Part 1: Introduction
Chapter 1
Basics of radiological diagnosis
Introduction
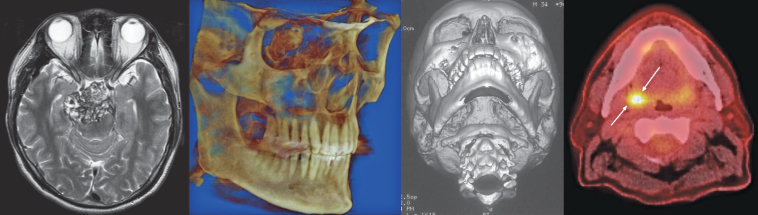
The clinician should understand how the image is made and the normal anatomy and its variants in order to be able to identify artifacts, particularly those that can mimic the appearance of disease. Although these elements, as they present on conventional radiography, are addressed in detail by the wide range of dental radiology texts currently available, this textbook’s figure legends note features caused by incorrect panoramic technique, artifacts, and variations of normal radiographic anatomy. Figure 1.1 outlines the main attributes of the imaging modalities that are featured in this textbook. These imaging modalities have been broadly divided into conventional radiography and advanced imaging.
Figure 1.1. The modalities used in oral and maxillofacial radiology. This is an overview of the main imaging modalities, including remarks concerning their clearest clinical uses, relative advantages over other modalities, and limitations of use.
Diagnosis in oral and maxillofacial radiology is most frequently based both on the clinical findings (including presenting complaint and history) and on the features observed on conventional radiographs. A definitive diagnosis is possible for a large proportion of lesion types that present to the primary care dentist. These lesions do not include just those lesions of inflammatory origin that present as periapical radiolucencies (on histological examination: granuloma, periapical cyst, or periapical abscess) and condensing osteitis, but also dentigerous cysts and dense bone island (also known as idiopathic osteosclerosis). They are not only the most frequently occurring lesions affecting the jaws, but a majority of them also have distinctive clinical and radiological presentations. Some other lesions such as florid osseous dysplasia, the cementoblastoma, the compound odontoma, and some cases of odontogenic myxoma can be definitively diagnosed solely on their radiological appearance. In those situations where a definitive diagnosis is not possible, a differential diagnosis should be developed. This will consist of two or more lesions. Such cases are frequently referred to a specialist as much for a diagnosis as for treatment. In order to assist the reader in his/her diagnosis this textbook is illustrated throughout with diagnostic flowcharts.
There is an expectation that the images created should adequately display the area of clinical interest with the purpose of addressing those clinical questions that indicated the need for the investigations. Thus the image or images should display the entire area of pathology and be free of artifacts. Therefore, an unerupted third molar should not only include the entire tooth and its follicle, but also at least a clear margin of 1 mm around them. This would allow the clinician to determine whether it is close to the mandibular canal or any other adjacent structure.
An example of inadequacy of the radiography resulted in a Canadian dental malpractice case that continued for 12 years through at least five courts before it was concluded, presumably settled.1 The only positive result of this failure to include only 98% of a third molar was its not insignificant contribution to Canadian law specifically and common law in general. From reading the case it is abundantly clear that if an adequate radiograph or radiographs had been taken in the first instance this case would have had little grounds upon which to proceed, and the spilling of so much legal ink and personal and professional distress would have been avoided.
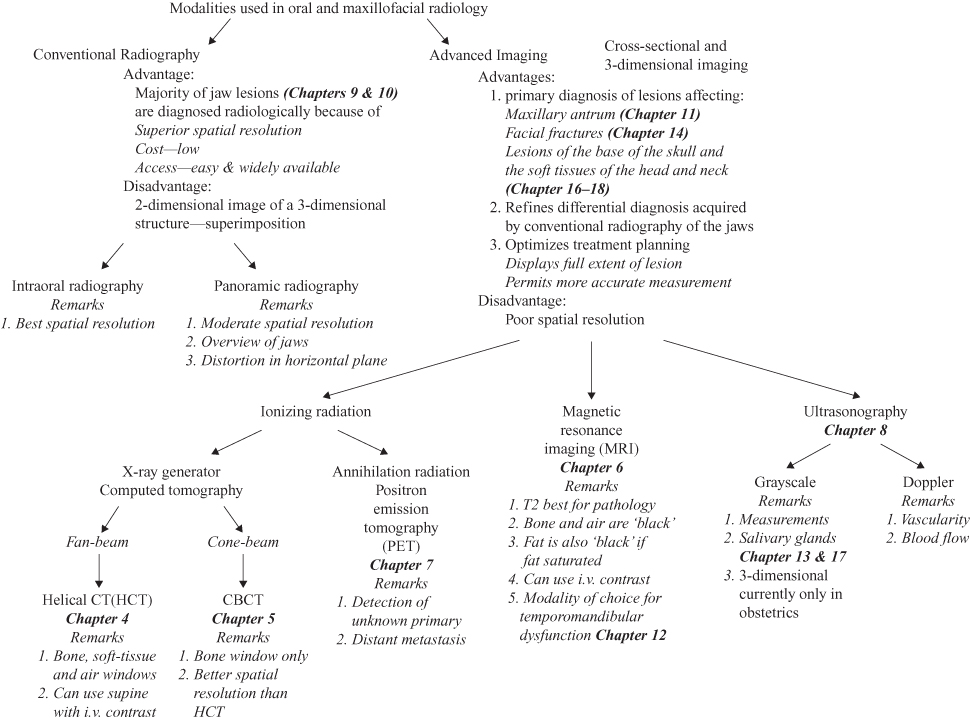
Radiographs are prescribed for three reasons, diagnosis, presurgical planning and follow-up. Those prescribed for the purpose of diagnosis and/or presurgical planning should be made prior to biopsy because this can change the radiology of the lesion appreciably. This is particularly so with regard to advanced imaging such as helical computed tomography (HCT) and magnetic resonance imaging (MRI). Two cases demonstrate the effects of biopsy prior to HCT.
The biopsy of an odontogenic myxoma, a locally invasive benign neoplasm, prior to HCT, provoked an inflammatory response within the depth of the lesion, which was enhanced by the intravenous contrast (Figure 1.2). Contrast is recommended for lesions, which include a neoplasm or a vascular lesion in their differential diagnosis. This, with regard to neoplasms, is important to determine local invasion of adjacent soft tissues, which would need to be resected along with the rest of the neoplasm.
Figure 1.2. A computed tomograph of an odontogenic myxoma carried out after the lesion had been biopsied. The biopsy site still has its dressing in place (Figure 1.2a and 1.2b). As a result there was enhancement (Figure 1.2c) by the intravenous contrast at the site biopsied that is more likely to reflect hyperemia in response to the trauma of surgery. Note: All the major blood vessels including the facial and lingual arteries are enhanced in Figure 1.2c.
Figure 1.2c reprinted with permission from MacDonald-Jankowski DS, Yeung R, Li TK, Lee KM. Computed tomography of odontogenic myxoma. Clinical Radiology 2004;59:281–287.
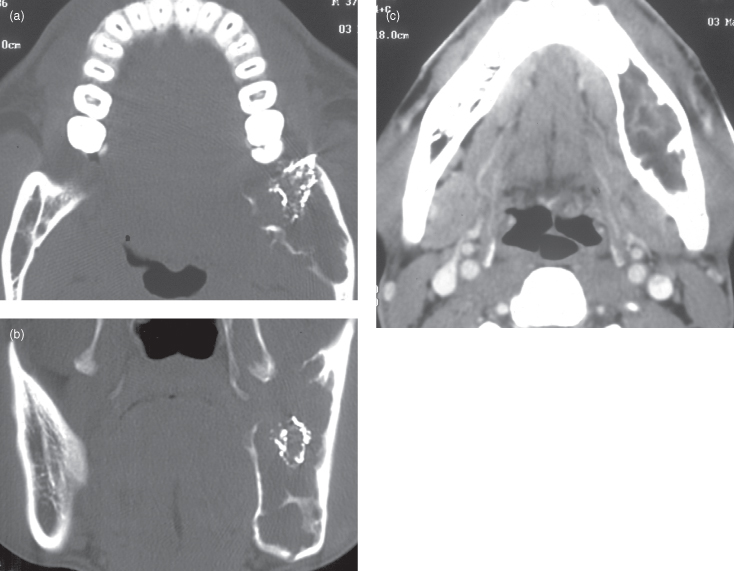
Figure 1.3 displays a case of fibrous dysplasia, which caused a substantial expansion of the affected mandible. When it was first seen by general surgeons unfamiliar with its manifestation in the jaws they performed multiple biopsies. These biopsies created their own artifacts on a subsequent HCT. These artifacts were loss of cortex and dysplastic tissue exuding through a biopsy site.
Figure 1.3. This is a bone-window axial computed tomography of fibrous dysplasia affecting the vertical ramus of the mandible. The cortical defects are the result of several biopsies performed prior to referral for computed tomography. Such operations can largely invalidate any clinically important radiological findings because these, if erroneous, could lead to a wrong diagnosis and inappropriate treatment. Note: Radiology is very central to the diagnosis of specific fibro-osseous lesions, discussed later.

Conventional radiography will be the first imaging modality to be prescribed to investigate further a lesion occurring within the bony jaws obvious to or suspected by the clinical history and/or examination. For the majority of lesions affecting the jaws, conventional radiography is likely to be the sole imaging modality deemed clinically necessary. The principal advantages of conventional radiography are its superior spatial resolution (especially of the intraoral technologies), low radiation dose, and low cost. It is also available in the dental office or surgery. It is most likely that this prescription will include a panoramic radiograph that may be accompanied by intraoral radiographs. These images may be in either analogue (film) or digital format. An overview of the various conventional radiographic technologies is set out in Table 2.1. The panoramic radiograph permits an overview of the jaws from condyle to condyle. It also permits comparison between sides. These premises can be valid only if the patient is properly positioned within the panoramic radiographic unit exposed by the most appropriate exposure factors and the image is properly developed. Finally it is also expected that the resultant image is properly reviewed (read) under optimal viewing conditions (see Chapter 2). To reiterate, all prescriptions for a radiological investigation must be based upon a thorough clinical examination. Although there is little, if no, place for routine radiographic screening in the modern practice of dentistry, every image should be carefully reviewed to identify any pathology that may be incidental to the patient’s complaint and the results of the clinical examination.
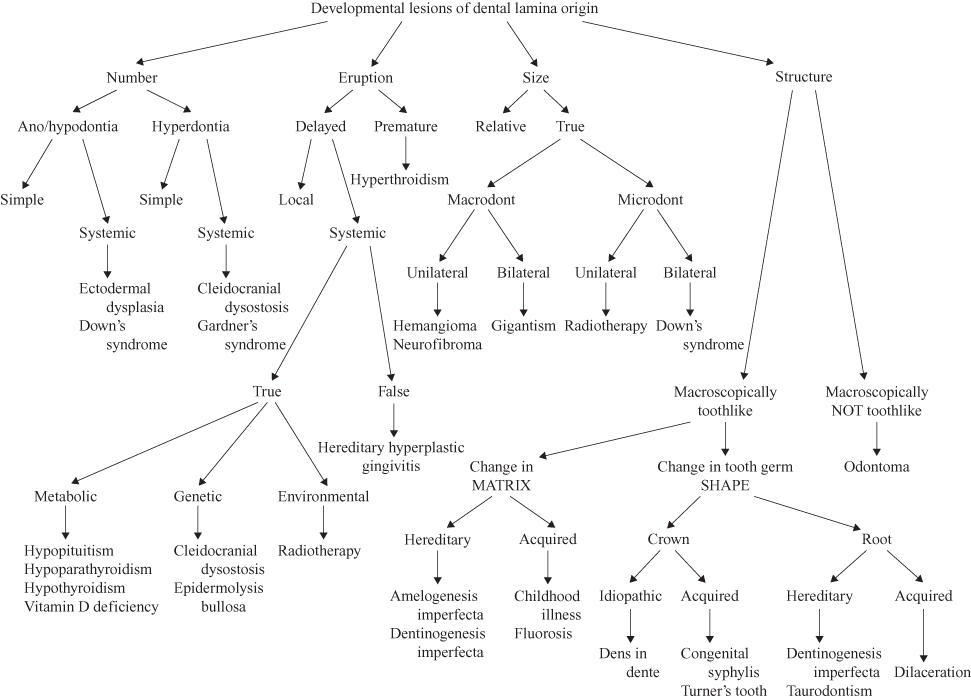
The panoramic radiograph in addition to permitting determination of the specific features of the lesion or suspected lesion that prompted its making, can also reveal macroscopic abnormalities such as size differences and changes in a specific anatomical location (Figure 1.4) Furthermore, it can compliment the clinical examination by confirming defects in the dental development, such as the number, eruption, size, and even structure of the teeth (Figure 1.5). Because these features have been fully addressed in other texts and are generally well understood, space constraints preclude offering images of them here.
Figure 1.4. Classification of macroscopic abnormalities.
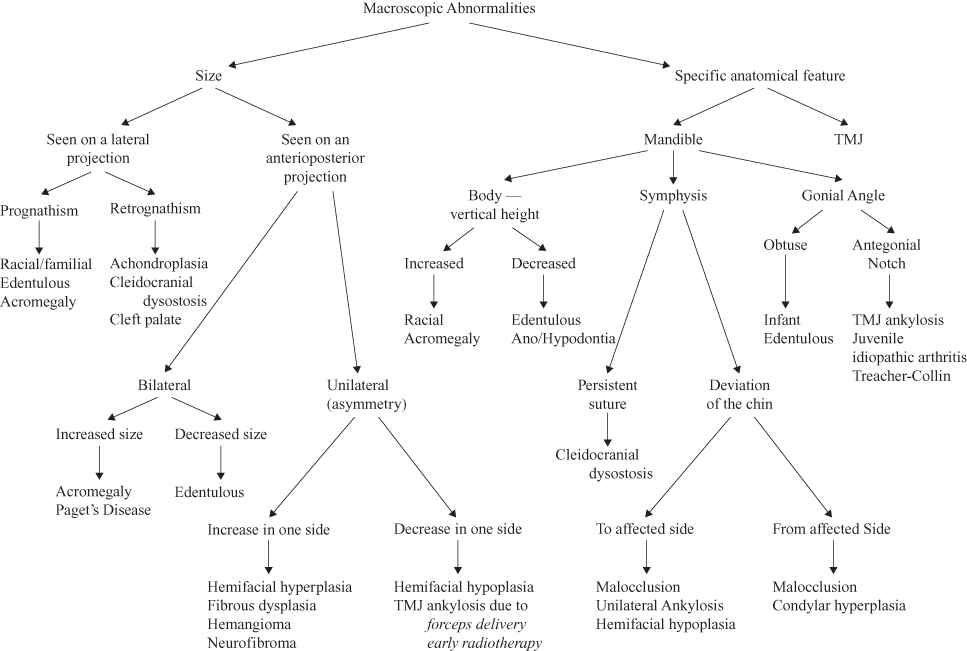
Figure 1.5. Classification of developmental lesions of dental lamina origin.
The various lesions, occurring within the face and jaws, often present with similar features at certain stages. Most will at some stage present as a radiolucency as they create space for further growth within the bony jaws. The borders of this radiolucency give a further clue as to their intrinsic behavior. Encapsulated benign neoplasms and many uninfected cysts grow at a moderate pace and are generally well defined. They may even have a cortex. Infected lesions and malignancies are generally associated by a poorly defined margin reflecting their more aggressive infiltrative expansion into previously normal bone. Sometimes, if the infected lesion becomes less virulent the adjacent bone may respond by laying down more bone on the trabeculae resulting in sclerosis.
Slow-growing lesions, such as most cysts and encapsulated neoplasms, can displace teeth and adjacent structures such as the mandibular canal and cortices. More aggressive lesions are more likely to resorb them. Some malignancies, such as a squamous cell carcinoma, will destroy structures with very little displacement, whereas others will provoke a periosteal reaction such as the onion layer typical of osteogenic sarcoma or Ewing’s tumor. Such periosteal reaction can occur in chronic osteomyelitis. Such periosteal reactions are frequently seen in the extragnathic skeleton2 but are infrequently seen in the jaws.
After the lesion has been properly imaged and reviewed the clinician reaches the point at which s/he wants to identify the lesion. Because the aim at this stage is to achieve, if possible, a definitive diagnosis it follows that this is best accomplished if the images of the lesion have been scrupulously reviewed. To this end I developed the rule of the “Five S’s” (shade, shape, site, size, and surroundings) and its ancillary “Three D’s” (diameter, density, and displacement. There are many lesions that can be definitively diagnosed at this stage, but many others require further investigations, which could include advanced imaging.
In order to ensure that the most appropriate investigations are applied, the provisional diagnosis should be restricted to no more than 3 lesions if possible, placing the most likely in the first position so the most appropriate investigation can be performed to determine whether it is that lesion. An important exception to this “most likely” rule is potential seriousness of outcome of the lesions. Table 1.1 compares clinical outcomes according to a 10-step (0 through 9) hierarchy of seriousness of outcomes. The higher placed lesions have the more serious outcomes.
Table 1.1. Scale of severity of outcomes/potential severity of outcomes of oral maxillofacial radiology*
|
9. Resection, but high likelihood of recurrence or metastasis Poorly differentiated squamous cell carcinoma 8. Resection and lower likelihood of recurrence or metastasis Well-differentiated squamous cell carcinoma (qualified by site) 7. Resection and likelihood of recurrence or metastasis rare Solid ameloblastoma 6. Enucleation and cytotoxic treatment (Carnoy’s solution) Unicystic ameloblastoma (provided not affecting posterior maxilla) 5. Simple enucleation and high chance of recurrence (recurrence rate of 10% and over) Aneurysmal bone cyst (ABC) 4. Simple enucleation and little chance of recurrence Adenomatoid odontogenic tumor (AOT) 3. Simple enucleation and no chance of recurrence (in a neoplastic fashion) Periapical radiolucencies of inflammatory origin (either nonresponsive to orthograde endodontics or too large) 2. Conservative surgery may be required only to improve aesthetics Fibrous dysplasia (surgery is not indicated unless compelled by appalling aesthetics or risk of blindness) 1. No treatment generally required Linqual bone defect |
*This table was inspired by the Richter scale for earthquakes. The scale is based on the general current treatment paradigms for each lesion.
The selection of the lesions can vary among clinicians depending upon that particular lesion’s presentation and frequency within a particular clinician’s patient pool. The age, gender, and ethnic origin of the particular patient and site of predilection are perhaps overemphasized in most teaching programs. The main problem with this is that many lesions frequently present first outside their expected age ranges. Occasionally, this expected age range may simply be out of date. An example is fibrous dysplasia; the majority in a recent systematic review first presented in the third decade and older. If the predilection of a lesion is less than 80% for a particular feature, its value as a major diagnostic tool should be discounted unless it may hint at a serious lesion that should not be overlooked or inappropriately treated. One such lesion is the ameloblastoma, the most common odontogenic neoplasm globally. This 80% limit is reflected in the receiver operating characteristics’ (ROC) area under the curve (AOC).3
Another source for inaccuracy is that lesions are often superficially reported as relative period prevalence (RPP), which is not only dependent upon their proportion but on that of the other lesions within the same group of lesions, such as odontogenic neoplasms. The RPP not only varies between communities,4 but it is also dependent upon the edition of the World Health Organization (WHO) classification of odontogenic neoplasms used. Many previously classified odontogenic neoplasms are no longer formally considered as such. An example is the cementifying fibroma (then later combined with the “ossifying fibroma”, previously considered to be a separate lesion, as the cemento-ossifying fibroma), once considered by the 1971 WHO edition5 to be an odontogenic neoplasm is now considered to be a wholly osseous neoplasm, the ossifying fibroma. Some other lesions are reclassified as neoplasms. The parakeratotic variant of the odontogenic keratocyst is now, according to the 2005 WHO edition,6 keratocystic odontogenic tumor, a neoplasm and thus no longer a cyst, whereas the orthokeratotic variant remains a cyst, the orthokeratinized odontogenic cyst. The same has also happened to the calcifying odontogenic cyst, which is now according to the 2005 edition the calcifying cystic odontogenic tumor. Such changes render RPP increasingly unreliable.
After a diagnosis has been made the clinician has a choice of three broad approaches to the lesion’s management. These have been summarized in the rule of the 3 R’s. Refer (to an appropriate colleague) and review are obvious, whereas recipe (treatment) requires an explanation. This is derived from the apothecary’s “barred R,” now often reduced to Rx derived from the Latin imperative Recipe! meaning Take! or Receive! This is still printed at the top-left corner of prescriptions for pharmaceuticals and/or other treatment.
The nomenclature used throughout will be, as far as possible, that used by the 2005 edition of the World Health Organization Classification of Tumours.6 Common synonyms will appear in parentheses with the first appearance of each term in each chapter. As far as possible the morphology code of the international classification of diseases for oncology (ICD-O) will be provided along with the invaluable behavior codes (“/0” for benign; “/3” for malignant, and “/2” for uncertain). Although, the vast majority of lesions are diagnosed and treated in oral and dental practice solely on clinical and radiological criteria, the overwhelming majority of such lesions are sequelae of dental caries. There are many other lesions, such as cysts and neoplasms, in which a definitive diagnosis based on their histopathology is necessary.
Radiological Features
The radiological features central to the diagnosis of oral and maxillofacial lesions are encapsulated as the Five S’s and Three D’s rules. Although the use of these rules is most apposite for conventional radiography, they can also be applied when viewing HCT’s “bone-windows” (Chapter 4) or cone-beam computed tomographic (CBCT) images (Chapter 5).
SHADE
Shade reflects the radiodensity of the lesion or feature under consideration and is its most obvious radiological attribute. This is readily reflected in the greatest frequency of radiodensity referred to in reports.
The radiodensity of a lesion observed by conventional radiography is usually described as one of three manifestations, radiolucency, radiopaque, and mixed. The radiolucency appears black and represents an absence of the bone type normal for that site (Figure 1.6).
Figure 1.6. A panoramic radiograph displaying a well-defined unilocular radiolucency within the mandible extending from the right first molar’s distal root to the junction between the contralateral canine and first premolar. The right lower border of the mandible has been eroded and displaced downward. The root of the right first premolar has been displaced distally. The root of the second premolar displays resorption. This is a unicystic ameloblastoma. Note 1: This panoramic radiograph had not been made using the optimal technique. It is in the head-down position. Note 2: The apparent root resorption or shortening of the teeth in the anterior sextant is most likely to be an artifact; due to its appearing outside the focal trough of the panoramic radiography. This happens particularly in the anterior sextant. Note 3: The horizontal band superimposed upon the roots of the right molars is the secondary image of the contralateral lower border of the mandible.
Reprinted with permission from MacDonald-Jankowski DS, Yeung R, Lee KM, Li TK. Ameloblastoma in the Hong Kong Chinese. Part 2: systematic review and radiological presentation. Dentomaxillofacial Radiology 2004;33:141–151.
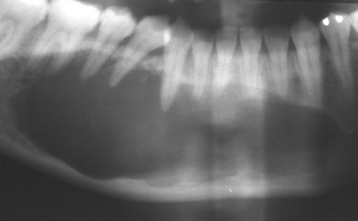
The radiopacity appears white and represents an excess of mineralized tissue—frequently abnormal mineralized tissue (Figure 1.7). This abnormal tissue is usually laid down by cells (almost invariably abnormal bone cells and their variants) due to dysplastic or neoplastic processes and may show some sort of structure. It is not always possible to determine the process by histopathology; three very different lesions, fibrous dysplasia (Figure 1.7), ossifying fibroma (Figure 1.8), and osseous dysplasia (formerly known as cemento-osseous dysplasia) (Figure 1.9) are entirely different lesions but display similar histopathological appearances, those of fibro-osseous lesions. This is discussed in detail in Chapter 10. Sometimes the bone is not per se abnormal but merely thickened trabeculae as found for idiopathic osteosclerosis (also known as dense bone islands) (Figure 1.10).
Figure 1.7. A panoramic radiograph displaying a generalized radiopacity of the posterior sextant. The mandibular canal has been reduced in thickness and displaced to the lower border of the mandible. Two unerupted molars are embedded within the vertical ramus. The lesion has expanded the body of the mandible vertically. This is fibrous dysplasia. Note 1: The mandibular canal is very obvious here as a radiolucent structure set against a background of abnormal (in this case dysplastic) bone. It has not only been displaced downward in this case, but also reduced in diameter and with a slightly irregular course. Note 2: The radiolucent presentation of the maxillary alveolus is a result of the superimposition of the air-filled oral cavity upon it. It may be prevented by instructing the patient to raise the tip of his/her tongue to contact the hard palate. Note 3: The secondary image of the contralateral mandible is superimposed upon the upper two-thirds of the vertical ramus. Note 4: The soft-tissue images of the soft palate and dorsum of the tongue are superimposed upon the upper third of the vertical ramus. The air space of the residual oral cavity between them presents as a radiolucent line, which has been mistaken to represent a fracture of the vertical ramus in other cases.
Reprinted with permission from MacDonald-Jankowski DS. Fibrous dysplasia in the jaws of a Hong Kong population: radiographic presentation and systematic review. Dentomaxillofacial Radiology 1999;28:195–202.
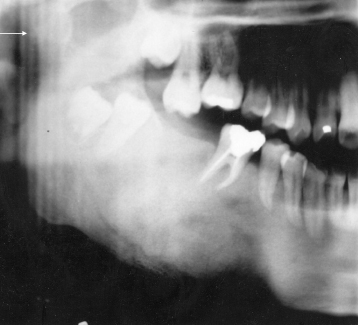
Figure 1.8. Panoramic radiograph displaying an ossifying fibroma. The lesion is well defined. It has a capsule of varying thickness. It has displaced downward the lower border of the mandible and displaced upward the alveolar crest. It has also displaced the mandibular canal toward the lower border of the mandible. It has displaced the root of the premolar forward and the roots of the molar distally. Its central radiodensity has a cotton wool pattern. Note 1: The partial superimposition of the hyoid bone on the lower border of the mandible is an indicator that the exposure had been made in the chin-down position. Note 2: The soft tissue of the gingival mucosa is observed in the edentulous space.
Reprinted with permission from MacDonald–Jankowski DS. Cemento-ossifying fibromas in the jaws of the Hong Kong Chinese. Dentomaxillofacial Radiology 1998;27:298–304.
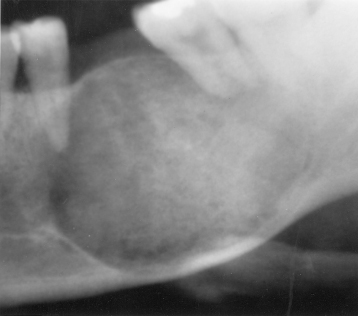
Figure 1.9. The panoramic radiograph exhibits radiopacities in all four posterior sextants. The mandibular lesions are confined to the alveolar process; that is, they are found above the mandibular canal, which can be seen in places. This is a case of florid osseous dysplasia. Note: The relative radiolucency of the anterior sextant of the maxilla is due to the superimposition of the residual oral cavity.

Figure 1.10. This is a panoramic radiograph displaying a well-defined radiopacity associated with the root of the first premolar. The periodontal ligament space is intact and of regular thickness separating it/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


