Studies have shown that surgical removal of impacted third molars is associated with an incidence of complications around 10%. These complications can be classified as the expected and the predictable ones, such as swelling and pain, and more severe complications such as fracture of the mandible. The overall incidence and severity of the complications are directly related to the depth of impaction, age of the patient, the relative experience and training of the surgeon and the time taken for the procedure.
In a study conducted by Haug RH (2005)’, the sample was provided by 63 Oral and Maxillofacial Surgeons and was composed of 3,760 patients with 9,845 third molars who were 25 years of age or older. Alveolar osteitis was the most frequently encountered postoperative problem (0.2% to 12.7%). Postoperative inferior alveolar nerve anesthesia/paresthesia occurred with a frequency of 1.1% to 1.7%, while lingual nerve anesthesia/paresthesia was calculated as 0.3%. All other complications also occurred with a frequency of less than 1%.
In a recent study by Waseem Jerjes et al (2006),1087 patients who underwent surgical removal of third molar teeth were prospectively examined to analyze the possible relationship between postoperative complications and the surgeon’s experience parameter. Seven surgeons; three specialists in surgical dentistry and four oral and maxillofacial Senior House Officers (OMFS residents) carried out the surgical procedures. The study concluded that the higher rate of postoperative complications in the residents group suggests that at least some of the complications might be related to surgical experience. This raises a number of important issues related to training. Ideally, third molar removal should only be
carried out by experienced practitioners and not by occasional surgeons. However, surgeons are not created by divine right and need training to gain the requisite level of experience. This will unfortunately result in a higher level of complications even when residents are closely supervised.
Complications may occur:
A. During the surgical procedure
B. Immediate postoperative period
C. Late postoperative period.
A. Complications during the Surgical Procedure
These are a found to occur during each major step of the surgical procedure viz.
1. Incision
2. Bone removal
3. Tooth sectioning
4. Elevation of the tooth.
Possible complication which can occur during each of the above step and appropriate preventive steps that can be taken to avoid these will be explained.
1. Complications during incision
Following the standard incision for the reflection of flap that is described above only a mild bleeding will occur which can be easily controlled. Excessive bleeding may occur in the following situations:
a.Pre-existing local inflammation which is inadequately controlled. Hence attention should be paid for adequate control of local infections like pericoronitis before contemplating the surgery.
b. Bleeding from retromolar vessels: If the incision is carried upwards towards the coronoid process instead of directing it out wards towards the cheek, retromolar vessels may be cut. These small vessels emerge from a small foramen; retromolar foramen located at the apex of the retromolar triangle or in the retromolar fossa. If these vessels are injured, the ensuing bleeding can be troublesome interfering with further reflection of the flap. The bleeding can be easily controlled with pressure pack.
c.Bleeding from facial vessels: This is an unusual complication to occur; and if it happens a torrential hemorrhage can result. The facial vessels (artery and vein) cross the inferior border of mandible at the level of the anterior border of masseter. These vessels can be injured if the anterior incision is carried too vertically down into the buccal sulcus and at the same time pierces the periosteal envelope and reaches the muscle. This mishap can be avoided by holding the sharp edge of the blade directed superiorly and making the incision from down towards the teeth. Should this misfortune occur, the bleeding can be arrested temporarily by external digital compression of the vessels where they lie over the bone. For permanent hemostasis, the artery or vein has to be clamped with a hemostat and ligated.
d. Damage to lingual nerve: Utmost care should be taken while making incision on the lingual aspect in the third molar region due to the possibility of injuring the lingual nerve which lies superficially and in close proximity to the tooth. A vertical incision should never be given on the lingual aspect of the mandible in this region for the same reason.
2. Complications during bone removal
a. Use of bur: Provided reasonable precautions are taken, use of bur will not cause problem during use. But the possibility of following complications should be borne in mind while using hand piece and bur.
•Accidental bums: An improperly maintained hand piece with a damaged bearing can get heated up during usage. If this is not detected by the gloved fingers of the operator, accidental burning of the cheek and lip of the patient will occur. This will not be felt by the patient since the above regions will be anesthetized. Burns can be very painful during the healing period and will be associated with delay in healing.
•Laceration of soft tissues: During use the bur may slip and get driven into the buccal or lingual soft tissue. This will cause laceration of the tissue and on the lingual side it may injure the lingual nerve. If the bur is revolving while the hand piece is being taken in and out of the mouth, the soft tissues of the cheek and the lips can get abraded or lacerated. Hence make sure that the micromotor has stopped completely before these acts.
•Injury to inferior alveolar neurovascular bundle: While ‘guttering’ bone on the buccal side of the impacted tooth, as the bur reaches the apex of the tooth, the mandibular canal may be inadvertently opened. This will result in brisk hemorrhage from inferior alveolar vessels, which can be controlled with pressure pack or bone wax. But sometimes damage to nerve can also occur resulting in anesthesia in the distribution of mental nerve. In rare instances the mandibular canal may be buccally placed and at a more superior level than the normal. In such cases injury to contents of the canal will occur more easily during ‘guttering’.
•Injury to adjacent tooth: Drilling in the region of the mesial surface of impacted tooth should be kept to the minimum to avoid damage to the distal aspect of the adjacent second molar.
•Injury to lingual nerve: While removing bone on the distolingual aspect extreme care is taken to protect the lingual nerve from bur by way of proper retraction. It is advisable not to remove any bone on the lingual aspect due to the possibility of causing damage to lingual nerve.
•Necrosis of bone: Even though this is a late complication, it occurs due to inadequate cooling of the rapidly revolving bur which in turn causes overheating of bone and its subsequent necrosis followed by sequestration. Profuse irrigation of the surgical site using sterile saline can avoid this mishap.
•Emphysema: Air driven handpiece has the disadvantage of causing surgical emphysema as well as driving the tooth and bone particles into the soft tissues. Retention of such debris in the soft tissues can result in postoperative infection also. Using micromotor and handpiece can avoid this complication
b. Use of chisel: Chiseling is a relatively safe, speedy, and efficient means of bone removal when used correctly. When used improperly it can also cause the following substantial damages.
•Splintering of bone: When chisel is used to remove the buccal cortical plate covering the impacted tooth, the split can sometimes extend forwards along the buccal aspect of the teeth and denude the teeth of external cortical plate. This happens because on the buccal and lingual side in the posterior aspect of mandible the ‘grains’ runs antero- posteriorly. Hence, a vertical stop cut is made first at the mesial end of the portion of the bone to be removed to avoid accidental splintering of the buccal cortical plate.
Similarly when splitting the lingual plate, if the cutting edge of the chisel is held parallel to the internal oblique ridge, a splintering of lingual plate will occur, with the split extending up to the coronoid process. To avoid this, the bevel of the chisel should be held at an angle of 450 to the bone surface and pointing in the direction of the lower second premolar of the opposite side. In its correct position the cutting edge of the chisel will be parallel to the external oblique ridge.
•Fracture of mandible: If the chisel is carelessly placed and if a blow with considerable force is delivered it can lead to fracture of mandible.
•Displacement of tooth into lingual pouch: A hard chisel blow directed on the buccal side of the wisdom tooth may fracture the lingual wall of the socket, displacing both the tooth and the fractured lingual plate into the lingual pouch.
•Injury to lingual nerve: While working on the distal aspect of the impacted third molar, slippage of the chisel can severe the lingual nerve unless it is adequately protected with a retractor.
•Injury to second molar tooth and soft tissues: Wrong positioning of the chisel blade or slippage of the instrument can injure the second molar or the adjacent soft tissue.
3. Complications during sectioning of tooth
Tooth can be sectioned using bur or osteotome: Unless this is carefully performed it can lead to the following complications:
Use of bur
•Incorrect line of sectioning of crown: The ideal site for sectioning of the crown is the cervical portion of tooth
i.e. apical to the cemento -enamel junction with bur held at right angles to the long axis of the tooth. If the bur cut is not correctly angulated or bur cut is done at different sites, it will be difficult to separate the crown and remove it.
•Injury to mandibular canal: During tooth sectioning if the bur is carried to the full width of the tooth in the superior inferior direction, to reach its ‘bed’ there is a possibility of damaging the contents of the canal. This can lead to severe bleeding from the vessels during the surgery and later on numbness of the lower lip. Hence the entry of the bur is limited to three-fourths of the width of the tooth. The rest of the tooth is separated with leverage using an instrument like curved Warwick James elevator. But this has the disadvantage of sometimes leaving a thin shelving edge of root extending forwards along the floor of the socket. This will make the subsequent root removal more difficult.
•Breakage of bur: This can occur either due to the application of a heavy pressure or due to the repeated use of the same bur. Used burs should be discarded and a fresh bur used in each case. Binding of the bur in the tooth structure is another reason for fracture. Tapering fissure burs are less likely to bind than flat fissure burs and hence the former is preferred for tooth sectioning. Recovery of a fractured bur tip from the bone or tooth structure is a difficult endeavor.
Use of osteotoine
•Compared to osteotome, chisels are ineffective to achieve a clean section of the tooth. Hence the former one is used. However, osteotome can not create a space into which the sectioned crown could be moved. Hence more than one section is necessary. Conversely if a wide bur is used then sufficient space will be created into which the sectioned crown can be moved enabling its removal.
•Fracture of mandible, injury to lingual nerve, second molar or soft tissues and displacement of tooth into lingual pouch are other possible complications associated with the use of an osteotome.
4. Complications during elevation of tooth
A number of complications which are listed below may occur during this stage of surgery:
•Fracture of impacted tooth/ root: This is considered to be the most common complication to occur during this stage and is most often due to inadequate removal of bone. It may also be due to already weakened tooth structure due to caries, resorption or restoration. Adequate bone removal and proper assessment of the tooth preoperatively can prevent this. Facture of the root also can occur. All efforts should be made to remove the root tip. It must be remembered that aggressive and destructive attempts to remove roots may cause more damage than benefit.
•Injury to second molar: Injudicious elevation of impacted tooth using second molar as the fulcrum can result in the subluxation or expulsion of the latter. This risk is more if the second molar has conical roots or when first molar is missing. Similarly fracture of the crown or dislodgement of filling / artificial crown of second molar can also occur during elevation of wisdom tooth. The incidence of damage to restorations of the second molar has been reported to be 0.3 % to 0.4%. Teeth with large restorations or carious lesions are always at risk of fracture or damage upon elevation. Correct use of surgical elevators and adequate bone removal can help prevent this. Possibility of such a mishap has to be informed to the patient preoperatively and all precautions taken to avoid it.
•Fracture of mandible: Mandibular fracture as a result of third molar removal is a recognized complication and has significant medico legal and patient care implications. It should be included in all third molar extraction consent forms (Bouloux et al 2007).3 Mandibular fracture during or after surgical third molar removal is however a rare one. The incidence has been reported to be 0.0049% (Libersa et al, 2002).4
Possible predisposing conditions, such as increased age, mandibular atrophy, concurrent presence of a cyst or tumor and osteoporosis have been implicated in increasing the risk of mandibular fracture. The preangular region of mandible is an area of lowered resistance to fracture because of its thin cross-sectional dimension and an impacted tooth occupies a relatively significant space of this weak area. The concurrent presence of a dentigerous cyst around the third molar or a radicular cyst around the second molar and the removal of the tooth and any surrounding bone to mobilize it will further weaken this area.
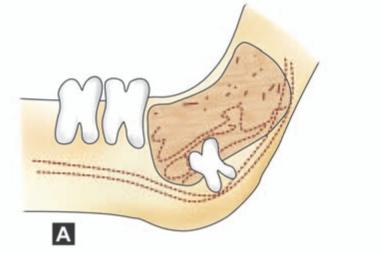
Fracture is almost always caused by the application of excessive tensile or shear forces across the superior border of the mandible in the third molar area (Fig.13.1). This results in the initiation of a fracture and its propagation along the line of weakness caused by the third molar in its socket. The instrument in use is almost always the large straight elevator and the operator tries to elevate the wisdom tooth distally and occlusally using excessive force.
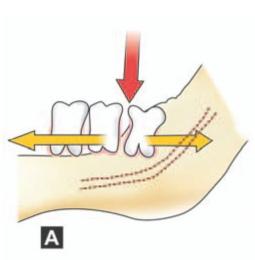
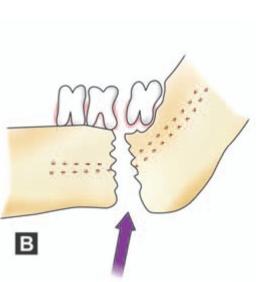
Figs 13.1 A and B: (A) Application of excessive force (red arrow) using an elevator mesial to impacted third molar without adequate removal of overlying bone, forces the adjacent teeth in opposite directions (yellow arrows) resulting in extensive shear force. This result in fracture of mandible (B) shown as blue arrow
Weakening of mandible due to excessive removal of bone or a thin and atrophic mandible due to resorption as in old age or bone weakened by local pathological conditions are contributory factors (Figs 13.2 to 13.5).
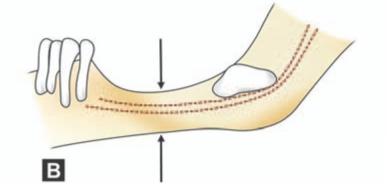
Figs 13.2A and B: Conditions causing weakening of mandible predisposing to fracture during surgical removal of impacted tooth. (A) Dentigerous cyst involving angle of mandible, (B) Atrophy of mandible in old age. Sclerosis of bone / osteoporosis is also a contributory factor
An intra-operative fracture must be suspected when a loud crack accompanies sudden loosening of a tooth that was very resistant to elevation. Inspection of the operative site will demonstrate a fracture through the tooth socket. Displacement of the fracture will be accompanied by a change in the patient’s occlusion. The diagnosis must be confirmed radiographically (Fig. 13.6).

Fig. 13.3: Extensive dentigerous cyst associated with impacted 38
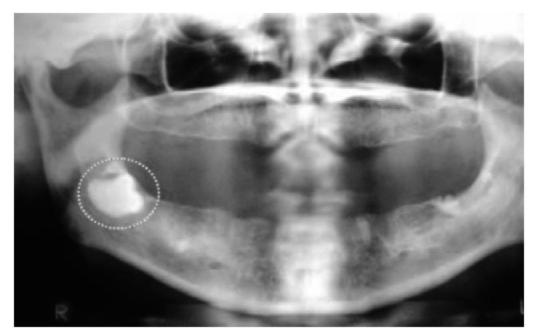
Fig. 13.4: Impacted 48 (complete bony impaction) in edentulous mandible. The angle of mandible is weakened by the presence of impacted tooth. Extensive removal of bone for extracting the tooth will further weaken the mandible predisposing to fracture
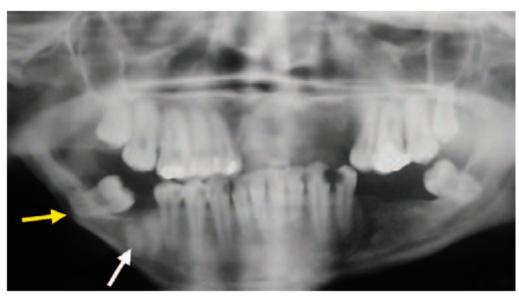
Fig. 13.5: OPG showing impacted 48 in a congenitally atrophic mandible. Note the thin amount of basal bone beneath 48 (yellow arrow), which is likely to get fractured during surgical removal of impacted 48. Note the root stumps of 46 (white arrow)
Alternatively, a patient may present in the post surgical period with a fractured jaw secondary to trauma. This happens because removal of tooth leaves a defect in the jaw and temporarily renders the jaw more susceptible to fracture from minor trauma especially when unwarranted bone removal has been done. Studies have shown that the fractures occurred 5 to 28 days after the tooth removal. It has been concluded that the major risk factor for this complication seemed to be advanced age in combination with a full dentition.
Regardless of the mechanism, mandibular fractures that occur during or soon after the extraction of the mandibular third molars are usually non displaced or minimally displaced. Such hairline fractures that extent from an extraction site are not easily identified and clinical suspicion may require CT if the initial panoramic film gives negative results. The practitioner should treat the fracture definitively just as if the patient were a trauma patient. Failure to do so may result in further complications. If this mishap occurs, the case has to be referred to a specialist for expert management. The patient should be informed of this disaster and all records relevant to the case like radiographs and clinical notes preserved. The line of management includes removal of the remaining portion of the impacted tooth followed by fixation of fracture by eyelet wiring and maxillary mandibular fixation or upper border wiring or bone plating or other methods of fixation. The line of management is dictated by the amount of bone loss, degree of displacement and the accessibility.
•Dislodgement of tooth/crown into the lingual pouch or lateral pharyngeal space: Mandibular third molars can be iatrogenically displaced into the sublingual, submandibular, pterygomandibular and lateral pharyngeal spaces. Weakened or thin lingual plate, lingual obliquity of impacted tooth, insufficient reflection of overlying mucoperiosteum, inadequate bone removal, excessive or uncontrolled force during elevation are considered the main causes for this accident. Adequate reflection of overlying gingiva and placing a finger over the wisdom tooth to assess its movement during elevation can help to a great extent to prevent this complication. Lower third molars that are pushed through a perforation in the thin lingual alveolar bone normally pass inferiorly into the mylohyoid muscle.
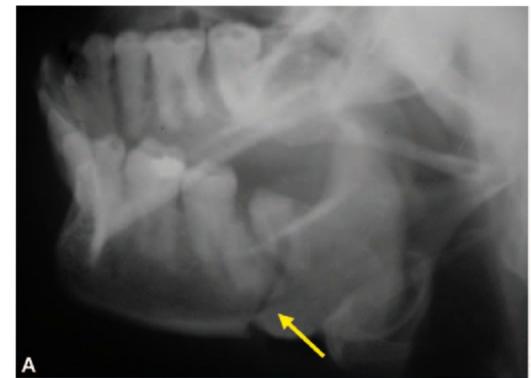



Figsl3.6 A to D: (A and B) Radiographs of mandible showing fracture of left angle of mandible (yellow arrows) in a 54-year-old female which happened during attempted removal of impacted 38 by a general dental practitioner, (C and D) Postoperative radiographs following open reduction and internal fixation using mini plates alongwith surgical removal of impacted 38
A fractured root also can be displaced into the lingual pouch during its attempted removal from the socket. See Figure 5.9 in Chapter 5.
To retrieve a tooth or root displaced into the lingual space, pressure is exerted beneath the mandible externally to prevent its further displacement downwards and at the same time using the index finger of the other hand to milk the tooth / root back into the socket through the breach in the lingual plate. If required the lingual gingiva may be reflected as far as the premolar region and the mylohyoid muscle incised to gain access to the submandibular space and deliver the tooth. It is then grasped using a hemostat and removed. Good light and
suction are mandatory for success. Also care should be taken to protect the lingual nerve. Locating the displaced tooth is challenging due to the limited working area and hemorrhage with resultant compromised visualization and blind probing that may result in further displacement. A combination of intraoral and extraoral approach may be required in certain instances to remove the tooth.
Gay-Escoda and associates (1993) reported a case in which a patient underwent extraction of a displaced mandibular third molar that was found between the platysma and sternocleidomastoid muscle. It was removed via transcutaneous approach. The authors opined that the tooth might have undergone progressive migration as a result of inflammatory reaction.
Esen and colleagues (2000)6 described a case in which a patient presented months after attempted extraction of a mandibular third molar with progressive limitation in mouth opening, edema of left neck and dysphagia. A panoramic film revealed a tooth in the pterygomandibular region. CT scans showed the precise location of the tooth at the anterior border of the lateral pharyngeal space beneath the left tonsillar region. The tooth was removed transorally from the tonsillar fossa (after completion of a tonsillectomy) through a vertical incision from the tonsillar fossa to the retromolar trigone.
In cases where the tooth / root have been further migrated downwards and backwards into the lateral pharyngeal space, the patient will be complaining of severe pain on swallowing. An extra oral approach will be necessary to reclaim the tooth and to avoid the development of an infection.
Ortakoglu et al (2002)’ reported a case of displacement of lower third molar into the lateral pharyngeal space during surgical removal. The radiological examination included panoramic, occlusal and computerized tomographic (CT) views to localize the tooth correctly. The radiological findings showed that the tooth was displaced into the pterygomandibular region. Removal of the tooth under local anesthesia via lingual approach was performed. The incision was made on the alveolar crest between the anterior edge of the ramus and lingual mucoperiosteum of the second molar. After reflection of the mucoperiosteal flap, the lateral pharyngeal space was reached by blunt dissection. In this area the tooth was located in a horizontal position and removed carefully.
Figure 13.7 shows the various radiographic views of a tooth displaced into the pterygomandibular space.


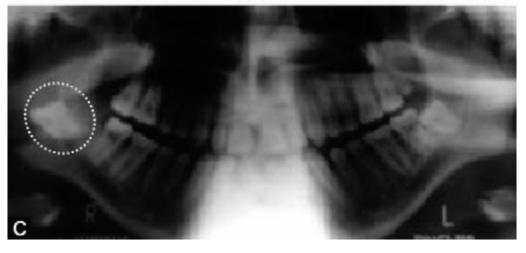
Figs 13.7A to C: Radiographic views of a tooth displaced into pterygomandibular space. (A) Periapical X-ray (note the yellow arrow pointing towards the tooth), (B) Axial CT scan showing the displaced tooth (yellow interrupted oval), (C) OPG shows the displaced tooth (white interrupted circle). [Courtesy., Ortakoglu et al]
Some authors suggest that the displaced tooth must be removed at the initial surgical attempt to avoid development of infection. However, others propose a 34 week waiting period to allow the development of fibrous tissue around the tooth thereby immobilizing it. This will enable its removal in the second attempt. Such a line of management has the possibility of development of infection unless antibiotics are administered. Delayed intervention in the event of a displaced tooth into the lateral pharyngeal space carries the risk of infection, thrombosis of the internal jugular vein, erosion of the carotid artery or one of its branches and interference with cranial nerves IX to XII (Bouloux et al, 2007).3
•Injury to mandibular canal: While elevating the tooth as the crown moves upwards, the roots may be forced downwards (Fig.13.8) with the apices piercing the mandibular canal and injuring the neurovascular bundle. This happens more commonly in cases of mesioangular and horizontal impactions. Injury to vessels can result in brisk hemorrhage. Bleeding can be controlled by immediately packing the socket with gauze. Once the initial severe bleeding is controlled, bone wax can be applied or placing a pack of Whitehead’s Varnish or antibiotic cream on gauze and leaving it in position for one or two days. Other alternatives are gelatin sponge (Gelform) or oxidized cellulose (Oxycel) to control the bleeding. Unlike the gelatin sponge, oxidized cellulose can be packed into the socket under pressure. Damage to inferior alveolar nerve also can occur in a similar situation resulting in anesthesia in the distribution of mental verve.
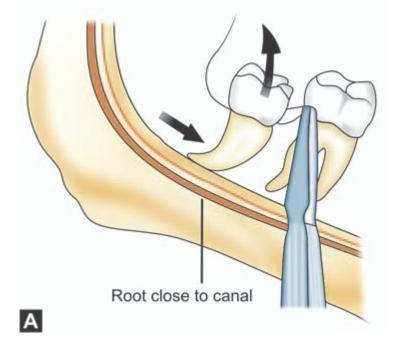
Fig 13.8A
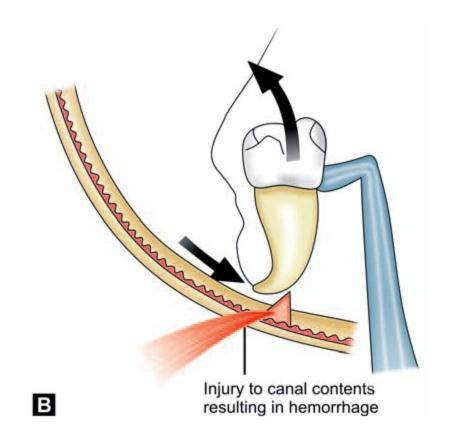
Figs 13.8A and B: (A) While elevating the tooth; as the crown moves upwards, the roots may be forced downwards with the apices piercing the mandibular canal, (B) Injury to the neurovascular bundle and resulting hemorrhage. Damage to inferior alveolar nerve also can occur resulting in anesthesia in the distribution of mental verve
While working in the depth of the socket to retrieve a fractured root, the root piece can be inadvertently pushed into the canal resulting in injury to the contents. If bleeding occurs it has to be controlled by the methods described above. Any further attempt to remove the fragment through the socket is futile and buccal cortical plate in the region has to be removed to expose the root to effect its removal.
Post Surgical Sequelae and Complications
Following the surgical removal of an impacted third molar, certain normal physiological responses will occur as sequelae. These range from mild bleeding and swelling to trismus. Even though the patient has been for warned, all these are disagreeable to the patient and hence, they should be kept to the minimum.
1. Hemorrhage: If adequate hemostasis is achieved at the time of surgery, it is unlikely for postoperative hemorrhage to occur. The incidence of clinically significant bleeding following third molar extraction ranges from 0.2 to 5.8%. Excessive hemorrhage resulting from extraction of mandibular molars is more common than bleeding from maxillary molars. In a study conducted by Chiapasco et al (1993)8 the rate of postoperative bleeding for mandibular and maxillary third molar extraction was 0.6% and 0.4%, respectively. These complications occurred mostly in cases of deep distoangular and horizontal impaction in the mandible. In the maxilla, high vertically positioned molars were most often implicated.
Jensen (1974)9 reviewed 103 cases of postoperative hemorrhage after oral surgery and made several important observations. He found that the male to female ratio was 2:1, and the age range was 21 to 45 years. There was a personal or family history of bleeding in 25% of cases. Postoperative bleeding occurred within 8 hours of the surgery in 75% of cases. The general physical condition of the patient was not affected in 84% of cases. Among cases in which the location of the bleeding was identified, 7% had an arterial source and 72% involved hemorrhage from the soft tissue. A single site of bleeding was found in 43% of cases. 10% had inadequate postoperative instructions. Local control was successful in 84% of patients. Hematological investigations revealed no diagnosable bleeding abnormalities, except in 4 patients with previously known coagulation deficiencies.
The hemorrhage can be either intraoperative or postoperative and its etiology being either local or systemic in nature. Systemic conditions such as hemophilia A or B and von Willebrand’s disease are often diagnosed early in patient’s life. Management of these patients include close coordination with the hematologist and maximum use of local measures, including the fabrication of a customized dressing plate before surgery. Anticoagulant drugs such as warfarin sodium and antiplatelet medications such as aspirin should be discontinued /switched to other drugs in the preoperative period.
Local factors that result from soft tissue damage and injury to blood vessels represent the most common cause of postoperative hemorrhage. Intraoperative and postoperative bleeding can be minimized by using good surgical technique, minimum trauma to the hard and soft tissues and avoiding damage to inferior alveolar neurovascular bundle. Nevertheless as a result of physical exertion or raise in blood pressure or due to any of the local or systemic causes (bleeding diathesis) post operative bleeding can occur.
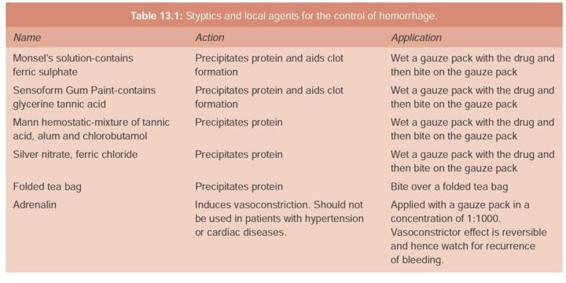
The most effective way to achieve hemostasis following surgical removal of impacted tooth is the application of a moist gauze pack over the site of the surgery and bite with adequate pressure for 45 minutes. Preparations of zinc sulphate (Zingisol) or glycerine tannic acid (Sensoform Gum Paint, Stolin Gum Astringent) can be used to wet the pack as these will act as styptics and stop bleeding (Table 13.1).
Rarely bleeding from inferior alveolar vessels or facial vessels may occur. After locating the source of bleeding, packing the site or clamping and ligature of the vessel is done. When bleeding occurs from the socket, attempting to control it by tight suturing across the socket is futile and hazardous. This is because bleeding may still continue with blood not collecting in the oral cavity but rather spreading into the tissue spaces beneath the sutures. This may lead to hematoma formation in the base of the tongue or parapharyngeal space ultimately resulting in respiratory obstruction.
Treatment of post extraction bleeding starts with a review of the patient’s medical and surgical history. Vital signs and clinical status should be monitored continuously. An attempt to quantify the amount of blood loss is helpful. Hypotension due to loss of blood volume can be measured by blood pressure and heart rate. An increase in the heart rate of more than 15 beats/minute, a decrease in the systolic blood pressure of more than 15 mm Hg or any drop in the diastolic blood pressure indicates significant hypovolemia (defined as more than 30% of total blood volume lost). Intraoral examination with adequate lighting of the oral cavity and oropharynx will allow identification of the bleeding area. Direct pressure with gauze is then applied for 20 to 30 minutes. This measure is usually sufficient to control bleeding, since the reason for bleeding is some secondary trauma associated with the patient sucking the socket. If the bleeding continues, infiltration of local anesthetic (with 1:100,000 epinephrine) should be done. In contrast to the common misconception that any clot that has formed should be left in place, all clot and debris must be removed to allow examination of the socket. The socket should be curetted and suctioned to identify the source of bleeding. If the source is not arterial, then any of a variety of local hemostatic agents can be used. If an arterial source is identified (indicated by pumping of bright red blood), the vessel must be ligated. If the bleeding is from soft tissue and is arterial in nature but does not involve the neurovascular bundle, it is usually amenable to cautery. Bleeding from bone can be managed with bone wax or various other hemostatic agents described below. If the source is intra-alveolar, then absorbable packing may be placed into the socket, and maintained thereby sutures. Oral fibrinolysis from salivary enzymes may be a cause for postoperative bleeding. The use of fibrin stabilizing agents such as epsilon aminocaproic acid or tranexamic acid may be helpful in such cases.
The following materials can be placed in the socket to achieve hemostasis. (Table 13.2).
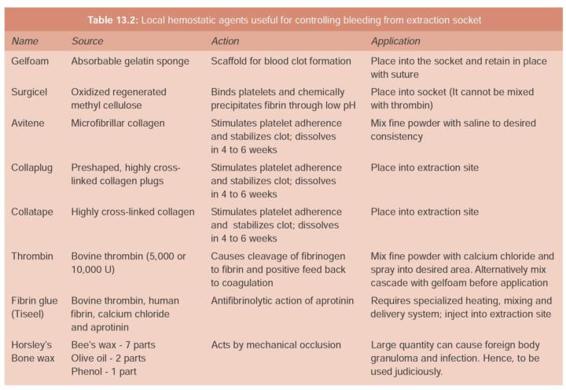
Absorbable gelatin sponge: The most commonly used and the least expensive is the absorbable gelatin sponge (Gelfoam). This material is placed in the socket and held in place with a figure – of -eight suture placed over the socket. The absorbable gelatin sponge forms a scaffold for the formation of blood clot and the suture helps to keep the sponge in position during the coagulation process. A gauze pack is then placed over the socket and is held with firm pressure.
Oxidized cellulose: Another material that can be used to control bleeding is oxidized regenerated cellulose (Surgicel and Oxycel). The material promotes coagulation better than the absorbable gelatin sponge, because it can be packed into the socket under pressure. The gelatin sponge on the other hand becomes very friable when wet and can not be packed into a bleeding socket. However, since the packing of the socket with oxidized cellulose causes a delay in the healing of the socket, this is reserved for more persistent bleeding.
Surgicel comes in knit form whereas Oxycel comes in a microfibrillar form. Surgicel has the fibers which are knit together and they are solid fibers whereas Oxycel has hollow fibers but they essentially work the same way. Surgicel is relatively acidic and is thought to cause some small vessel contraction. Like gelfoam, it works at the same point in the intrinsic pathway of clotting causing contact activation. Hence, functional clotting factors are needed in order for this to work. It is thought to be relatively bacteriostatic when compared to other hemostatic agents. The theory behind this is that because of its relatively low pH, it deactivates and denatures some of the bacterial proteins especially those related to antibiotic resistance, thus making them more susceptible to antibiotics. It needs to be applied dry and absorbs within four to eight weeks.
Topical thrombin: If there is some doubt regarding patient’s ability to form clot, a liquid preparation of topical thrombin (prepared from bovine thrombin) can be saturated onto a gelatin sponge and inserted into the socket. The thrombin bypasses all the steps in the coagulation cascade and helps to convert fibrinogen to fibrin enzymatically, which forms a clot. The sponge with topical thrombin is secured in place with a figure – of – eight suture. A gauze pack is then placed over the socket.
Collagen: This is another material that can be used to control bleeding from a socket. Collagen promotes platelet aggregation and thereby accelerates coagulation. Collagen is currently available in several different forms. Microfibrillar collagen (Avitene) is available as a loose and fluffy material that can be packed into the extraction socket. This is then held in place using suture and gauze pack. A more highly cross-linked collagen is supplied as a plug (Collaplug) or as a tape (Collatape). These materials can be more easily packed into the socket. However, they are more expensive.
If local measures are not successful then the situation needs to be managed urgently, especially if the patient becomes symptomatic. The surgeon should consider performing additional laboratory screening tests to determine whether the patient has a profound hemostatic defect. Consultation with the hematologist is advisable in such instances for the further management of the case. Figure13.9 shows the general management protocol and algorithm for the treatment of post extraction bleeding.
Airway, breathing and circulation must be assessed. As in all emergencies, airway management is the first step in stabilizing the patient. Uncontrollable intraoral hemorrhage can quickly lead to airway compromise either because of an expanding hematoma in the neck or from blood pooling in the airway. The size and spread of a hematoma depends on its vascular origin (capillary, venous or arterial) and the tissue into which it is bleeding (muscle, fat or interstitia). The location of the hematoma can be delineated using CT scan with contrast. Hematomas stop expanding when the pressure of the pooling blood exceeds the vascular pressure of the bleeding site. If the hematoma continues to expand obstructing the airway surgical exploration of the site, evacuation of hematoma and ligation of the vessel has to be done.
In the event of considerable blood loss, replacement therapy in the form of whole blood or blood substitutes should be considered />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses