Chapter 13
Imaging of the salivary glands
Introduction
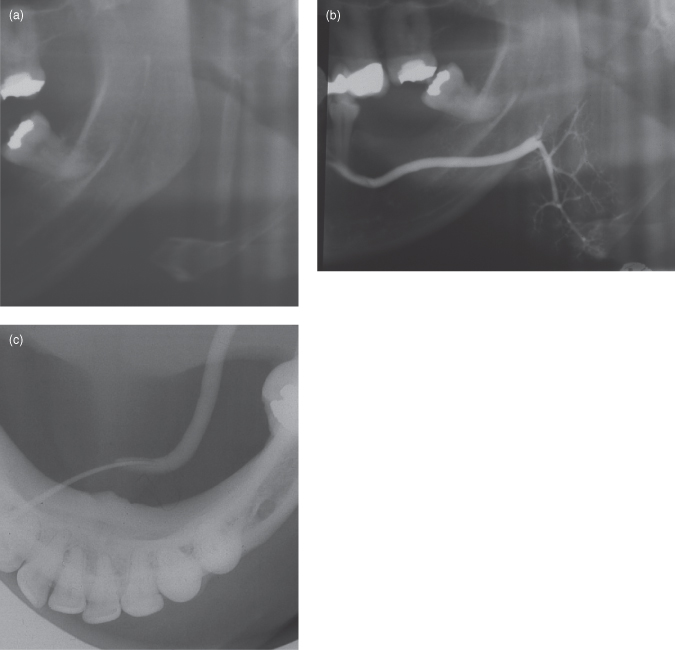
Imaging of the salivary glands includes almost the entire range of imaging modalities, from conventional imaging through computed tomography (CT), magnetic resonance imaging (MRI), ultrasound (US), and positron emission tomography (PET). Figure 13.1 overviews the main glandular lesions and their imaging strategies. The classical imaging technique for salivary gland disease is sialography (Figure 13.2). Although it temporarily slipped into abeyance, it has experienced a renaissance due to its central role in interventional sialography, a therapeutic modality for the conservative (or minimal surgical) treatment of obstructive glandular disease. This conservative treatment can also be achieved under US guidance and may include lithotripsy. The basic principles of US were introduced in introduced in Chapter 8.
Figure 13.1. Overview of the principal glandular lesions and their imaging strategies. PET, positron emission tomography; PSA, pleomorphic salivary adenoma.
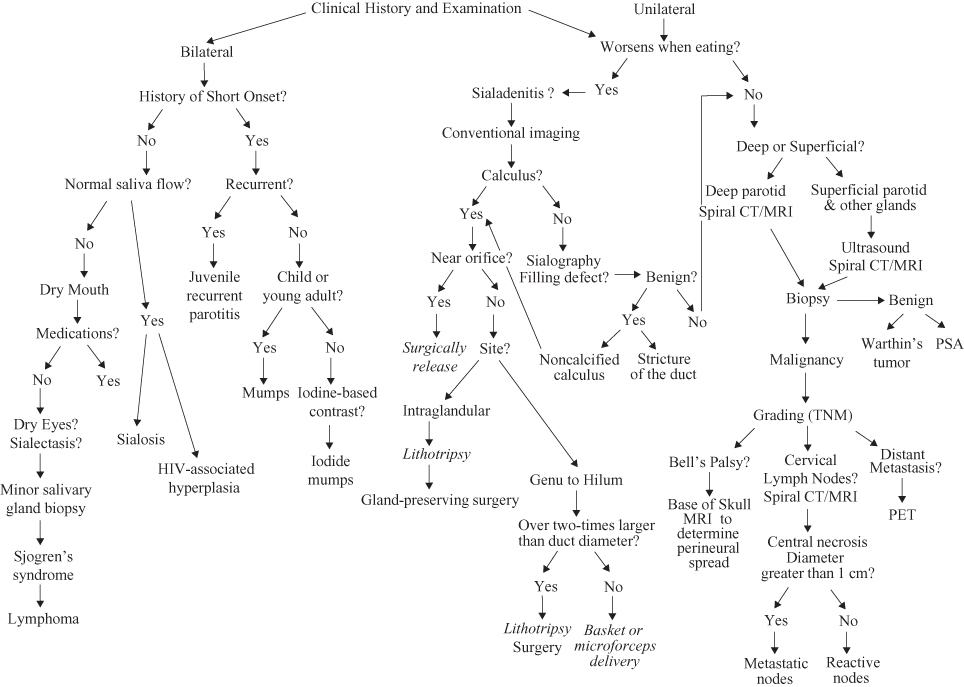
Figure 13.2. Sialography of a normal submandibular gland. (a) Pre-sialogram panoramic radiograph displaying no radiopacities. (b) Panoramic radiograph showing a normal submandibular gland. The “blush” around the terminal ducts represents some overfilling of the acini. The submandibular gland is of uniform width and displays no filling defects. It follows a horizontal route until it reaches the posterior margin of the myohyoid muscle and turns sharply downward to the hilum of the submandibular gland. (c) A true occlusal image displaying the cannula inserted into the submandibular duct through the submandibular papilla.
Diseases affecting salivary glands can affect one or more glands. Affected glands generally appear swollen or enlarged. This may be accompanied by pain, particularly if acute onset, and perhaps an alteration in saliva flow rate. The last is usually reduced. Those arising from obstructive disease or neoplasia most frequently affect one gland, whereas those caused by systemic disease affect more than one and frequently present bilaterally. Although the smaller major salivary glands (submandibular and sublingual) can be affected by the latter it is usually swelling of the larger parotid glands that is most clinically obvious.
Bilateral Swelling
Bilateral swelling of the salivary gland can be of rapid onset or chronic. The most frequent cause for rapid onset of swelling and pain is mumps, whereas the chronic swellings are features of Sjogren’s syndrome and human immunodeficency virus (HIV) infection.
MUMPS
Acute sialadenitis, such as in mumps, are generally readily diagnosed by their classical presentation and so quickly self-resolving that there is little role for radiology, particularly when mumps presents within an epidemic and affects young patients. Nevertheless, presentation in the older patient may require appropriate imaging, such as US. Radiology itself may provoke “iodide mumps,” a rare response to intravenous contrast.
Hitherto, mumps was a significant public health issue prior to the measles, mumps and rubella (MMR) vaccine. As a result incidence of mumps plummeted from the 1960s, only to reemerge recently among adolescents and young adults1 and in many schools and universities in North America and Europe.1–3 The morbidity is very high: cerebrospinal fluid pleocytosis (occurs in 50% of all cases), orchitis (up to 30%), and spontaneous abortion (27%).2 There may not be a single cause; a lack of vaccination, an incomplete vaccination, or a decline efficiency of vaccination have been variously proposed.
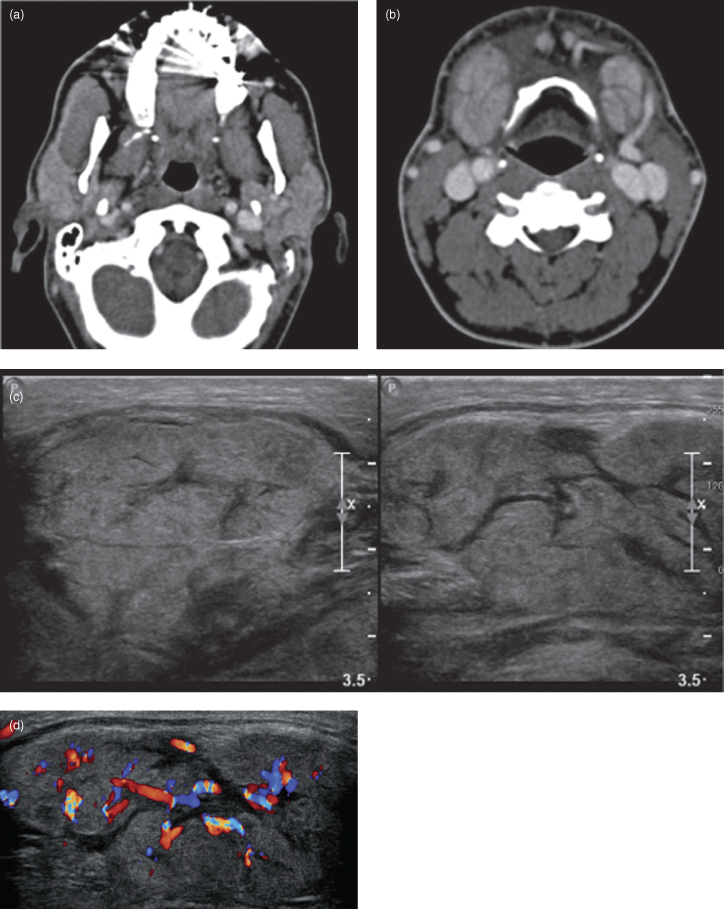
US is generally not indicated, unless the mumps manifests unilaterally. On US, mumps-affected parotid has a rounded shape “with a convex lateral surface and a hypoechogenic structure.”4 Such a case is displayed in Figure 13.3. This case was a middle-aged male, who presented with a rapid onset of bilateral swelling of the submandibular and parotid glands. Early diagnosis and intravenous immunotherapy may minimize complications of mumps.2
Figure 13.3. Adult mumps. (a) Contrast enhanced soft-tissue window axial computed tomograph at the level of the first cervical vertebra. Bilateral swollen parotid glands are displayed. The accessory lobe and the duct of the right parotid gland are displayed. (b) Contrast enhanced soft-tissue window axial computed tomograph at the level of the third cervical vertebra. Bilateral swollen submandibular glands are displayed. The facial vein is observed running on the lateral surface of the left submandibular gland. (c) The grayscale ultrasound displays diffuse almost symmetrical swelling of both submandibular glands. The parenchyma has a diffuse heterogeneous hypoechoic presentation, which is consistent with an acute sialadenitis. There are no hyperechoic foci suggestive of sepsis. (d) Color Doppler ultrasound reveals hyperemia, which is consistent with acute sialadenitis. Figures courtesy Dr. Eli Whitney; Oral Medicine, Faculty of Dentistry, UBC.
HIV-ASSOCIATED SALIVARY GLAND DISEASE
Although all salivary glands are affected by HIV, the parotid glands are most affected due to their inclusion of lymphoid tissue. Three types of lesions may be encountered: inflammatory reaction to the virus, lymphomas, and infection.5
The inflammatory reaction is expressed by benign lymphoepithelial lesions and AIDS-related cysts. The benign lymphoepithelial lesions appear on CT, MRI, and US as dilated cystic ducts within hyperplastic lymphoid tissue. They frequently cause the painless swellings of the parotid. This may be bilateral in up to a fifth of cases. On the other hand AIDS-related cysts appear on the above modalities as multiple lesions, which are bilateral in 80% of cases. These benign lesions are generally not treated and may regress spontaneously.5
Primary salivary gland lymphomas can occur in any gland and present as a painless mass. Severe infections of the salivary gland can occur. Lymph node hyperplasia affects half of the patients. The posterior cervical nodes are most frequently affected. Needle biopsy in addition to imaging is often required to determine whether the node is reactive, infected or neoplastic. The last may represent Karposi’s sarcoma, Hodgkin’s lymphoma, and non–Hodgkin’s lymphoma.5
SIALOSIS
Sialosis is a noninflammatory nonneoplastic phenomenon, which manifests as recurrent painless, usually bilateral, swelling, principally of the parotid glands. US displays hyperechoic parotid glands. Sialosis is associated with endocrine and deficiency diseases. It also is associated with alcoholism, malnutrition, and cirrhosis.
SJOGREN’S SYNDROME
The 5-step American-European classification criteria for Sjogren’s syndrome is set out and discussed by Ellis.6 Three-quarters of cases are in females in the fourth to seventh decades. The parotid is affected in 90%. Although bilateral disease is typical, one side may be more severely affected. The recurring progressive swelling can be accompanied occasionally by discomfort or even pain. Although the lobar architecture is preserved, the progressive parenchymal damage eventually results in the typical sialectasis obvious on sialography (Figure 13.4). it should be noted that sialectasis is not pathognomonic for Sjogren’s syndrome because it can be secondary to infection of the salivary glands.
Figure 13.4. Panoramic radiographs exhibit sialectasis secondary to Sjogren’s syndrome. (a) The sialographic image displaying irregular ducts and sialectasis or dilations within the substance of the parotid gland. There is a constriction of the main duct distal to the ducts for the accessory parotid lobe. (b) The emptying film (the cannula is removed) demonstrates no emptying, meaning that the constrictions of the main are preventing drainage. The emptying film demonstrates that there is also a constriction close to the parotid papilla.
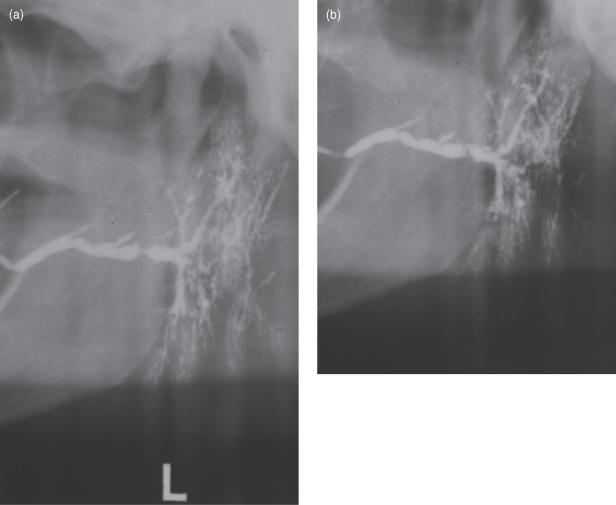
Poul et al. reported that high spatial resolution US is more sensitive than sialography for the investigation of Sjogren’s syndrome. Furthermore, they reported that accuracy is increased when US is carried out in conjunction with sialography.7
Although neoplasms of the salivary glands have long been displayed by MRI; (see also Kinoshita et al.’s pictorial essay8), preliminary work by a Japanese team presents MRI sialography as an alternative to conventional sialography. They compared normal and Sjögren’s syndrome patients9 with stimulated10 and unstimulated salivary flow.11
Bacterial Sialadenitis
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


