14
Fitting Complete Dentures
Objectives of this clinical stage
The overall objective when fitting complete dentures is to ensure that the patient is given the best possible start with the new prostheses. This may be achieved by checking that:
- there is no pain when the dentures are inserted and removed from the mouth, or when the teeth are brought into occlusal contact;
- the teeth meet evenly;
- the dentures stay in place when inserted and during normal opening of the mouth;
- the patient understands:
- how to control the dentures;
- what to expect of them;
- how to clean them.
As a result of this preparation the patient should be reasonably confident when meeting family and friends. It should be remembered that to achieve this satisfactory outcome with a patient who has not worn dentures previously will require very careful advice and instruction by the clinician.
The main changes in the dentures since the try-in stage are in the impression and occlusal surfaces. This chapter will focus on the assessment and correction of these two surfaces.
Assessment and correction of the impression surface
Before inserting the new dentures for the first time, the impression surface must be carefully checked for any potential causes of pain. If found these must be eliminated to ensure patient comfort and also to avoid the adoption of abnormal paths of closure of the mandible, which may be followed to avoid occlusal pressure at the site of discomfort.
The common causes of pain arising from the impression surface of a denture are shown in Fig. 14.1:
Figure 14.1 Common causes of pain arising from the impression surface of a denture are indicated by numbers (1) surface roughness associated with sharp projections and acrylic nodules; (2) sharp edge of relief chamber; (3) overextension into bony undercuts.
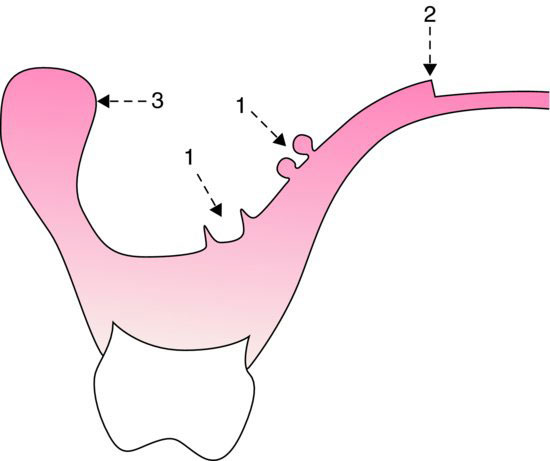
- Acrylic nodules and spicules. These are produced by acrylic resin being processed into indentations or porosity in the cast. These areas of roughness can be detected by observation of the dried denture surface and by passing a gauze napkin or cotton wool roll over the surface so that the threads catch on the offending areas. They should be carefully removed with a stone without modifying the fit of the denture.
- Sharp acrylic margins. Sharp edges can be caused by the presence of a tin-foil relief on the cast and can be identified by direct observation. Bevelling of these edges should be carried out.
- An undercut flange. A good indication of whether or not an undercut flange is likely to cause pain or mucosal injury can often be obtained by a careful visual inspection of the impression surface. A disclosing material, such as soft wax or silicone rubber, can then be used to locate the offending area precisely. A thin, even layer of the disclosing material is applied to the suspect area and the denture is gently inserted until the patient just begins to experience slight discomfort, and is then removed. The location of the undercut producing the discomfort is shown up as an area of acrylic from which the disclosing material has been displaced.
Retention and stability
The retention and stability of new dentures should be carefully evaluated at the fit stage. This may be achieved as follows.
Retention
The dentures are inserted and, after a short interval during which the denture becomes enveloped by a saliva film, they should normally stay in place during moderate opening of the mouth. The upper denture should offer resistance when pulled downwards by finger and thumb gripping the incisors. The lower denture, however, will not normally offer significant resistance to attempted displacement because it has a relatively inefficient border seal.
Stability
Neither denture should rock when finger pressure is applied alternately to either side of the occlusal surfaces in the first molar region. Horizontal displacement should not result in a shift of the centre line of more than 2 mm.
Further discussion of retention and stability can be found in Chapters 4 and 13.
Assessment of the occlusal surface
The occlusion of the dentures is checked once completion of the adjustments mentioned above have ensured that:
- each denture can be inserted and removed from the mouth without discomfort;
- firm pressure can be applied to the occlusal surface without eliciting pain.
Before discussing the methods of occlusal adjustment the possible causes of occlusal error arising from the laboratory processing of the dentures will be considered.
Laboratory occlusal errors
Causes of errors
Poor laboratory technique (Fig. 14.2) can result in the movement of individual teeth or in an increase in occlusal vertical dimension of the denture.
Figure 14.2 Laboratory causes of occlusal error (for a description of the causes, see the text).
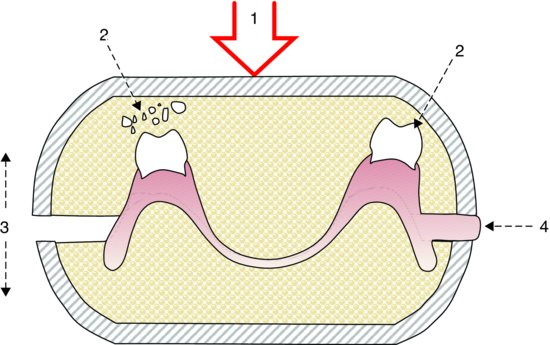
1. Excessive packing pressures resulting in the artificial teeth being forced into the investing plaster. This can occur:
- If the acrylic resin has reached an advanced dough stage and thus offers increased resistance to closure of the flask. Excessive pressure will then be needed to bring the two halves of the flask together.
- If the two halves of the flask are closed too quickly, resulting in a rapid build-up of pressure in the flask.
2. Normal packing pressures breaking the investing plaster and causing movement of the teeth when the layer of investing plaster is weakened as a result of:
- porosity in the mix;
- the use of an incorrect powder–water ratio;
- an inadequate thickness of plaster between the walls of the flask and the denture.
3. If pressure on the flask is released during the curing cycle, the two halves are likely to separate, thus increasing the occlusal vertical dimension of the completed denture.
4. Separation of the two halves of the flask by a layer of excess resin which should have been removed during trial closure of the flask. This ‘flash’ results in an increased occlusal vertical dimension of the denture.
In spite of taking all due precautions to prevent the errors just described, small occlusal inaccuracies invariably occur. It has been shown that a processed denture exhibits an average increase in height of 0.5 mm and a shift in tooth contact towards the posterior region. These errors can be corrected in the laboratory if a split-cast mounting technique is used.
Correction of errors
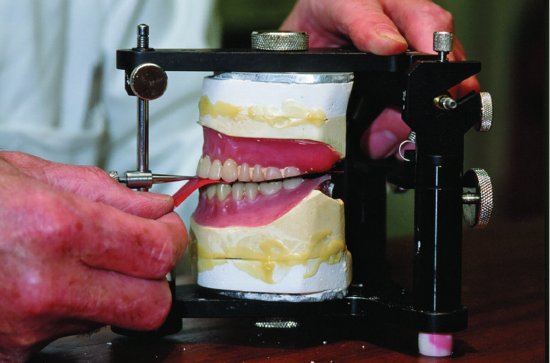
Laboratory occlusal errors can be effectively corrected by using the split-cast technique. This technique involves replacing the processed dentures, still on their casts, back on to the articulator in exactly the same jaw relationship as when the trial dentures were produced (Figs. 14.3–14.5). Any deflective occlusal contacts resulting from displacement of individual teeth can then readily be seen. An overall increase in occlusal vertical dimension will be indicated by the incisal pin failing to make contact with the incisal table.
Figure 14.3 Split-cast mounting technique (1). The trial dentures had been mounted on an average movement articulator. Before the master casts were plastered to the articulator, location grooves were cut into each cast. A film of petroleum jelly was applied to the location grooves and to the peripheral areas of each cast; as a result, the master casts were readily detached from the topping plaster before processing.
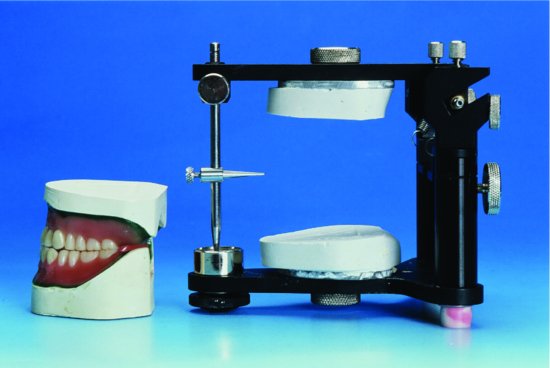
Figure 14.4 Split-cast mounting technique (2). In the laboratory, the denture, still seated on the cast, has been removed from the investing plaster after processing. It can now be relocated onto the topping plaster via the locating grooves.

Figure 14.5 Split-cast mounting technique (3). In the laboratory, the master casts, on which the dentures are still seated, have been accurately relocated on the topping plaster and secured with sticky wax. The occlusion can now be refined.
There is evidence to show that if complete dentures are processed by injection moulding rather than the more common compression-moulding technique there is significantly less incisal pin opening and generally fewer occlusal inaccuracies (Nogueira et al. 1999).
Clinical occlusal errors
If all appropriate precautions have been taken while processing the dentures, any remaining occlusal errors detected when the dentures are placed in the mouth are likely to be primarily of clinical origin and to have passed undetected at the trial stage.
The objectives of adjusting the occlusion on the finished dentures are to achieve:
- occlusal balance in the intercuspal position;
- a balanced articulation.
Occlusal errors can be identified and subsequently corrected by occlusal adjustment with or without remounting the dentures on an articulator.
Occlusal adjustment without remounting the dentures on an articulator
In general, small occlusal discrepancies in the absence of a horizontal slide can be corrected effectively by chair side adjustment following a thorough intra-oral assessment using the methods described in the following.
Identification of occlusal errors
i. Visual assessment. Visual assessment of occlusal contact relationships of the dentures by the clinician can be an effective way of recognising obvious deflective occlusal contacts and slides which occur after the initial contact. It is essential that the clinician bases an assessment of the occlusion on the initial contact of the dentures rather than on the final occlusal relationship, as the latter can be the product of the dentures tipping and of mucosal displacement.
ii. Feedback from mucosal mechanoreceptors. A usually reliable guide to identifying occlusal imbalance in dentures is the patient’s sensory nervous system, as the mechanoreceptors in the oral mucosa are capable of fine pressure discrimination. They are generally able to detect the presence of a deflective occlusal contact, but may not precisely identify the specific site that should be adjusted. This will usually require the use of articulating paper.
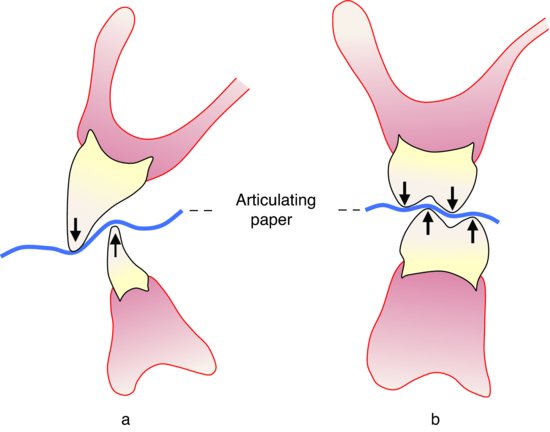
iii. Articulating paper. When searching for deflective contacts with articulating paper, using the technique described in the next section, it should be remembered that articulating paper marks can be very misleading. False marks can readily be created because of the following reasons:
- Even thin articulating paper may fill the space between non-occluding teeth and mark areas of the occlusal surfaces that are not actually contacting.
- Mucosal displacement and tipping of the dentures can bring non-occluding teeth into contact with the articulating paper.
- The vertical overlap of teeth associated with cusp/fossa relationships and vertical overlap of anterior teeth can ‘crimp’ the articulating paper and produce false marks (Fig. 14.6).
Figure 14.6 Articulating paper can mark the teeth that are not in contact when it is ‘crimped’ by a deep vertical overlap or by posterior teeth with cusps.
Correction of occlusal errors
This may be undertaken as a two-stage process:
i. Produce a balanced occlusion in the muscular position.
- When the dentures have been made comfortable, the patient is encouraged to relax and is then instructed to open and close without making occlusal contact. In this way, the pattern of jaw movement is largely determined by sensory input from the temporomandibular joint receptors and from the muscle spindles in the muscles of mastication.
- Sensory input from the mechanoreceptors in the denture-bearing mucosa is then introduced by asking the patient to continue opening and closing in a relaxed manner but to make initial, light contact on the teeth and to report on the location of that contact. It is essential that the patient refrains from heavy contact; this ensures that the joint sensory input prevails and thus prevents alteration to the path of closure of the mandible. In addition, it should be remembered that heavy contact is likely to compress the underlying mucosa, or tip the dentures, and so mask the presence of the deflective contact.
The majority of patients are able to offer such comments as ‘The dentures are meeting on the left side first of all’, or ‘I am meeting on the back teeth only’. This discrimination comes from stimulation of the mechanoreceptors in the denture-bearing mucosa. It is the clinician’s task to interpret this evidence, and with the assistance of additional tests eliminate the deflective contacts.
- A piece of thin horseshoe-shaped articulating paper is inserted between the teeth and the patient is asked to repeat the jaw movements. A single strip of articulating paper should not be placed on only one side of the dental arch as this is likely to induce jaw movement to that side.
- Instructing the patient how to occlude onto the articulating paper needs to be carried out with care. The request to ‘bite together’ is not advisable as it encourages protrusion of the mandible towards an edge-to-edge incisal relationship and consequently an incorrect result. On the other hand, ‘close on your back teeth’ will encourage a normal closure pattern. Once the desired position has been obtained the patient is requested to tap the teeth together several times in that position in order to mark the occlusal surfaces.
- Adjustment of the occlusal surfaces should be made only on those markings made by the articulating paper which coincide with the patient’s comments. The process is repeated until the patient reports that the teeth meet evenly.
ii. Produce a balanced articulation. Having established a balanced occlusion in the muscular position, the clinician should normally check that there is an area of balanced articulation 1–2 mm around this position. Articulating paper is again used to mark interfering contacts requiring adjustment. With a horseshoe of articulating paper between the teeth the patient closes into intercuspal position and then slides the mandible into the lateral or protrusive position being assessed.
The occlusal vertical dimension and occlusal balance in intercuspal and muscular position normally depend on contact between the palatal upper cusps and the buccal lower cusps of the posterior teeth (Fig. 14.7a). These cusps are therefore known as supporting cusps.
Having established even occlusal contact in muscular position, further adjustment of these supporting cusps should be avoided wherever possible. Thus, if, in a lateral occlusal position, a deflective contact is detected on the working side between a buccal upper and buccal lower cusp, it is the buccal upper cusp (BU) that should be reduced. Similarly, if interference is observed on the working side in lateral occlusion between a palatal upper and lingual lower cusp, it is the lingual lower cusp (LL) that should be reduced (Figs. 14.7b and 14.7c). This approach to correcting the occlusion on the working side is known as the BULL rule.
However, this rule cannot be applied to the correction of deflective contacts on the balancing side, because here both upper and lower supporting cusps are in opposition (Fig. 14.7d). It is usually possible in this situation to reduce the interfering contact without eliminating the supporting contact. If this is not possible, it is necessary to adjust one of the offending cusps and to accept loss of supporting contact in this area. Overall balance in muscular position will not be lost as a result.
Figure 14.7 (a) Contact between supporting cusps maintains the occlusal vertical dimension and occlusal balance in tooth pos/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


