CHAPTER 13
Sinus Graft Combined with Osteoperiosteal Flaps
Originality is nothing but judicious imitation.
—Voltaire
The sinus graft, although of major benefit for gaining bone mass for osseointegration, does not in itself address deficient alveolar form.1 Although guided bone regeneration, block grafting, and alveolar split graft combined with sinus grafting have been used successfully, there are few reports in the literature describing a combination of sinus and alveolar grafting.2–4 The use of the sandwich osteotomy graft to raise the residual alveolus crestally in combination with sinus grafting is an additional technique for improving alveolar form for implant placement. This approach not only results in an increase in bone but also can lead to a relatively stable alveolar crest morphology when compared with alternative approaches.5–8
Though technically challenging, a sandwich osteotomy 9,10 can be performed from access through the lateral sinus osteotomy site.11 Similarly, an alveolar split graft (book flap) made over the sinus cavity provides access to the sinus floor from a transalveolar approach.12 Through these methods, an increase in both height and width can be obtained simultaneously. A third approach, the intra-alveolar split osteotomy, performed after the horizontal segment cut of the sandwich osteotomy, increases the height and width of the alveolar process. However, sufficient bone must be available to allow the intra-alveolar split, usually a minimum of 4 mm (see chapter 8).
Interpositional bone grafting, with all of these approaches, extends upward into the sinus floor beneath the previously elevated sinus membrane. Relatively modest intra-alveolar expansion and sinus membrane elevation create a large cavity that is particularly well suited to placement of a recombinant human bone morphogenetic protein 2 (rhBMP-2) graft.13
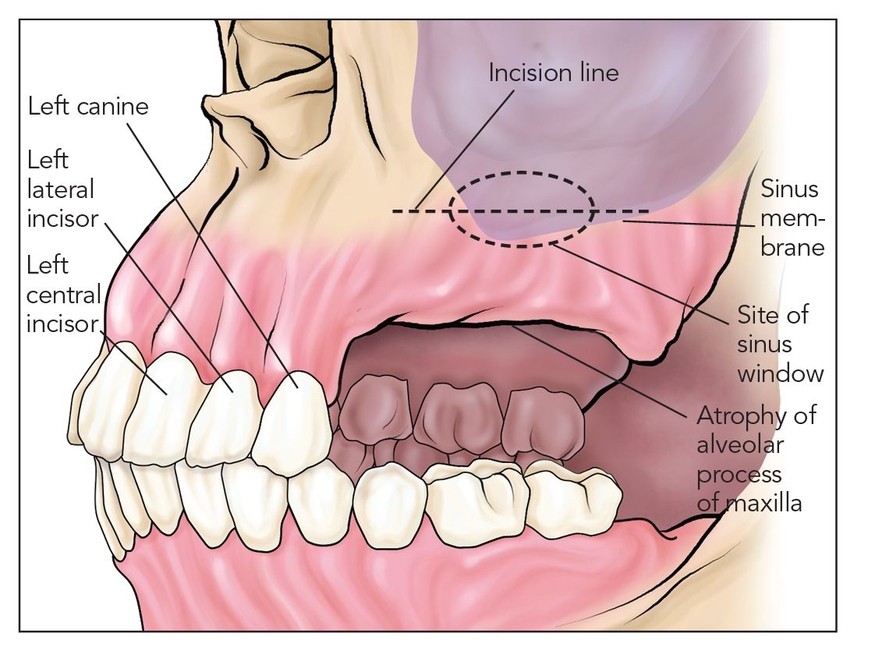
Fig 13-1a A lateral window osteotomy is made for sinus grafting after a vestibular incision is minimally elevated toward the alveolar crest.
The great advantage of the sandwich osteotomy technique is that it provides a relatively stable alveolar crest and a considerable amount of bone mass for osseointegration. 8 Primary wound closure is usually easily obtained because the incision is made in the vestibule for the sandwich graft and palatocrestally for the split graft, sites that are both easily mobilized to obtain closure for modest gaps of 5 mm or less. Because these are vascularized osteoperiosteal flaps, incision sites heal well, and the alveolar reconstruction is less likely to break down.
 Posterior Maxillary Sandwich Osteotomy
Posterior Maxillary Sandwich Osteotomy
Surgical Technique
In the partially dentate individual, it is difficult for the surgeon to obtain access to perform this osteotomy. The surgeon must be able to visualize the posterior lateral maxilla clearly in order to perform a transsinus osteot-omy procedure. If access is limited, the procedure should not be attempted.
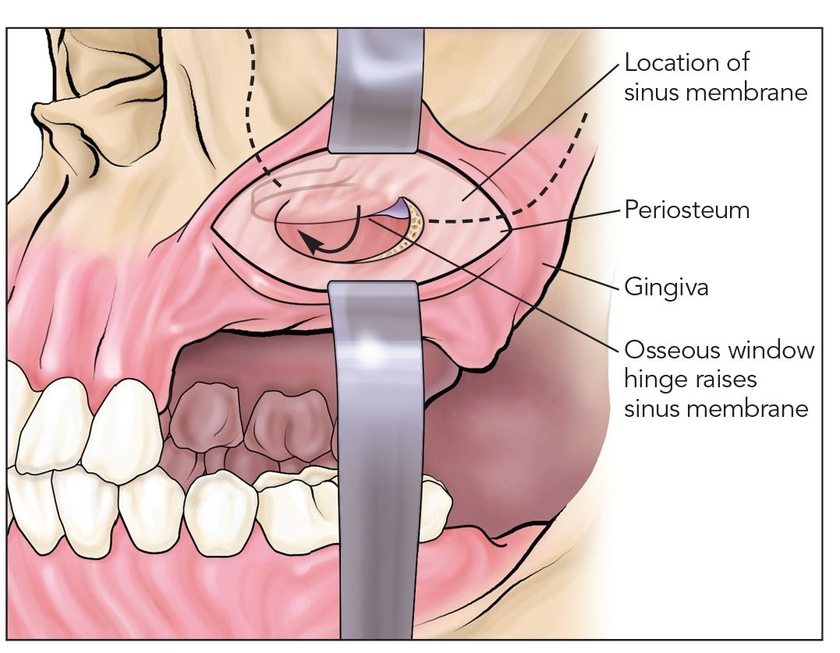
Fig 13-1b Following elevation of the sinus membrane, a lateral horizontal osteotomy is made forward and backward, curving toward the alveolar crest.
The incision is a standard vestibular incision that extends the length of the edentulous space. This procedure is a good choice when both premolars and molars are absent. A much more difficult case arises when only molars are absent, and the value of doing the procedure is one of diminishing returns. After the vestibular incision is made, reflection is minimal crestally but enough to access the lateral maxilla to create a window for elevation of the sinus membrane (Figs 13-1a and 13-1b).
Once the sinus elevation is completed, a horizontal osteotomy cut is made forward and backward, tapering to the alveolar crest (Fig 13-1c). Next, a transsinus downward curving osteotomy is made, connecting at the alveolar crest with laterally made cuts (Fig 13-1d). This palatal osteotomy is done with an oscillating saw or sometimes a piezoelectric knife. If it cannot be completed, an osteotome is used to complete the cut, and the segment is downfractured toward the palate.
The mobilized segment is displaced crestally about 5 mm (Fig 13-1e). To maintain blood supply, no palatal releasing incisions are made (Fig 13-1f). A bone plate is placed to hold the alveolus in a crestally elevated position (Fig 13-1g). If the alveolus deflects significantly palatally, this can be corrected by an alveolar split graft at the time of implant placement, 4 months later (see chapter 7).
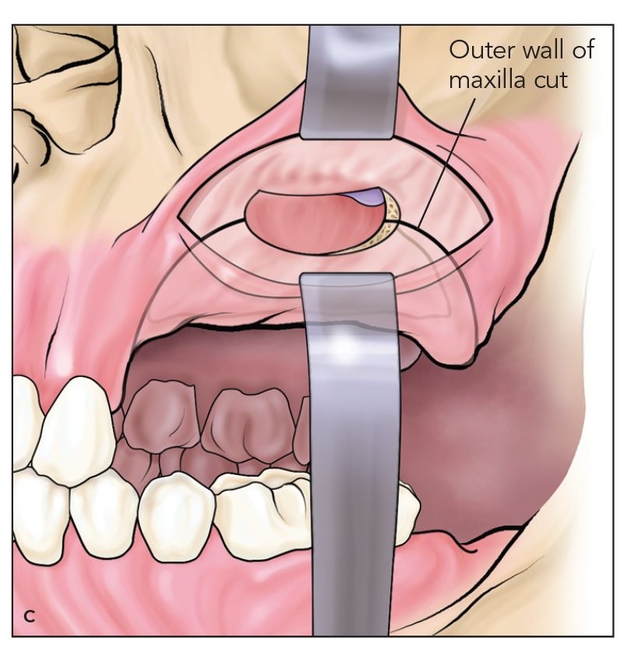
Fig 13-1c A transsinus palatal connecting osteotomy is made, freeing at least a 5-mm (vertical) segment of alveolar bone. An oscillating saw or piezoelectric knife is used in conjunction with spade osteotomes.
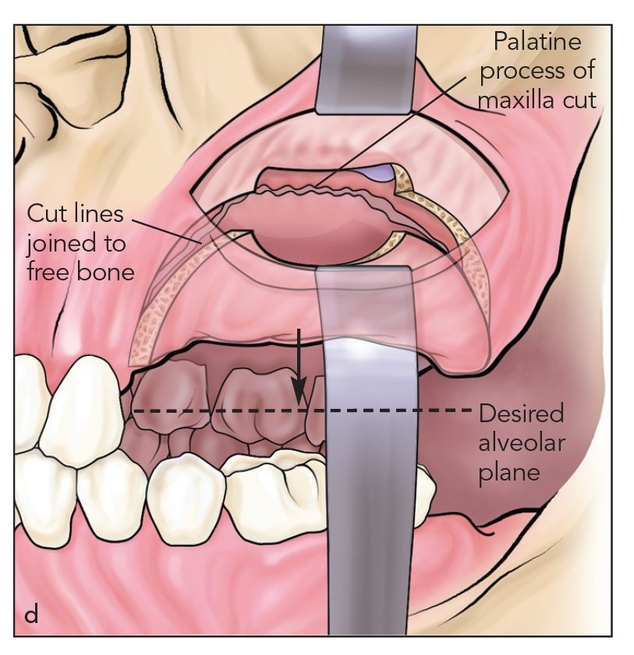
Fig 13-1d The connection at the alveolar crest is made blindly beneath the flap so as not to detach mucoperiosteum from the alveolar segment.
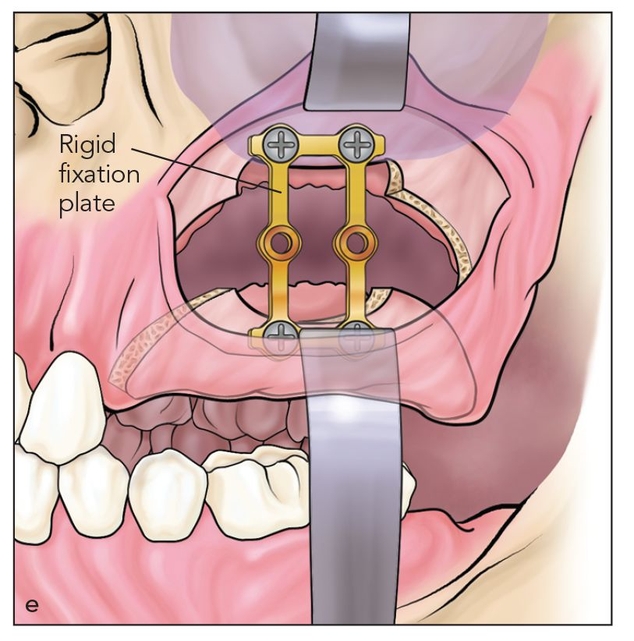
Fig 13-1e Vertical elevation of the segment is usually limited to 5 mm before significant palatal deflection occurs. A bone plate is fixed in place.
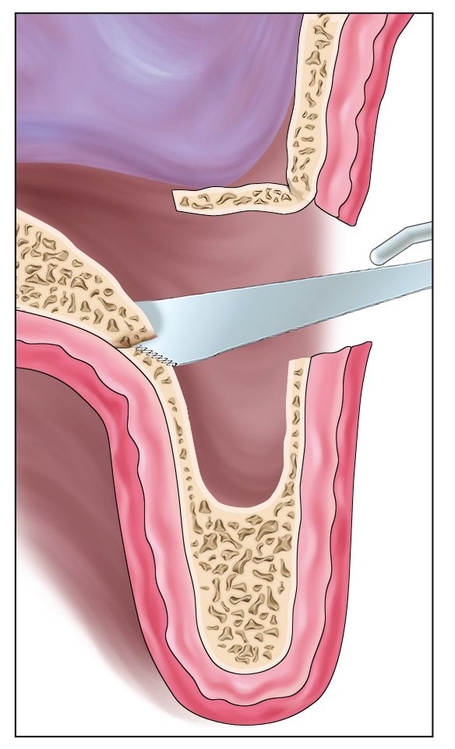
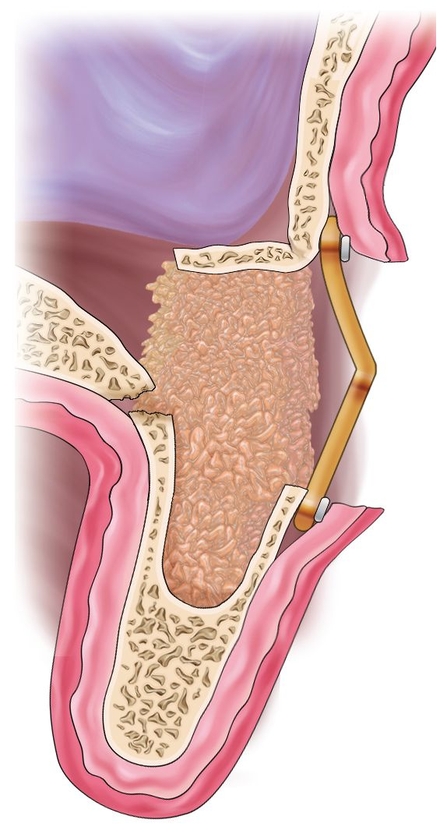
Fig 13-1f A cross-sectional view of sinus elevation from the lateral approach. A transsinus bone cut of the palate tapers to connect with the lateral cut and frees the segment.
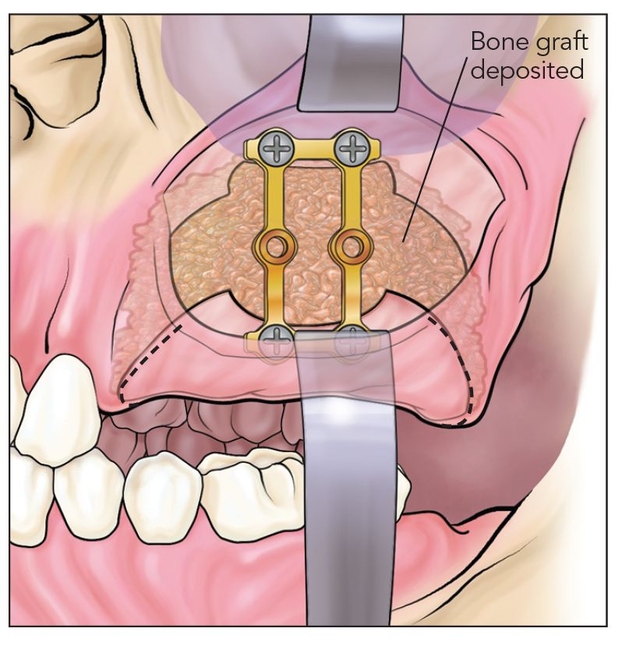
Fig 13-1g The interpositional graft is placed after bone plate fixation. The combination of interpositional and sinus floor grafting has considerable capacity for bone mass expansion.
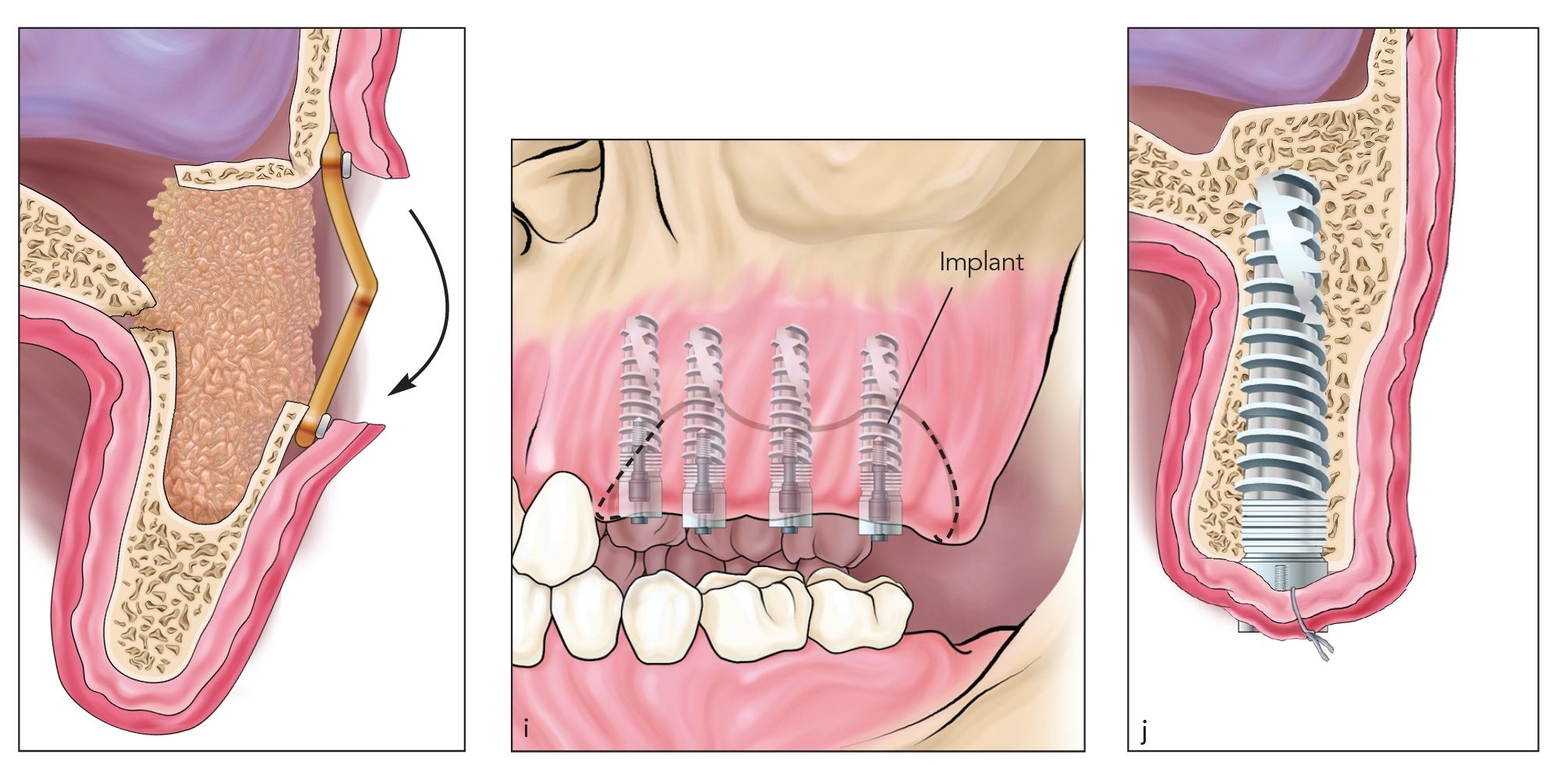
Fig 13-1h Following placement of the bone plate and grafting in the defect, the bone plate is bent (arrow) to torque the alveolus into axial alignment.
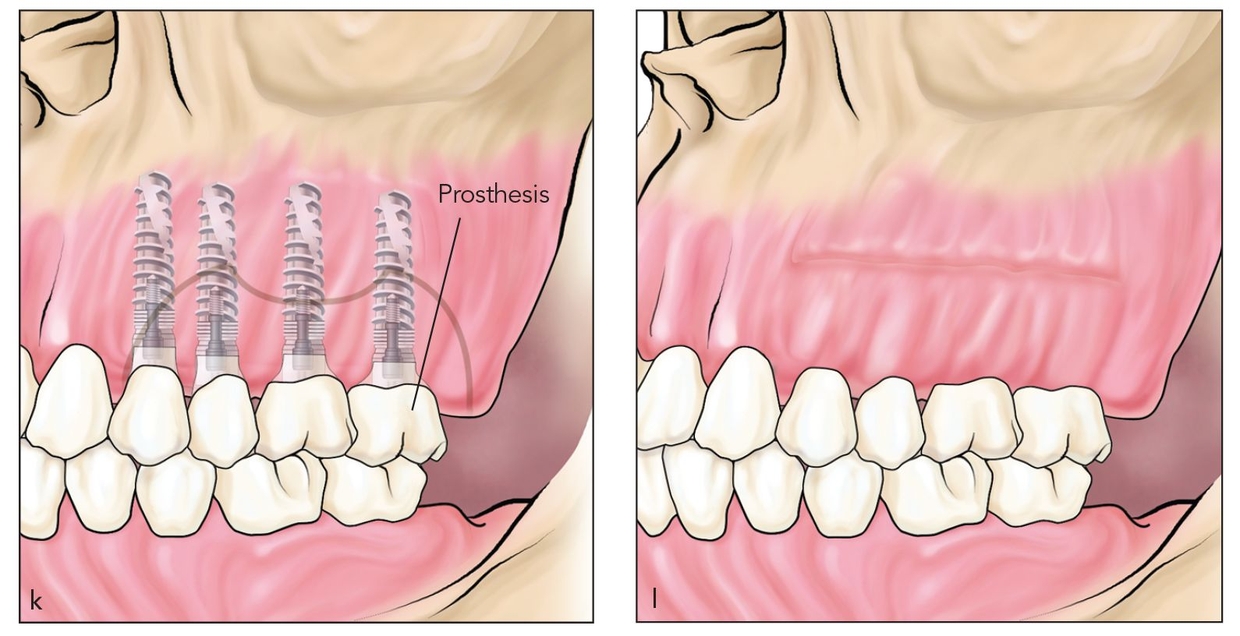
Figs 13-1i to 13-1l Implants are placed 4 to 6 months after grafting, often through an alveolar split approach to normalize alveolar dimension. Final restoration commences 4 months after implant placement.
Following bone plating, the alveolus is torqued toward axial alignment by using a wire twister in a circular crimping action to bend the bone plate (Fig 13-1h). When internal alveolar splitting is used as a strategy to gain width, plate torquing is critical to establishing an axial alveolar position.
Combined with sinus elevation, the osteotomy usually provides 10 to 15 mm of vertical space for bone grafting (Figs 13-1i and 13-1j). This is an excellent setting for the use of rhBMP-2.8 The graft is placed, and the wound is closed primarily in the vestibule.
Following 4 to 6 months of healing, the alveolus is approached from the alveolar crest. If the crest is inclined palatally, an alveolar split bone flap can bring the buccal segment into a lateral position while implants are placed transalveolarly in the sinus graft consolidation (see chapter 8). Final restoration proceeds 4 months after implants are placed (Figs 13-1k and 13-1l).
Case 1: Posterior sandwich osteotomy with sinus floor grafting
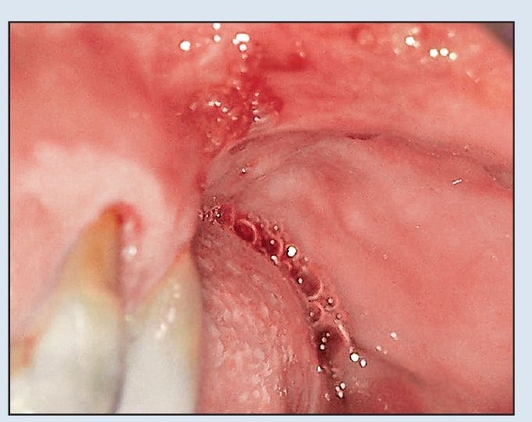
Fig 13-2a A 51-year-old woman is missing her maxillary left molars and has a 12-mm vertical alveolar deficiency.
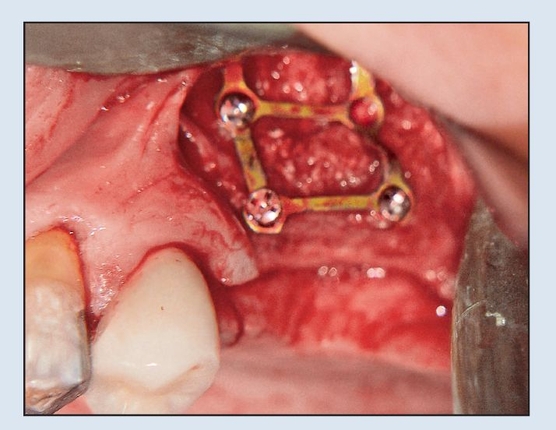
Fig 13-2b A combined sandwich osteotomy and sinus floor graft are used to move the segment downward 5 to 6 mm. The segment is fixed still short of the alveolar plane.
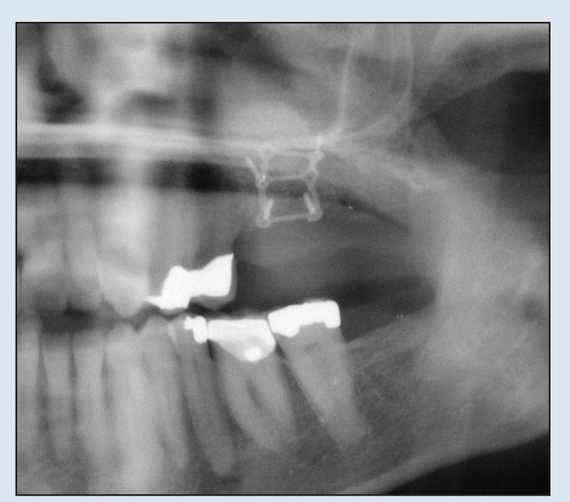
Fig 13-2c The panoramic radiograph reveals good consolidation of the segment 4 months after grafting.
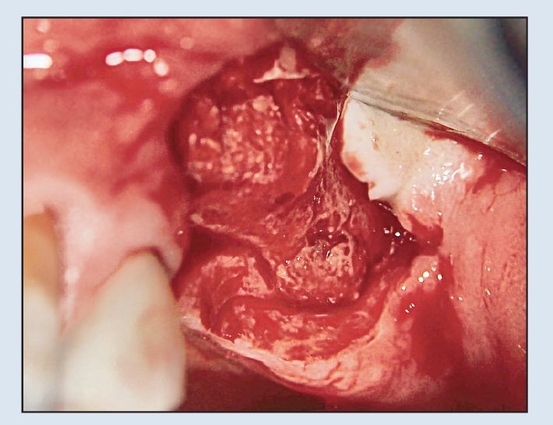
Fig 13-2d The site is approached through a crestal incision, and the titanium bone plate is removed, revealing well-healed bone.

Fig 13-2e Two implants are placed in the healed site, and the final restoration is completed 4 months later.

Fig 13-2f The final radiograph shows a stable bone level.
Case 1: Posterior sandwich osteotomy with sinus floor grafting
A 51-year-old woman was missing her maxillary left molars. A prominent sinus was associated with vertical atrophy of approximately 12 mm (Fig 13-2a).
A vestibular incision with minimal elevation toward the alveolar crest was used to create a lateral antrostomy window for elevation of the sinus membrane. Horizontal osteotomies were made forward and backward, curving toward the alveolar crest. These cuts were connected with a hori/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


