Nephrology
Key Points
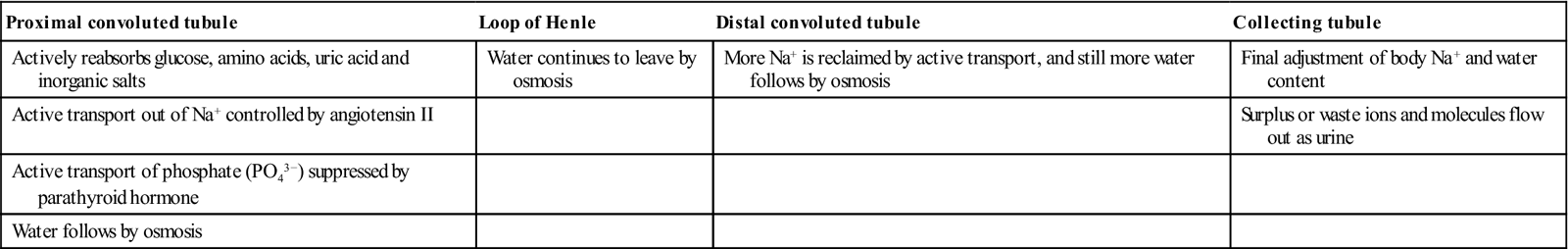
The kidneys (nephrons) have many functions, especially fluid and electrolyte balance, waste removal, acid–base balance, vitamin D metabolism and stimulation of erythrocyte production. The kidney makes urine by filtering small molecules and ions from the blood and then reclaiming useful materials such as glucose (Fig. 12.1). The nephron consists of a Bowman’s capsule, glomerulus (a capillary network within Bowman’s capsule), proximal convoluted tubule, loop of Henle, and distal convoluted and collecting tubules (Table 12.1).
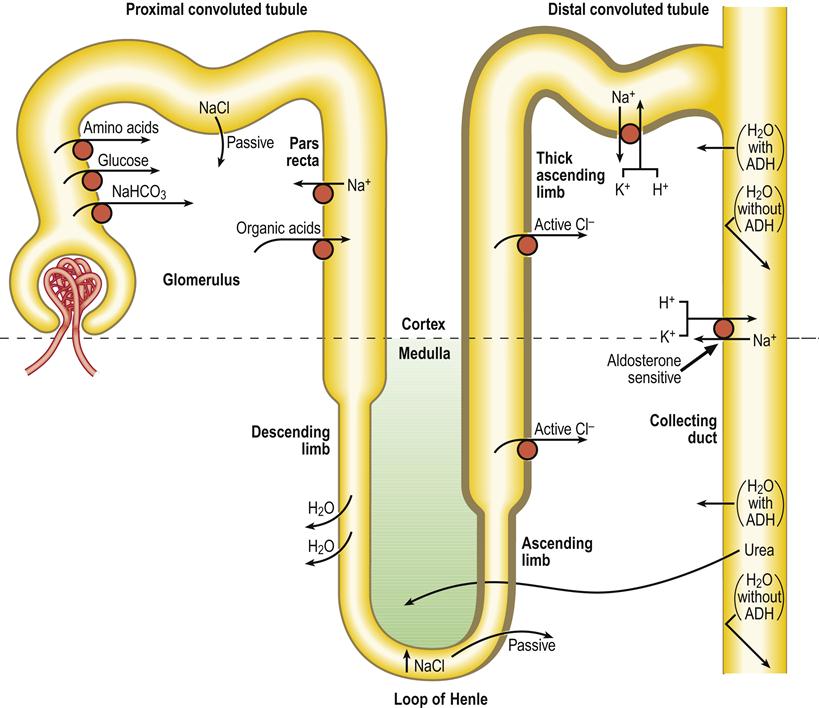
ADH=antidiuretic hormone; Cl−, chloride; H2O=water; H+, hydrogen; K+, potassium; Na+=sodium; NaCl=sodium chloride; NaHCO3=bicarbonate.
Table 12.1
The kidney: constituents and functions
< ?comst?>
| Proximal convoluted tubule | Loop of Henle | Distal convoluted tubule | Collecting tubule |
| Actively reabsorbs glucose, amino acids, uric acid and inorganic salts | Water continues to leave by osmosis | More Na+ is reclaimed by active transport, and still more water follows by osmosis | Final adjustment of body Na+ and water content |
| Active transport out of Na+ controlled by angiotensin II | Surplus or waste ions and molecules flow out as urine | ||
| Active transport of phosphate (PO43−) suppressed by parathyroid hormone | |||
| Water follows by osmosis |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
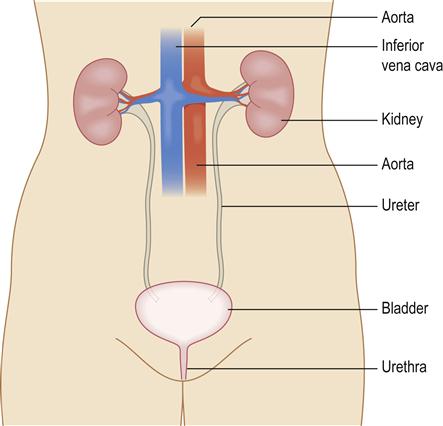
The kidneys constantly pass urine through the ureters to the bladder; it is stored in the bladder to be passed from time to time via the urethra (Fig. 12.2). Nearly a quarter of the blood volume perfuses the kidneys each minute. The glomerular filtration rate (GFR) can be calculated from creatinine clearance, inulin clearance, or clearance of isotopes, such as 125I-iothalamate, 51Cr-EDTA (ethylenediamine tetra-acetic acid) or 99mTc-DPTA (diethylenetriamine penta-acetic acid), or plasma creatinine levels; it is increasingly expressed as an estimate calculated by using the Modification of Diet in Renal Disease (MDRD) study equation, which takes into account patient age, gender and serum creatinine level. In health, the GFR is around 120 mL/min per 1.73 m2 for women and 130 mL/min per 1.73 m2 for men. In population terms, this declines by 1–2 mL/min per year over the age of 20 years. The kidneys also act in the excretion of drugs and hormones, and as endocrine organs for the synthesis of hydroxycholecalciferol (active vitamin D), erythropoietin, renin and prostaglandins, and as target organs for parathyroid hormone and aldosterone.
Renal failure can come on suddenly (acute renal failure; ARF), as after surgery or severe injuries, or when renal blood vessels become obstructed, but more usually develops slowly (chronic renal failure, CRF; chronic kidney disease, CKD). Renal failure results in fluid retention, acidosis, accumulation of metabolites and drugs, damage to platelets (leading to a bleeding tendency), hypertension, anaemia and endocrine effects.
Acute Renal Failure
Acute renal failure can be caused by pre-renal, renal or post-renal factors:
ARF is a medical emergency, which may lead to confusion, seizures and coma. Management is often by dialysis.
Chronic Kidney Disease (CKD; Chronic Renal Disease)
General aspects
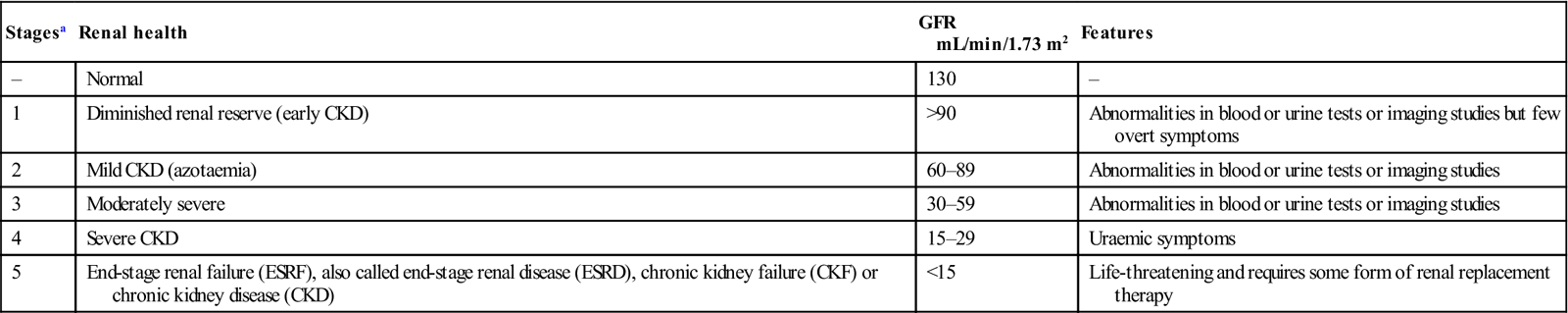
Chronic kidney disease is defined as kidney damage, or a reduction in the GFR, for 3 or more months. All individuals with a GFR of less than 90 mL/min per 1.73 m2 for 3 months are classified as having CKD, if there is also proteinuria or haematuria. They are at increased risk of loss of kidney function and development of cardiovascular disease (Table 12.2).
Table 12.2
Stages of chronic kidney disease
< ?comst?>
| Stagesa | Renal health | GFR mL/min/1.73 m2 | Features |
| – | Normal | 130 | – |
| 1 | Diminished renal reserve (early CKD) | >90 | Abnormalities in blood or urine tests or imaging studies but few overt symptoms |
| 2 | Mild CKD (azotaemia) | 60–89 | Abnormalities in blood or urine tests or imaging studies |
| 3 | Moderately severe | 30–59 | Abnormalities in blood or urine tests or imaging studies |
| 4 | Severe CKD | 15–29 | Uraemic symptoms |
| 5 | End-stage renal failure (ESRF), also called end-stage renal disease (ESRD), chronic kidney failure (CKF) or chronic kidney disease (CKD) | <15 | Life-threatening and requires some form of renal replacement therapy |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Historically, CKD has been classified according to the part of the renal anatomy involved, as follows:
CKD is said to be present when damaged kidneys perform their functions less well, causing waste substances such as urea to accumulate and leading to other issues. CKD is not a specific disease. The most common causes (75% of all adult cases) are diabetes, hypertension and glomerulonephritis. Renal diseases (e.g. chronic glomerulonephritis, polycystic renal disease, renal artery stenosis), systemic diseases (lupus erythematosus, myeloma, amyloid), poisoning (e.g. lead or betel) and drugs (e.g. long-term use of aspirin or other NSAIDs, or large amounts of paracetamol [acetaminophen]) are other causes.
CKD is more common among women than men. In men, it is 50% more likely than in women to progress to renal failure. It is seen in 35% of people aged 20 years or older with diabetes, and 20% of people aged 20 years or older with hypertension. Since diabetes and hypertension are both common in people of South Asian and of African heritage, such individuals have a high prevalence of CKD.
Other risk factors include cardiovascular disease, obesity, hypercholesterolaemia and a family history of CKD. Inadequately controlled diabetes and hypertension increase the risk of progression of CKD to kidney failure. Repeated kidney injury (e.g. infections, drugs or toxins injurious to the kidney) can also contribute to progression to kidney failure, especially in older people. CKD is usually irreversible and progressive and can lead to end-stage renal disease (ESRD; renal failure), through five stages defined by the National Kidney Foundation (see Table 12.2). CKD can be compensated by structural and functional hypertrophy of surviving nephrons, to a point at which around 50% of renal function remains, when chronic renal insufficiency ensues. This inevitably progresses to ESRD.
Clinical features
People with early CKD often have no symptoms; at this point, only a blood test to estimate kidney function and a urine test to assess kidney damage will help the diagnosis. Only when kidney function has fallen to less than 25% of normal do nocturia and anorexia appear, and serum levels of nitrogenous compounds (urea) become raised (azotaemia or uraemia). Later, problems such as cardiovascular disease (heart attacks, heart failure, heart rhythm disturbances and strokes), anaemia and bone disease cause clinical features.
Leading causes of ESRD are diabetes and hypertension. Less common causes include glomerulonephritis, hereditary kidney disease, and malignancies such as myeloma.
Premature death from both cardiovascular disease and from all causes is higher in adults with CKD compared to adults without CKD.
CKD can be associated with fluid overload, sodium and potassium imbalances, bone and mineral disorders, and anaemia. Advanced CKD causes significant impairment of all renal functions, affects virtually all body systems, and causes changes in urea and electrolytes and other blood constituents (Table 12.3; Fig. 12.3). CKD can manifest in a range of clinical features (Table 12.4). Purpura and a bleeding tendency may appear from abnormal platelet production (a consequence of diminished thrombopoietin production); diminished platelet factor 3 (thromboxane), which impairs conversion of prothrombin to thrombin; raised prostacyclin (prostaglandin I), leading to vasodilatation and poor platelet aggregation; and defective von Willebrand factor. Hypertension is common. Anaemia is frequently found and is caused by toxic suppression of the bone marrow, lack of renal production of erythropoietin and/or iron deficiency, from blood loss in the gut. A tendency to infection arises because of defective phagocyte function, which results from reduced interleukin-2 (IL-2) and increases in pro-inflammatory cytokines (IL-1, IL-6, tumour necrosis factor [TNF]).
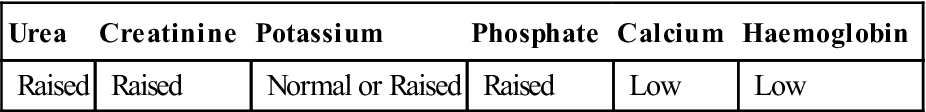
Table 12.3
Laboratory features of chronic kidney disease
< ?comst?>
| Urea | Creatinine | Potassium | Phosphate | Calcium | Haemoglobin |
| Raised | Raised | Normal or Raised | Raised | Low | Low |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
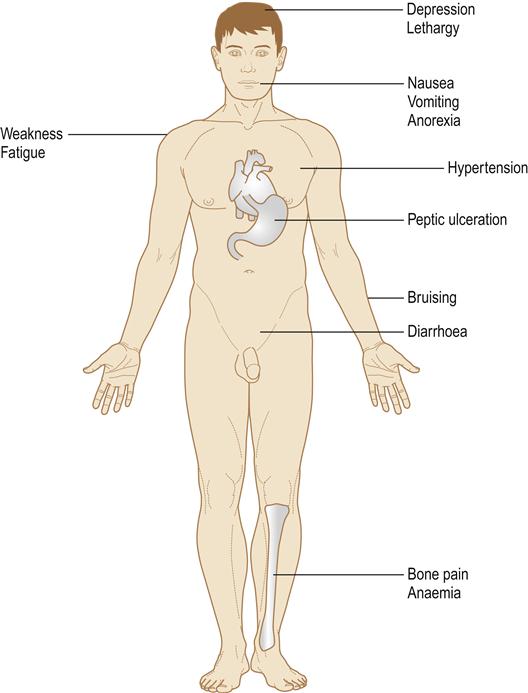
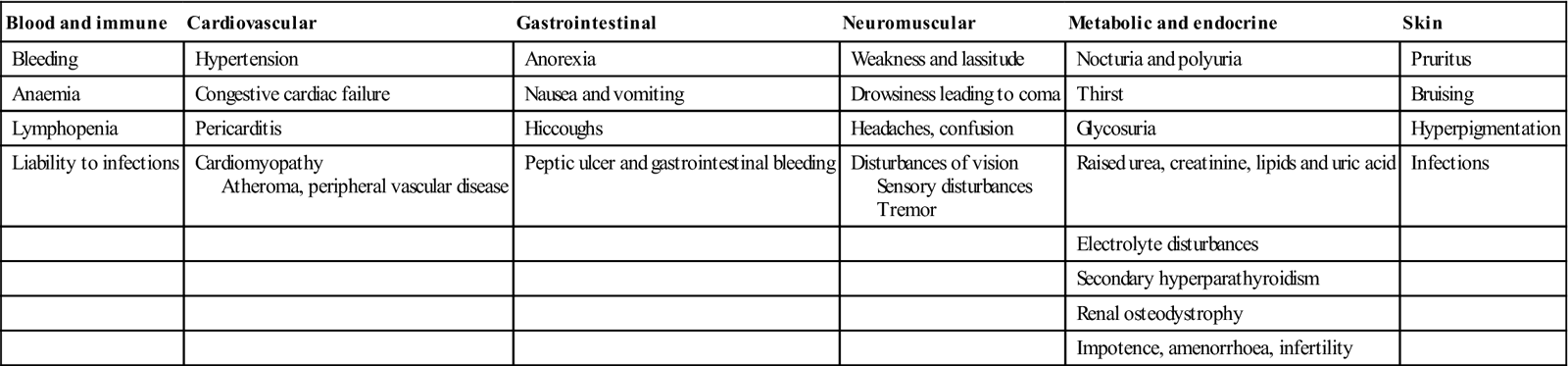
Table 12.4
Clinical features of chronic kidney disease
< ?comst?>
| Blood and immune | Cardiovascular | Gastrointestinal | Neuromuscular | Metabolic and endocrine | Skin |
| Bleeding | Hypertension | Anorexia | Weakness and lassitude | Nocturia and polyuria | Pruritus |
| Anaemia | Congestive cardiac failure | Nausea and vomiting | Drowsiness leading to coma | Thirst | Bruising |
| Lymphopenia | Pericarditis | Hiccoughs | Headaches, confusion | Glycosuria | Hyperpigmentation |
| Liability to infections | Cardiomyopathy Atheroma, peripheral vascular disease |
Peptic ulcer and gastrointestinal bleeding | Disturbances of vision Sensory disturbances Tremor |
Raised urea, creatinine, lipids and uric acid | Infections |
| Electrolyte disturbances | |||||
| Secondary hyperparathyroidism | |||||
| Renal osteodystrophy | |||||
| Impotence, amenorrhoea, infertility |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Renal osteodystrophy is common; phosphate retention leads to depression of plasma calcium levels and subsequently raised parathyroid activity (secondary hyperparathyroidism). There is also deficiency of renal production of 1,25-dihydroxycholecalciferol (vitamin D3) and calcium absorption is thereby impaired. Parathyroid hyperplasia may eventually become adenomatous and irreversible (tertiary hyperparathyroidism).
General management
CKD is diagnosed by clinical history and presentation, and by rising plasma urea (in the USA, blood urea nitrogen; BUN) and creatinine levels and a falling GFR, which is increasingly expressed as an estimate (eGFR; calculated by using the Modification of Diet in Renal Disease [MDRD] equation, which takes into account patient age, gender and serum creatinine level). There is also a correction that can be applied for those of Afro-Caribbean background.
The decline in eGFR can be plotted over time, allowing accurate prognosis (such as timing of requirement for dialysis, creation of arteriovenous fistulae, etc.). It also allows for demonstration of effects of therapy, the most important of which is control of blood pressure – by using ACEIs and angiotensin II blockers (ARBs). Underlying causes of CKD should be treated where possible and any stress, infection or urinary tract obstruction should be dealt with, as/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


