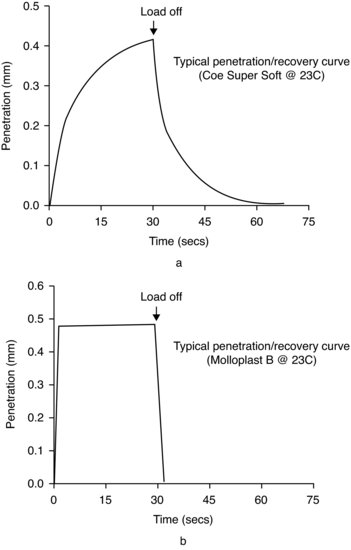
- Elasticity. As shown in Fig. 16.2, silicone rubber materials react quite differently from soft acrylic resins when a load is applied through a penetrometer. The heat-curing silicone material responds almost immediately to the application and removal of a load; it is elastic in nature. In contrast, the heat-curing soft acrylic material shows a more gradual response; it is viscoelastic (McCabe et al. 1996). The elastic nature of the silicone soft lining material is responsible for its ability to absorb shock more effectively than the acrylic lining and is no doubt the reason why it has been shown to be better at enhancing masticatory performance.
- Ageing. The properties of some long-term soft lining materials alter dramatically with age and with immersion in water. Whereas the softness and elastic behaviour of heat-curing silicone materials have been shown to remain stable with time (Dootz et al. 1993; Jepson et al. 1993; Kawano et al. 1997a) soft acrylic materials become harder with time and with immersion in water as a consequence of the plasticiser leaching out into the liquid medium.
- Bonding. Heat-curing silicone and heat-curing soft acrylic materials have similar bond strengths to the hard denture base polymer, whereas some cold-curing silicone soft liners have lower values. This problem of low bond strength appears to be restricted to those materials with a high filler content. Of particular significance is the fact that higher bond strengths are found if the soft lining is processed against polymerised polymethylmethacrylate than against the unpolymerised material. In practice this means that it is better to add a soft lining to an existing hard denture base than to process both materials at the same time (Kawano et al. 1997b).
Further practical considerations
Durability
There has been a reluctance to prescribe soft linings because of the belief that their clinical life is too short. It is possible that such a viewpoint stems from the observed hardening of soft acrylic materials and the debonding of heavily filled cold-curing silicone materials. Evidence from clinical surveys supports the long-term benefit of a heat-curing silicone soft lining. In one of the surveys (Wright 1994), a number of linings had been in situ for up to 8 years. Patients sought replacement dentures, not because of problems with the soft linings but because the acrylic teeth had worn down. Another survey (Jepson et al. 1994) showed that the survival time of a heat-curing silicone soft lining was better than a heat-curing soft acrylic resin. This last study also showed that survival time was related to thickness of the lining but that there was no benefit in increasing the thickness beyond 2 mm.
Midline fracture
A frequently reported complication is fracture of the lower denture. As the soft lining must be at least 2 mm thick if its beneficial properties are to be fully effective, a corresponding reduction in the thickness of the hard acrylic resin of the denture base is necessary to make room for the lining, which weakens the denture. Finite element analysis of lower dentures has shown the presence of high stress concentrations lingually in the lower canine areas and also around the area of the labial notch (Shim & Watts 2000). To reduce the risk of fracture a strengthener in the form of a cobalt-chromium lingual plate may be added to the denture (Fig. 16.3).
Figure 16.3 A lower denture with a cobalt-chromium lingual plate strengthener.

Cleaning
Some soft lining materials suffer from high levels of water sorption. When the lining is placed in the mouth it absorbs saliva and can be invaded by oral microorganisms. It is perhaps this set of circumstances that has led to the belief that soft linings may cause infections of the oral mucosa. Whilst soft linings do not actively support the growth of yeasts such as Candida albicans they do permit it and can in fact encourage it due to the ready availability of nutrients and to the difficulty of cleaning the surface of the lining (Wright et al. 1998). Effective cleaning is more difficult if the surface of the lining is rough. With respect to the retention of Candida albicans a rough silicone lining is worse than a rough soft acrylic lining (Verran & Maryan 1997).
It is therefore essential to achieve a smooth surface to the lining (see below), and to give the patient detailed instructions on how best to clean the lining (Davenport et al. 1986). This information should stress that the manufacturer’s recommendation with respect to temperature of the water used with denture cleansers should be followed; if not, there is a risk that there may be a detrimental effect on colour of the lining and creation of surface roughness (Handa et al. 2008).
Dietary advice, such as avoiding frequent intake of carbohydrates to restrict the supply of nutrients to the microorganisms, may also be of value. A sodium hypochlorite denture cleanser is effective in eliminating Candida albicans and Staphylococcus aureus from the lining (Baysan et al. 1998; Yilmaz et al. 2005; Ferriera et al. 2009), while not adversely affecting the mechanical properties of the lining itself. However, it will cause some loss of colour and might cause corrosion of a metal lingual plate strengthener. Microwave irradiation has been shown to inhibit colonisation by Candida albicans (Buergers et al. 2008) but should not be used if the denture has a metal lingual plate.
Adjustment
Long-term soft linings can be difficult to adjust unless the burs and stones designed specifically for trimming these materials are used. After any reshaping has been completed it is important to leave as smooth a surface as possible.
The flabby ridge
The flabby ridge is most frequently seen in the anterior maxillary region and has been reported in up to a quarter of edentulous patients (Carlsson, 1998). The bone is grossly resorbed, sometimes up to the level of the anterior nasal spine, and is partly replaced by fibrous tissue. As a result of this mobile fibrous tissue, the support for a complete denture is poor in the affected region leading to instability of the prosthesis/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


