14
Ethnocultural diversity
INTRODUCTION
This chapter, in three parts, explores the influence of culture on health beliefs, behaviors, and outcomes in frail elders who are part of an immigrant population. The first part presents the concept of culture and acculturation. It explores the models used to explain the health and social outcomes of immigrant groups, and it describes the demographics of immigrant groups with an emphasis on several multicultural countries. The second part examines the health, particularly oral health, of ethnocultural minority groups and explains how oral health can relate to cultural background. These include oral health status, beliefs, attitudes, and knowledge, as well as oral health-related practices, use of general healthcare services, and barriers to care. The last section identifies the gaps in our current knowledge about the systemic and oral health of older immigrants and discusses future challenges to health promotion and clinical practice.
POPULATION CHANGE AND DIVERSITY
Most Western countries are culturally diverse, composed of numerous ethnocultural groups (e.g., indigenous people, recent immigrants, established immigrants and their descendents) coexisting within a larger, predominant culture, and creating multicultural and multiracial societies. In any given year, hundreds of thousands of people migrate across national borders to a new environment. As a result, the size and diversity of ethnic mix in various countries are increasing. Whether this movement is voluntary or involuntary, temporary or permanent, these people are “cultural strangers” in an unfamiliar environment.
Changes in the composition of the population create a new demand for appropriate content in multicultural policies affecting all aspects of society––political, social, economic, and academic (United Nations, 2004). Sociologists and anthropologists identify the quality and nature of social interactions, while psychologists study the impact of culture on perceptions and attitudes. Gerontologists and demographers have noted the impact immigration has had on the aging of populations. In some countries, such as Australia and Canada, immigration by older adults is one of the factors contributing to the graying of that society (Minichiello and Coulson, 2005). In contrast, immigration has protected the United States from becoming an “aging” country because of the influx of younger families, and higher birthrates among immigrants.
In response to both the opportunities and challenges of multicultural societies, government officials seek to establish policies and allocate resources, while educators and service providers attempt to deal with multilingual and multicultural needs. For health professionals and healthcare providers, this trend involves working with different cultures and across cultural borders to create more sensitive and appropriate healthcare. However, more than that, they need strategies to facilitate rapport with people who are culturally different from themselves. This has set an agenda of educating the workforce to be more responsive to ethnocultural differences.
Health needs of immigrants are exacerbated by a number of factors. Immigrant populations not only bring with them hopes and aspirations to their new country, but also a set of traditions, values, and beliefs from their native culture. Settlement experiences vary for each immigrant, depending on factors such as language and communication skills, migration circumstances, the support of family and friends, financial resources, and the geographical location of immigrant communities. For some immigrants, the settlement period prior to living independently can be relatively short, while for others, it can last several years or forever. Immigrants with cultural characteristics markedly different from the dominant society will experience greater difficulties relative to immigrant groups whose cultural values are closer to the dominant society. These and other barriers––real or perceived––such as language and communication; lack of familiarity with the nature and location of health services; fear of, and hostility toward, the mainstream society; premigration cultural beliefs; and knowledge of the dominant culture’s customs, all have a potential impact on every aspect of life to create a unique set of health risks for immigrant groups. Moreover, in many situations, the risks cannot be reduced by established procedures in the host country, so it is not difficult to accept and expect that different approaches may be required for immigrants from different cultures.
The impact of increasing diversity on social and health services, and on the health of immigrants, is all but unknown, although certainly not inconsequential. Elderly immigrants pose special challenges for health workers because they have difficulty adapting to their new surroundings and often maintain unrealistic psychosocial expectations (Mariño et al., 2001; Soldov and Poon, 2001; Waxler-Morrison et al., 2005). There is little doubt, for example, that elderly members of ethnic minorities are prone to social isolation, which is linked to an increased risk of morbidity and mortality (Cacioppo and Hawkley, 2003). Furthermore, when considering the mediating factors and experiences of older immigrants, consideration should be given to the diverse reasons why older people emigrate. Mostly they move to join their children under a family reunion or family reunification visa, or to seek asylum as refugees (United Nations, 2004). However, no matter how or when they arrive, older immigrants are likely to have different experiences and needs than the indigenous residents of the host country.
WHAT IS CULTURE?
The past quarter century has witnessed worldwide changes that highlight the relevance of culture in healthcare. Terms such as “culture,” “race,” “language spoken,” or “country of origin” have been used interchangeably and often without clarity. Race, for example, is a biological concept based on genetic features, while “culture” embraces the values, beliefs, ceremonies, and ways of life characteristic of a given group (Giddens, 2006). However, to assume that all black people, whether from Africa, the Caribbean, or the United States, have the same health values and beliefs is stereotyping that can negatively influence health outcomes. Perhaps more importantly, it is potentially offensive and politically inappropriate to operate on this assumption.
Ethnicity in this chapter is defined as “the shared sense of belonging, based on characteristics such as: common religion, language, ancestry, national or geographic origin and/or other cultural attribute” (Parrillo, 1994), and an ethnic group has one or all of these elements in common. For example, it is not unusual for second or subsequent generations to maintain the identity with their ethnic group. The terms “ethnic populations” or “ethnic groups” are often misused in reference to minority populations as if other groups do not have an ethnicity. It is also frequently confused with nationality or with immigrant status (Kedar et al., 1996). For example, there are 165 different ethnic groups within the single racial group of Chinese, so the term “Chinese” certainly does not designate homogeneity. This misuse of words and assumptions of homogeneity can lead to problems when using “race” or country of birth as variables for ethnicity, or even identifying all Chinese as one ethnic group, or the more common error of categorizing all Asians as one group. The U.S. census, for instance, identifies Asians as one ethnic group that includes people of Chinese, Vietnamese, Korean, Japanese, and other national backgrounds.
Culture is an essential element of the concept of ethnicity and is used often to refer to combinations of differences in country of origin, language, customs, and even socioeconomic class (Triandis and Brislin, 1984). It has been defined as the shared knowledge, behaviors, beliefs, customs, traditions, meanings, value orientations, and norms held by a group of people, who use it to see the world in a certain way, and it is transmitted to other members of the group through time as the basis for communication and mutual understanding (Leininger, 1993; Purnell and Paulanka, 1998).
Culture is a dynamic concept that constantly incorporates new values, beliefs, and attitudes relevant only in given situations. Therefore, it is neither homogeneous nor static, nor do all members of an ethnic group necessarily strive for the same cultural elements (Erez and Early, 1993). When the cultural environment changes, so too can people change or acculturate as they adapt to varying degrees from one culture to another (Redfield et al., 1936).
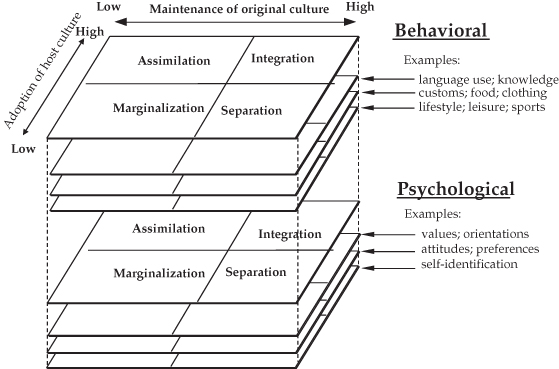
Behavioral or sociocultural acculturation relates to learning and adopting the observable aspects of the dominant culture, including social skills and the ability to “fit in” or negotiate aspects of the new sociocultural reality (Searle and Ward, 1990). It is affected by the level and length of contact with the host culture, cultural similarities, and dissimilarities, along with various personal characteristics. Psychological acculturation, in contrast, reflects the degree of personal satisfaction or agreement with defined norms of the host culture. It is a much more complicated phenomenon than behavioral acculturation, although it is less dependent on the length or level of exposure to the host culture.
Acculturation can be considered from two conceptual perspectives: a “bipolar unidimensional” model and a “two-dimensional” model, which incorporates and extends the bipolar model (Laroche et al., 1998). In the bipolar model, the acculturation process varies along a single continuum with the original culture at one end and the receiving or host society at the other on the assumption that strengthening one pole requires weakening the other (Laroche et al., 1998; Vega et al., 1998). This means that an individual becomes so integrated into the host society that newcomers and hosts are indistinguishable or assimilated. In contrast, the two-dimensional model presents the original and receiving cultures independently (Berry, 1998), whereby increased involvement in the host society does not necessarily entail rejection of the original culture. Within this model, it is possible to integrate, assimilate, separate, or marginalize in one way or another (Berry, 1998). In real life, however, the acceptance and rejection of the original and host cultures probably fluctuate dynamically between one another in a complex interplay of behaviors and beliefs (Figure 14.1). For example, an elderly immigrant might have assimilated into the host society but remain separated from the larger culture by language and food preferences.
Figure 14.1 A model of acculturation.
DEMOGRAPHY OF IMMIGRANT GROUPS
Immigrants form a substantial proportion of the population in most countries within the Organization for Economic Cooperation and Development (OECD) and, particularly, in Australia, Canada, and New Zealand, where immigration policies support the workforce (Dummont and Lemaître, 2005). Nearly 20% of the residents, young and old, in Australia, Canada, New Zealand, Luxembourg, and Switzerland today were born elsewhere. Indeed, by 2026, it is projected that perhaps one in three of all elders in Australia will have been born overseas. Similarly, in the United States by 2050, more than one-third of the older population will identify themselves as immigrants or ethnic minorities (Latinos: 17%, African-Americans: 12%, Asians: 8%) born in the United States (Passel and Cohn, 2008).
Numbers will fluctuate of course reflecting the various waves of immigration from different countries (Victorian Ethnic Affairs Commission, 1995). In the United Kingdom, the 2001 census found that about 8% of the population identified with an ethnic minority––an increase of nearly 50% since the 1991 census (ONS, 2003; Dorling and Thomas, 2004; Simpson et al., 2006). Immigrants tend to concentrate in regions as a protective strategy of “group density,” which seems to benefit health, probably by enhancing access to culturally competent healthcare and social services (Pickett and Wilkinson, 2008). The family reunification component of Canada’s immigration policy since 1994 accounts for about one-in-four immigrants, and has brought large numbers of Chinese and South Asian elders to the major cities (Ip, 2008).
GENERAL HEALTH OF ETHNOCULTURAL MINORITY GROUPS
Migrant populations in many countries are granted equal access to the healthcare system, along with the right to cultural recognition and freedom from discrimination. However, despite these supportive policies, healthcare systems do not always meet the dynamic needs of a culturally and linguistically diverse society, nor do they produce equivalent health outcomes for all ethnocultural groups (Migrant-friendly Hospitals, 2005).
The health status of immigrants is affected by ethnicity, gender, age, socioeconomic status, and migration (Julian, 2004). Recent immigrants to Australia, for example, are less healthy than other Australians if they are elderly and live alone in rented accommodation, with low income, limited social support, and inadequate English (Julian, 2004). Moreover, health disparity is compounded further by the genetic disposition of some groups to caries (Shuler, 2001). Although there is evidence that genetic disposition to disease is associated with ethnicity (Smith et al., 2000; Sproston and Mindell, 2006), it is not yet clear that it extends to the more common oral diseases.
Complementary and alternative medicines are used more often by some immigrant groups, particularly by Chinese elders, who typically combine it with Western medicine (Lai and Chappell, 2007).
Health screening of potential immigrants creates the “healthy immigrant effect” through selection of relatively healthy people––even among those who qualify under the family reunification policy operating in many countries (McDonald and Kennedy, 2004; United Nations, 2004; AIHW, 2006). Nonetheless, immigrants as they age tend more toward conditions such as diabetes, ischemic heart disease, and cerebrovascular disease, compared with the indigenous population (AIHW, 2006).
ACCULTURATION AND ORAL HEALTH
Typically, oral health is worse in older minority groups than among majority groups who live in Western societies (MacEntee et al., 1993; Mariño et al., 2001; Persson et al., 2004; Swoboda et al., 2006; Lai and Hui, 2007). Although immigrant elders have relatively fewer caries and tooth loss––probably because of traditional diets low in sugar and limited access to dentists (Newton et al., 1999)––their experiences of toothaches and other mouth problems are relatively numerous (Newton et al., 2003).
The level of acculturation is a good predictor of health-related outcomes (Liou and Contento, 2001; Mariño et al., 2001). Some cultural behavior is beneficial while others are detrimental to health and well-being (Marmot and Syme, 1976). Consequently, efforts to promote health in immigrant populations should combine traditional practices with Western concepts of care. Diets, for example, are likely to be more palatable and healthy if based on traditional foods and recipes. Likewise, health-related information is best presented in written and spoken formats that are familiar to the group and in cultural contexts that extend beyond simple translation of Western concepts and words (Guillemin et al., 1993; Mallard et al., 1997).
There is evidence that the majority of elders (not necessarily immigrants) in the United States have serious difficulties understanding and using written health materials in a prose format, finding and processing information based on numbers, or interpreting forms, lists, charts, and graphs (Rudd and Horowitz, 2005). Indeed, remarkably little attention has been paid to the oral health literacy of immigrants whether young or old, but it seems clear now that the process of acculturation should be considered carefully when framing appropriate health policies, developing health promotion and preventive and treatment programs, and planning health services for the elders in a multicultural society.
ORAL HEALTH-RELATED BELIEFS, KNOWLEDGE, AND ATTITUDES
Culturally specific beliefs in most instances are limited to people who live, congregate, and interact where a specific culture is concentrated. There are many cultural beliefs associated with susceptibility to and seriousness of dental disease. Body humor, yin and yang, and qi, for example, play a role in oral health as in general health for people from China. Losing teeth in old age is widely expected and accepted in Chinese culture, even to the point where it is considered bad luck not to lose teeth with advancing age (Kwan and Holmes, 1999). Older immigrants also worry about burdening their families; consequently, they tend to isolate themselves, use home remedies, and suf/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


