13
Prosthodontics, endodontics, and other restorative care for frail elders
GUIDELINES TO CARE
“Come, grow old with me, the best is yet to be” opines the poet but not the experienced dentist to her or his frail patients. The physiological parameters of old age, which still include functional abilities and remedial potential, are frequently eclipsed by disease. All too suddenly, management strategies based on routine dental treatment formulae are passé and must be replaced by more eclectic and humanitarian care outside our traditional boundaries.
It is one thing to cope with the technical challenges encountered when treating elderly patients, but quite another to manage the oral healthcare of frail elders. The former’s requirements for health maintenance are not dissimilar from those for other age groups. They are variations on the themes of traditional dental ingenuity, albeit with subtle differences in patient management irrespective of whether the clinical initiative involves retention of teeth or their replacement. The needs of all elderly patients vary greatly and should be considered within the context of general health and social circumstances, which change as our patients grow frailer. These flux and uncertainty require mature clinical aptitude and experience together with a high level of interpersonal skills in all aspects of healthcare. As a result, maintenance of oral health for frail elders demands an optimal convergence of realistic concerns and desires from the elders and their caregivers complemented by competent professional skills and judgments.
Frail elders, when managed appropriately, require stronger doses of compassion, common sense, and clinical pragmatism. Their expectations, and often those of their caregivers, of comfort and function are unlikely to warrant “herodontic” interventions or even major aesthetic concerns. Automatic reliance on the sort of “comprehensive treatment” repertoire that includes extensive fixed prostheses and complex implant restorations should be avoided in patients who are systemically brittle and obviously fragile. Frail elders are also unlikely to be managed suitably by dentists whose convictions regarding optimal professional care preclude simpler and less invasive management strategies. There is very little rigorous evidence to support a particular course of treatment for patients who are frail and dependent. Consequently, dentists must rely on personal and borrowed best practices from more robust patients with similar impairments and disabilities. However, the most prudent and sensible perceptions of care must focus on comfort and function without risking additional morbidity.
There are ethical and legal considerations that challenge a dentist’s remit even further when managing the needs of this vulnerable population. Clinical judgments leading to dental treatment need to be made as correctly as possible and, preferably, in consultation with caregivers along with family and friends who have a close and affectionate relationship with the patient. The old maxim “treat the patient as you would if he or she was your own parent” is an admirable humanitarian substitute for the absence of a specific scientific measure for gauging a patient’s adaptive potential. The concept of reconciling normative with realistic treatment needs for frail patients offers a prudent example for managing the oral healthcare needs of patients with, for example, Alzheimer’s disease (Nordenram et al., 1997). It is based on a comparable escalating level of intervention that initially deals with immediate and necessary concerns, such as relief of pain and control of infection (Table 13.1).
Table 13.1 Normative compared with realistic treatment needs for frail elders.
| Normative needs | |
| Patients in this category have stable systemic health and good cognitive function. They also demonstrate a capacity to make independent decisions. | |
| Overall management objectives respond to pain, discomfort, and compromised function in the context of ensuring symptom relief and instituting preventive and corrective measures that maintain oral health, comfort, and aesthetics, as requested by the patient. | |
| 1 | Immediate: |
| Relief of pain and management of oral infections (extractions, endodontic treatment, relief of sore spots related to dentures, etc.) | |
| 2 | None: |
| Pain or disease is not present and oral function is satisfactory | |
| 3 | Minor: |
| Preventive measures to support and maintain oral health modifications | |
| Repairs/modifications/cleaning of prostheses | |
| 4 | Major: |
| Traditional clinical responses to sequelae of caries, periodontal, pulpal, or mucosal diseases by relieving discomfort and preventing bacterial dissemination | |
| Fabrication of new prostheses with consideration for implant support design | |
| Realistic needs | |
| Critical concerns here are the patient’s systemic health and cognitive capacities, as well as the availability and ability of caregivers to provide routine and frequent oral hygiene. | |
| Overall management objectives are the same as those employed in normative needs. However, impaired cognition and/or inability to cooperate will determine the extent of intervention. | |
| 1 | Immediate: |
| Relief of pain and management of oral infections (extractions, relief of sore spots related to dentures, etc.). Interventions are minimal and seek to improve overall function and quality of life. | |
| 2 | None: |
| The patient is uncooperative, but treatment is unnecessary if the patient’s oral environment is judged to be harmless or free of pain. | |
| 3 | Modest: |
| Only palliative care is rendered if the patient is uncooperative, and operative or prosthodontic treatment is likely to compromise the patient’s overall well-being. Even the most minimal interventions might require general anesthesia, which raises a need for more general management decisions with broader medical implications. | |
| 4 | Extensive: |
| The patient wants treatment and is cooperative. The intervention seeks to maintain or improve oral health, and prosthodontic treatment might be feasible. | |
Indeed, this conceptual approach acknowledges “no treatment” as an appropriate management strategy when there is no evidence of pain or risk, and particularly if the patient is uncooperative. Interceptive or corrective treatments, when needed, can be selected from a repertoire of modest protocols to correct and manage oral impairments and disabilities. And finally, there is a wide range of prosthodontic treatments available to meet most expectations of function and comfort.
Other than people with surgical maxillofacial defects, there is probably no other group demanding of so much wisdom, compassion, and clinical skill from dental professionals than the growing population of frail elders. And yet, our knowledge is far from adequate to offer them a defensible “best prosthodontic practice.” Regrettably, there is a prevailing view that technological innovations offer quasi-panaceas that eclipse all other concerns. However, we believe that we have a compellingly professional obligation to balance technical skill with humanitarian priorities and common sense when attending to the needs of this particularly vulnerable population.
This chapter deals with the management of oral healthcare for frail elders under the following headings: dental restorations for individual teeth, endodontic interventions to prolong the life of useful teeth, teeth replacement with fixed or removable prostheses, and recruiting oral implants to optimize prosthodontic prognoses.
DENTAL RESTORATIONS FOR INDIVIDUAL TEETH
Process and product in restorative and operative treatments
Teeth function for frail elders no differently than for other age groups. Whether sound or restored, they affect appearance, mastication, and other functions of the dentition as a whole. And while some teeth are more important than others (Käyser, 1994; Witter et al., 1999), dental restorations in general repair compromised teeth and protect them from further disease and trauma. Decisions to restore teeth for frail patients depend on a balance of input (effort, cost, and risk for unwanted side effects) and outcome (functional effectiveness, durability, comfort, etc.). However, the propensity or willingness of patients to cope with all the inevitable burdens of restorative treatment is often diminished (Mojon and MacEntee, 1994; Ettinger, 1996; MacEntee et al., 1997). For this reason, all operative interventions should be kept to a minimum wherever possible and adapted to the patient’s general expectations and propensities.
In general, the important parameter or defining characteristic of operative dentistry for an able-bodied patient is the clinical product or treatment outcome. Typically, this should be long lasting and of high quality. However, frail patients require a different set of parameters that are physically and psychologically less demanding, relatively less durable, and repeatable at low cost if necessary (Table 13.2).
Table 13.2 Context of restorative treatments for elders who are robust or frail.
| Context | Elders | |
| Robust | Frail | |
| Overall objectives | Restore | Maintain |
| Treatment | ||
| • Range | Unrestricted | Restricted |
| • Burden | Limited | Extensive |
| Adaptability of patient | Good | Moderate to poor |
| Expected longevity of results | >5 years | <5 years |
Direct or indirect restorations
Direct adhesive restorations are the first choice in the treatment of primary caries (Selwitz et al., 2007). However, a large proportion (50%–65%) of restorations made for older patients are replacements, and as the restorations are enlarged, teeth are weakened (Brantley et al., 1995; Mjor et al., 2002; Forss and Widstrom, 2004). Indirect restorations are used to repair posterior teeth with large structural defects (Stavropoulou and Koidis, 2007), but anterior teeth that have been endodontically treated are more likely to be weakened further by metal ceramic or all ceramic crowns because of the amount of enamel and dentine removed to accommodate them (Sorensen and Martinoff, 1984). Nonetheless, there seems to be no significant difference overall in the clinical survival of direct and indirect restorations associated with endodontically treated teeth (Mannocci et al., 2002; Fokkinga et al., 2007, 2008). Indirect cast posts are probably more durable clinically than direct posts of composite resin (Jung et al., 2007), but the difference has little practical relevance to the dental needs of frail elders. Probably of greater relevance is the fact that directly bonded resin composites and amalgam restorations can be repaired effectively with minimal intervention to increase their longevity (Gordan et al., 2006; Moncada et al., 2009).
Cracks can occur in teeth with or without large restorations (Roh and Lee, 2006), and they can be treated with equal success by direct and indirect restorations if the tooth cusps are covered (Signore et al., 2007; Opdam et al., 2008). Finally, there is no compelling evidence favoring routine use of crowns to prevent fracture of teeth (Bader et al., 1996).
Abutment teeth
Abutment teeth for removable prostheses can carry heavy occlusal loads especially in denture-wearers who grind or brux their teeth. Consequently, if they are damaged and structurally weak, they can be crowned with indirect restorations to prevent further damage from stressful loads. However, the effectiveness of this preventive treatment, which seems reasonable, has been tested only for abutment teeth with precision attachments (Vermeulen et al., 1996). Overdenture abutment are subjected also to heavy loads in some patents, but here there is evidence that access to the root canal orifices can be closed effectively for at least 4 years with amalgam, composite, or glass ionomer restorations (Keltjens et al., 1999).
ENDODONTICS
Pulpal and periradicular disease is very common in adults; so is root canal treatment. In Denmark, Taiwan, and the United States, the annual incidence of endodontics lies somewhere between 1% and 7% of the adult population (Kirkevang et al., 2006; Tilashalski et al., 2006; Chen et al., 2007), while the prevalence is approximately 11% of all surviving teeth. Apparently, people accumulate periradicular disease and need root canal treatments as they age, and awareness of this need seems to be increasing (Goodis et al., 2001; Vysniauskaite and Vehkalahti, 2006). Therefore, where endodontic treatment is readily accessible, it is likely that frail elders with natural teeth will have teeth with endodontic restorations.
Underdiagnosis and undertreatment of periradicular pathoses is common, especially in elderly populations (Petersson et al., 1989), although many of the periapical radiolucencies are healing rather than failing lesions. As a result, radiolucencies reflecting healing lesions accumulate as people grow old. Moreover, it is also likely that patients tolerate incompletely healed endodontic treatments without seeking additional intervention. Of course, an endodontic failure with extant pathosis should be addressed by orthograde endodontic retreatment or by extraction of the tooth.
Outcomes of endodontic treatment
Endodontic interventions are very successful with about 97% surviving comfortably for at least 6 years (Torabinejad et al., 2007; Iqbal and Kim, 2008). Failed root canal treatments are best addressed by cleaning and obturating the canals again rather than by surgical endodontics (Torabinejad et al., 2009). Success of on-surgical retreatment increases over time as patients heal, whereas surgical successes appear to decrease steadily over time. Endodontic surgery should be considered very selectively and only when retreatment fails or there is an immovable impediment, such as a post, in the canal of a strategically important tooth. The invasiveness of surgery in contrast to endodontic retreatment is an important consideration for frail patients, and there is little doubt that root canal treatment is inherently less traumatic than extraction of a tooth.
Endodontics as a foundation for prosthodontics
Pulpal and periradicular health should be confirmed before predicting the prognosis of an abutment tooth, and the prognosis of endodontic treatment is based collectively on a patient’s history, the relative response of similar teeth to percussion, palpation, periodontal probing, electrical and thermal stimuli, and on radiographic observations. The absence of a pulpal response to cold, heat, or electrical stimuli does not necessarily mean that the pulp is necrotic. It can indicate also that there is thermal and electrical insulation by secondary or reparative dentin around the root canal––a common finding in old age. The correct interpretation of test results depends on clear communications to and from the patient, although communications can be challenging when patients are deaf, confused, or cognitively impaired.
Root canals calcify with age, which changes the technical difficulty rather than the prognosis of treatment (Goodis et al., 2001). The concept of the “stressed pulp” has been attributed to advancing age, but there is no convincing evidence that it exists in any way to justify “preventive endodontics” or “corrective endodontics.” Endodontic treatment for a patient at any age and in any state of health is justified only if it addresses pulpal and periradicular pathoses diagnosed firmly on the patient’s symptoms and clinical signs.
Medical and patient considerations for endodontics
The key to successful endodontics is removal of sufficient bacteria to allow normal healing, whereas instruments, materials, and techniques appear to be relatively unimportant. Few medical conditions are linked to this success (Quesnell et al., 2005). Healing, especially of periradicular lesions, is compromised in patients with diabetes (Fouad and Burleson, 2003), whereas bleeding disorders, radiation therapy, and high doses of bisphosphonates all favor root canal treatment over dental extractions or other surgical procedures. Indeed, root canal treatment is only precluded by severe and life-threatening illness or if a patient cannot understand and cooperate with the dentist’s directions. And even when cooperation is absent, sedation or general anesthesia can enable the treatment.
Restoring endodontically treated teeth
The risk of vertical fracture in a posterior tooth can be reduced by covering the occlusal surface with a metallic or ceramic crown (Stavropoulou and Koidis, 2007), but anterior teeth with endodontic restorations can be weakened further by the preparation needed to accommodate crowns (Sorensen and Martinoff, 1984). Survival of an endodontically treated tooth depends on the integrity and structure of its crown and of its root (Nagasiri and Chitmongkolsuk, 2005; Fokkinga et al., 2007). A coronoradicular amalgam alloy or resin-composite restoration is a conservative, simple, useful, and inexpensive way to maintain a tooth with an endodontic restoration (Nayyar et al., 1980; Kane et al., 1990). Occasionally, it is necessary to place a post in the root canal to retain and stabilize the coronal restoration, despite the risk of an untreatable vertical root fracture. Currently, there is a lack of long-term evidence to favor fiber over metal posts (Cagidiaco et al., 2008). Fiber posts are relatively flexible, which might reduce the risk of root fracture, but their flexibility could also leave them prone to retentive or structural failure.
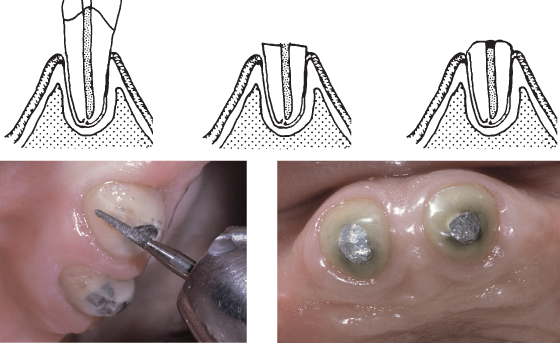
Artificial crowns on endodontic posts are rarely reliable abutments for removable dentures with distal extensions because the stress is likely to dislodge the post and crown. It is much less stressful to seal the root canal above the endodontic filling with an amalgam alloy or resin-composite restoration, and to contour the occlusal surface as a dome protruding approximately 3 mm above the gingiva so that it is easily cleaned when the denture is removed (Figure 13.1).
Figure 13.1 Overdenture abutments with amalgam restorations.
Managing discolored teeth
The appearance of discolored teeth after endodontics can be improved with bonded composite or porcelain veneers supplemented by internal bleaching of dentine. A white or light opaque core of composite material placed deeply within the access cavity to the pulp chamber will improve the color of an abnormally dark tooth. Internal bleaching is safe with an aqueous slurry of sodium perborate without superoxyl or heat if a resin or glass ionomer cement base is placed above the level of the periodontal attachment.
TEETH REPLACEMENT
Prudent prosthodontics for any age group should be driven by reconciling a patient’s needs and desires with a thorough knowledge of health, disease, and the likely outcomes of all treatments. The unavoidable risk of adverse ecological change dictates that treatment should be planned with concern for adverse biomechanical and aesthetic disturbances. The latter can take place in the context of possible time-dependent risks of further changes to the entire oral environment (Zarb et al., 1978). A history of caries and periodontal diseases increases further the challenge of repairing or replacing teeth and associated structures. Physical and cognitive disabilities reduce personal autonomy and the ability to handle and maintain oral prostheses, while compromising the ability and motivation for invasive and lengthy treatments. Muscle coordination and adaptation to dentures appears to decrease as dementia progresses (Taji et al., 2005). Limited finances––real or imagined––occasionally restrict treatment options even further. Nonetheless, preliminary or exploratory treatments can be useful for assessing a patient’s resiliency and ability to cope with a proposed treatment, which, in turn, could lead to further accommodations as frailty and dependency increase (Riesen et al., 2002).
Healthy elders today in many countries see themselves as consumers of healthcare who expect to pay a professional fee for correct and ethical guidance along with the treatment itself. They often expect to participate in developing the treatment plan, and the outcome can be influenced substantially by their commitment to it. Hence, the dentist’s responses to presumed treatment needs, such as “Let’s save all of the remaining teeth and replace the missing ones,” or “We’ll remove the hopeless ones and just wait and see,” are not always readily or uncritically received. On the other hand, explaining the time-dependent ecological implications of any form of provisional, partial, or extensive plan of treatment––and preferably for treatment that is as innocuous as possible––to frail patients and other caregivers demands a particularly prudent and resilient approa/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


