Alcohol and Substance Abuse
INTRODUCTION
Alcohol and other substance abuse by patients is a significant problem confronted by dentists in many countries. Alcohol, when consumed in moderation, is recognized to have cardiovascular and other health benefits.1 An otherwise healthy dental patient who consumes limited amounts of alcohol typically presents no limitations or contraindications to dental treatment. Patients who use alcohol to excess or patients who often use mind-altering substances, however, may have problems accepting, receiving, and completing dental treatment. Significant behavioral and medical issues can arise with the substance-abusing patient that may necessitate modifications to the dental treatment plan. Is some cases, treatment may need to be deferred, limited in complexity, or sequenced in a different manner. In addition, the alcohol- or substance-abusing patient is more likely to suffer from a variety of oral problems. It may be appropriate to refer the patient to a physician for management of related potential or imminent medical problems. It may be indicated or necessary to refer the patient to a counselor, therapist, or other substance abuse specialist to help manage the addiction and any related psychological or behavioral issues. Once the addiction is managed and any concomitant medical issues mitigated, the dentist may be able to treat the oral health issues in a routine manner. The dentist will need to remain aware, however, of the possibility of recidivism and be prepared to assist the patient in obtaining help to reestablish control of the addiction. Such possibilities represent unique challenges and will call upon skills and sensitivities on the part of the dental team that are not required when treating other patients.
The number of people who are substance abusers is increasing. Broadly defined, substance abuse (i.e., alcohol and other chemical dependencies combined) is currently the second most common psychiatric disorder in the United States.2 The focus of this chapter is to describe strategies that will help the general dentist and the dental team recognize alcohol and substance abuse in patients, to discuss how they can assist those patients in managing their addictions, and how treatment necessary to rehabilitate and maintain such a patient’s oral health can be planned and safely delivered.
Definition of Terms and Conditions
Patients who abuse drugs exhibit certain conditions recognized as addiction. These include a craving for more of the drug, increased physiological tolerance to exposure to the drug, and withdrawal symptoms in the absence of the drug. Addiction is characterized by repeated, compulsive use of a substance despite adverse social, physical, and/or psychological consequences. A wide range of substances, both legal and illegal, can be abused addictively.3
Drug tolerance occurs when a person’s reaction to a drug, such as alcohol or narcotics, decreases so that larger doses are required to achieve an equivalent effect. Drug tolerance often leads to physical dependence and addiction. The medical term referring to the rapid development of drug tolerance is called tachyphylaxis. For certain persons, the resulting pattern of uncontrolled escalating dosages may lead to a drug overdose.3
Physical addiction is defined as a physiologic state of adaptation to a substance, the absence of which produces symptoms and signs of withdrawal. Psychological addiction is a person’s need to use a drug out of desire for the effects it produces, rather than to relieve withdrawal symptoms. For example, heroin use eventually produces a physical addiction and, as the drug takes the place of natural endorphins, addicts may use heroin simply to reduce pain. Other drugs, such as marijuana, do not create a physical dependency or addiction. However, a person may become psychologically addicted if he or she comes to depend upon the drug’s effect as part of normal existence.3
A person can also be addicted to drugs to which they have not previously been exposed. This condition is known as cross-tolerance and is characterized by tolerance to a “new” drug as a result of long-term administration of a previous “drug of choice.” For example, a person who has developed tolerance to alcohol may not respond to the usual dose of an anesthetic. This occurs because increased tolerance to the effects of alcohol has also resulted in tolerance to the anesthetic.3
Withdrawal syndromes consist of a predictable group of signs and symptoms resulting from abrupt removal of, or a rapid decrease in, the regular dosage of a psychoactive substance. The syndrome is often characterized by hyperactivity of the physiologic functions that were suppressed by the drug and/or depression of the functions that were stimulated by the drug.3
The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) defines alcohol and/or substance dependence as a maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by three (or more) of the following, occurring at any time in the same 12-month period: (1) tolerance, as defined by either of the following: (a) a need for markedly increased amounts of the substance to achieve intoxication or desired effect or (b) markedly diminished effect with continued use of the same amount of the substance; (2) withdrawal, as manifested by either of the following: (a) the characteristic withdrawal syndrome for the substance or (b) the same (or a closely related) substance is taken to relieve or prevent withdrawal symptoms; (3) the substance is often taken in larger amounts or over a longer period than was intended; (4) there is a persistent desire to cut down or control substance use, but efforts to do so are unsuccessful; (5) a great deal of time is spent in activities necessary to obtain the substance (e.g., visiting multiple health care providers or driving long distances), use the substance (e.g., chain-smoking), or recover from its effects; (6) important social, occupational, or recreational activities are given up or reduced because of substance use; (7) the substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance (e.g., current cocaine use despite recognition of cocaine-induced depression or continued drinking despite recognition that an ulcer was made worse by alcohol consumption). The definitions for abuse/dependence of other substances follow the same criteria as for alcohol abuse/dependence.4
ALCOHOL ABUSE
Scope of the Problem
For most people, alcohol consumed in moderation is relaxing and provides a euphoric effect. For others, alcohol can be a problem. When an individual loses control while under the influence of alcohol, the results can be devastating. Such a person is at risk for development of systemic illnesses, impaired social functioning, home- and workplace-related difficulties, and legal problems, and is prone to life-threatening behaviors and activities. Under these circumstances, alcohol abuse is considered to be a psychiatric illness.4,5
The American Psychiatric Association divides alcoholism into two main components: alcohol abuse and alcohol dependence.4 Alcohol abuse occurs early in the disease process and is distinguished by the harmful consequences of repeated use. These episodes can alter mood, impair judgment, and keep individuals from completing their obligations. School and job performance invariably suffers, and neglect of family and household responsi-bilities is common. While under the influence, these individuals often participate in harmful and sometimes dangerous activities (e.g., driving while impaired), act inappropriately in social settings, get into arguments with family and friends, and either perpetrate or become victims of domestic violence. The consequences of their actions often lead to arrest and legal problems.5–8
Alcohol dependence is an advanced stage of the disease characterized by psychological dependence, increased tolerance, and/or withdrawal symptoms. During this phase, the individual needs to progressively increase the amount of alcohol used to achieve the same level of intoxication. Individuals in this stage may need to drink continuously to attain blood alcohol concentrations sufficient to prevent withdrawal symptoms. Heavy use of alcohol has been defined as chronic consumption of more than 14 alcoholic drinks per week or more than 4 drinks per occasion for men and more than 7 alcoholic drinks per week or more than 3 drinks per occasion for women.9
Alcoholism is a chronic, progressive disease characterized by a loss of control over the use of alcohol, with concomitant impaired social functioning and development of medical illnesses. The disease manifests in people who exhibit an uncontrollable craving for the alcohol-associated euphoria that results from the actions of certain neurotransmitters in the brain’s pleasure center. In time, these individuals develop tolerance to the effects of alcohol and suffer the symptoms of withdrawal when drinking stops (e.g., anxiety, rapid pulse, sweating, nausea, vomiting, and xerostomia).4,10,11
More than 14 million people meet the diagnostic criteria for alcohol abuse, making it the third most prevalent psychiatric disorder in the United States.5,12 Alcohol abuse and dependence can be found in any race, sex, age, or socioeconomic group. During their lifetimes, approximately 20% of men and 10% of women meet the diagnostic criteria for alcohol abuse, whereas 10% of men and 4% of women meet the diagnostic criteria for alcohol dependence.5,13,14 One study15 estimated that nearly two thirds of Americans older than 14 drink alcohol. Current figures indicate that more than 100,000 persons in the United States die each year because of alcohol abuse,12 with more than 20% of hospital admissions being alcohol related.16
In total, alcohol alone or in combination with other drugs, such as benzodiazepines, is estimated to be responsible for more overdose deaths in the United States than any other agent.17 The economic impact in the United States has been estimated to be more than $165 billion annually in direct treatment expenditures, reduced productivity, and premature death.14,18
Drinking patterns vary by age and gender. Men are two to five times more likely to become alcoholic than women.10 Men and women aged 21 to 34 years consume the most alcohol, with a gradually declining pattern of alcohol use after age 40.12,16,19 Women tend to start drinking heavily and develop alcoholism later in life than men. However, once it develops, alcoholism progresses more rapidly in women. Women experience higher blood concentrations of alcohol per kilogram after a given dose of alcohol than men because of their lower percentage of body water and higher percentage of body fat. Women also have less of the gastric enzyme alcohol dehydrogenase, or ADH, which metabolizes ethanol. With less alcohol broken down in the stomach, a proportionally larger amount enters the bloodstream. As a result of these higher alcohol levels, women are at greater risk of developing health-related consequences of heavy alcohol intake, such as cirrhosis, heart disease, and neurologic impairment.20
Most disturbing is the pattern of alcohol usage among younger people. One study21 estimated that 3.3 million people aged 14 to 17 years could be classified as problem drinkers. It is estimated that between 7% and 17% of college students have alcohol-related problems.22
Research has shown that many factors influence the risk of developing alcoholism. Studies have shown that genetic factors play a major role in determining if a person is at greater risk for alcoholism. These findings show that children of alcoholics are three to four times more likely than the general population to develop alcohol-related problems. These children are also at greater risk for behavioral and emotional problems. Certain aspects of family life also influence risk. Research has shown that a person’s risk increases if he or she is in a family in which an alcoholic parent suffers from chronic depression or has other psychological problems. Although the etiology of alcoholism remains ill defined, research suggests that a complex interaction of cultural influences, genetic predisposition, and neurochemical influences leads to an increased risk of alcohol abuse.23–27
Pathophysiology
The person who consumes one or two alcoholic drinks often feels more energetic, talkative, and outgoing than normal. This stimulating effect experienced by users while under the influence of alcohol is actually a disinhibition of personality. Instead of stimulating the central nervous system (CNS), alcohol actually depresses it. Alcohol slows normal brain function, becoming more sedating with increasing amounts of alcohol and, in higher doses, can become a general anesthetic. Tran-quilizers and sedatives are other examples of CNS depressants.
Alcohol and other CNS depressants should not be combined with any medication or substance that causes sleepiness, including prescription pain medications or certain over-the-counter cold and allergy medications. Such a combination can slow breathing, or slow both the heart and respiration, which can be fatal. A potentially deadly example of this process is the formation of cocaethylene in the body. When a person mixes cocaine and alcohol, they are compounding the danger that each drug poses. The result is a complex chemical process in the liver, which combines cocaine and alcohol to manufacture a third substance, cocaethylene. This new chemical intensifies cocaine’s euphoric effects, while dramatically increasing the risk of sudden death.
Chronic, high-dose alcohol abuse adversely affects nearly every organ system, including the oral cavity (see the What’s the Evidence? box). An associated problem is the development of low-grade hypertension, which in combination with increased levels of cholesterol fosters an elevated risk of cerebrovascular and coronary artery disease. Excessive alcohol ingestion may also damage cardiac muscle tissue, affecting myocardial contractility with resulting cardiomyopathy and congestive heart failure.5
Alcohol is an irritant to the gastrointestinal tract and may cause gastritis, gastric or duodenal ulcers, and in about 20% of chronic abusers leads to cirrhosis and pancreatitis. People with long-term alcohol abuse also experience increased rates of cancer of the pharynx, larynx, esophagus, and stomach.5,28
Alcohol abuse also frequently results in inadequate nutritional intake. Since alcohol ingestion often accounts for half of the daily caloric intake in abusers, it thereby displaces dietary proteins, minerals, and trace elements, such as magnesium and zinc. To compound this problem, chronic alcohol ingestion also causes malabsorption of folic acid; B-complex vitamins; thiamine (B1); riboflavin (B2); pyridoxine (B6); extrinsic factor (B12); and vitamins D, E, and K.5,29–31
Alcohol abuse has a deleterious effect on neural development. Acetylcholine and dopamine receptors are damaged, leading to motor and sensory disturbances. In the central nervous system, neuronal cell death and atrophy of several regions of the brain occur. Clinically, these anatomical changes correlate with deficits in judgment and decision-making ability, reduced attention span, short-term memory loss, emotional instability, and impaired coordination.5,32–34
Approximately half of all people who are diagnosed with alcohol abuse or dependence have additional psychiatric illnesses. When this situation occurs, the patient is said to have a “dual diagnosis.” These conditions may include anxiety, bipolar disorder, antisocial personality, and major depressive disorders. Although these patients are treated for and receive psychiatric medications for their psychiatric conditions, they are the least likely to abstain from alcohol use and are at greater risk of experiencing alcohol-associated morbidity and mortality. It is common for alcoholics to have multiple addictions, which include abuse of, or dependence on, other substances such as cocaine and nicotine.35–37
Any alcohol-dependent individual may develop these psychological conditions and concomitant cognitive impairment. In severe cases, neurologic damage may be permanent, predisposing the individual to alcohol amnestic disorder, which prevents recall of previously known material or causes the inability to learn and process new information. Alcoholic individuals have a propensity to develop depression because of the CNS effects from long-term alcohol abuse. Such individuals may also develop alcohol-related blackouts and some may have dementia and severe personality changes.
Other adverse effects of long-term alcohol abuse include impairment of the liver’s ability to produce coagulation factors and to metabolize medications, impairment of the chemotactic ability of white blood cells, and impairment of production of platelets in the bone marrow. Prolonged alcohol abuse leads to liver disease and can be expressed in three levels of severity: fatty liver, alcoholic hepatitis, and cirrhosis. The first changes in alcoholic liver disease are fatty infiltration of hepatocytes. The hepatocytes become engorged with fatty lobules, creating enlargement of the liver. This process is usually reversible.6,38
The second and more serious form of liver disease is alcoholic hepatitis. This condition is a widespread inflammatory condition characterized by cellular destruction. These changes may be irreversible and lead to necrosis, sometimes resulting in death if the damage is widespread. The clinical presentation of alcoholic hepatitis includes nausea, vomiting, anorexia, malaise, weight loss, and fever.6,38
The third and most serious form of liver disease is cirrhosis. Cirrhosis, the tenth leading cause of death among adults in the United States, is considered irreversible and is characterized by progressive fibrosis of the liver tissue. Cirrhosis results in a loss of excretory and metabolic function, leading to hepatic failure and associated morbidity, including diminished ability to detoxify drugs. The individual may develop bleeding problems secondary to the inadequate formation of prothrombin and fibrinogen and the eventual toxic effects on bone marrow. Individuals with cirrhosis are prone to anemia, hypoglycemia, hematemesis, melena, and lung abscesses. In advanced cases, cirrhosis can lead to hepatocellular carcinoma and ultimately death.6,38
OTHER ABUSED SUBSTANCES: SCOPE OF THE PROBLEM AND PATHOPHYSIOLOGY
Marijuana (Cannabis)
(Street names: pot, dro, ganja, weed, grass, bud, chronic, tree, herb, hash, Mary Jane, and reefer)
Marijuana is the most widely abused and readily available illegal drug in the United States. More than 95 million Americans over the age of 12 have tried marijuana at least once, and currently, there are 10 to 12 million users in the United States. The average age at first use is declining, and it is estimated that about half of U.S. teenagers try marijuana before finishing high school. Since 1991, lifetime marijuana use (“lifetime” refers to use at least once during a respondent’s lifetime) has almost doubled among eighth- and tenth-grade students, and increased by one third among high school seniors.39,40
All forms of cannabis are psychoactive (mind-altering) drugs. All contain THC (delta-9-tetrahydrocannabinol), the main active chemical in marijuana, and more than 400 other chemicals, including 66 other cannabinoids in each plant. Marijuana’s effect on the user depends on the potency of the THC it contains. THC concentrations in marijuana have steadily increased since the 1970s when concentrations were 1% to 2%. Today, most marijuana contains an average of about 5% THC, although higher concentrations of the active ingredient can be found in other forms. Sinsemilla (buds and flowers of the female plant) contains about 12% THC, but can range as high as 27%. Hashish (the sticky resin from the female plant flowers) and hash oil typically have THC concentrations of about 10%, although either may have concentrations as high as 40%.41,42
Marijuana affects the thought processes, mood, senses, and emotions of the user. Individuals using marijuana may experience dizziness; have difficulty walking; seem silly and giggle for no reason; exhibit increased appetite; have red, bloodshot eyes; and have difficulty remembering things that just happened. Some individuals experience an initial sense of well-being or euphoria and enhanced physical and emotional sensitivity, such as heightened feelings of interpersonal closeness.
Marijuana use has numerous effects on the nervous system, as a result of which, simple motor, complex psychomotor, and cognitive tasks are all impaired. The user experiences distorted perceptions of sights, sounds, time, and touch. Some users claim to have more acute visual and auditory perceptions and to perceive time as passing very slowly. They may also exhibit loss of hand-eye coordination, have delayed reaction times, and show errors in judgment, increasing the risk of motor vehicle accidents. Once these early effects fade over a few hours, the user usually becomes very sleepy and lethargic and sometimes withdrawn, depressed, fatigued and, at times, hostile.
Amotivational syndrome is frequently seen in chronic marijuana users. This is characterized by a loss of interest and desire to study or work, decreased energy or productivity, and generalized apathy, sullenness, moodiness, and inability to concentrate. Chronic users may exhibit an unkempt appearance and adopt a lifestyle that revolves around procurement of the drug.41
Short-term effects of marijuana use include memory and learning problems, distorted perception, and difficulty thinking and solving problems. Some re-searchers suggest that long-term marijuana use may create changes in the brain that result in a higher risk of becoming addicted to other drugs, such as alcohol or cocaine.43,44
Studies show that very few young people use other drugs without first trying marijuana, alcohol, or tobacco. Few young people use cocaine, for example, but the risk is greatly increased in youth who have tried marijuana compared with those who have never tried it. It is for this reason that many people describe marijuana as a “gateway” drug, leading to usage of more risk-associated substances.45
Cocaine
(Street names: coke, C, snow, flake, blow)
Cocaine abuse and addiction is a major health problem in North America. In 2002, an estimated 1.5 million Americans were classified as dependent on or having abused cocaine during the past 12 months, according to the National Survey on Drug Use and Health (NSDUH, formerly known as the National Household Survey on Drug Abuse). The same survey estimates that there are 2 million current users (i.e., used cocaine during the past month) and an estimated 567,000 current crack users. Adults 18 to 25 years old have the highest rate of cocaine use compared with other age groups.46
Cocaine is a powerfully addictive drug, which can be snorted, sniffed, injected, or smoked. Cocaine is an extract from the leaf of the Erythroxylon coca bush, primarily grown in Bolivia and Peru, and is marketed in two chemical forms, the hydrochloride salt (powdered) and freebase (rock). The powdered form of cocaine readily dissolves in water and can be administered intravenously or intranasally. Freebase refers to a processed form of cocaine that has not been neutralized by an acid to make the hydrochloride salt; this form of cocaine can be smoked. The term “crack” refers to the crackling sound heard when the mixture is smoked. Cocaine usually makes the user feel euphoric and energetic, although large amounts can cause bizarre and violent behavior.46
Several potentially severe medical complications are associated with cocaine use. Some of the most frequent are cardiovascular effects, including disturbances in heart rhythms (ventricular fibrillation), heart attacks, strokes, and hypertension. Cocaine abuse may cause respiratory effects, such as chest pain and respiratory failure; neurologic effects, seizures, and headaches; and gastroin-testinal complications, including abdominal pain and nausea.47
Different routes of cocaine use can produce different adverse effects. Persons who inject cocaine may have needle tracks (venipuncture sites) on various parts of the body, but most commonly on their forearms. Intravenous cocaine users may also experience allergic reactions, either to the drug or to some additive in street cocaine which, in severe cases, can result in death. Intravenous drug users are also susceptible to subacute bacterial endocarditis (SBE) and should be referred for a medical consultation to determine if prophylactic antibiotics are necessary before receiving dental treatment.
Potential long-term effects of snorting cocaine include nosebleeds, problems with swallowing, hoarseness, loss of sense of smell, and an overall irritation of the nasal mucosa, which can lead to a chronically inflamed, runny nose. Chronic cocaine users should not be given local anesthetic containing epinephrine because of the vasoconstrictive effects of the epinephrine, which can lead to an acute hypertensive crisis. It is of paramount importance that these patients inform the dentist if they have used cocaine before their dental appointment. Although most cardiovascular effects of cocaine diminish a few hours after use, the blood pressure can remain elevated. Even if the patient claims to have stopped using the drug, it is imperative to take the blood pressure before initiating treatment.46,47
Because cocaine has a tendency to cause loss of appe-tite with resulting decreased food intake, many chronic cocaine users experience significant weight loss and malnourishment. There is a potentially dangerous interaction between cocaine and alcohol. Taken in combination, the two drugs are converted by the body to cocaethylene, which has a longer duration of action in the brain and is more toxic than either drug alone. The mixture of cocaine and alcohol is the most common two-drug combination resulting in drug-related deaths.48
Heroin
(Street names: smack, H, ska, junk, horse)
Heroin is a highly addictive drug with a very high abuse potential, and its use is a serious problem in North America. In 2003, the National Survey on Drug Use and Health estimated that 3.7 million Americans have or will have used heroin during their lifetimes. During the past year, 315,000 Americans reported using heroin. The highest numbers of users are found among individuals 26 years of age and older. In 2003, 57% of past heroin users were classified as dependent on or abusing heroin. The Community Epidemiology Work Group (CEWG), reporting in December 2003, identified heroin as the primary drug of abuse for people in drug abuse treatment centers in major U.S. cities.48
Recent studies suggest a shift from injecting heroin to snorting or smoking because of increased purity and the misconception that these methods of drug delivery are safer. Heroin is processed from morphine, a naturally occurring substance extracted from the seedpod of the Asian poppy plant, and usually appears as a white or brown powder. The Drug Abuse Warning Network (DAWN) lists heroin and morphine among the four most frequently mentioned drugs reported in drug-related deaths in 2002. In the United States, hospital emergency room admissions caused by heroin overdoses have increased by 35% since 1995.48
After injecting heroin, the user reports a surge of euphoria, commonly referred to as a “rush.” This is accompanied by a warm flushing of the skin, dry mouth, and heavy-feeling extremities. Following this initial euphoria, the user alternates between a drowsy and a wakeful state. Mental functioning slows as a result of depression of the CNS. These effects usually last for a few hours. Long-term effects of heroin appear after repeated use of the drug. Chronic users often develop collapsed veins, abscesses, cellulitis, liver disease, and infections of the heart lining and valves.
Heroin is a CNS depressant, which can have serious effects on respiration. Heroin abusers frequently have pulmonary complications, including various types of pneumonia. Heroin abuse has been associated with fatal overdose, spontaneous abortion, and particularly in users who inject the drug infectious diseases, including hepatitis and human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS).
Tolerance develops with regular heroin use and, with time, the abuser must use more of the drug to achieve the same intensity of effect. As higher doses are used, physical dependence and addiction develop. Once the body has adapted to the presence of the drug, withdrawal symptoms occur if its use is reduced or stopped. Withdrawal typically begins a few hours after the last drug administration, with the patient experiencing a number of physical side effects. These may include drug craving, restlessness, muscle and bone pain, diarrhea and vomiting, cold flashes with goose bumps (“cold turkey”), involuntary kicking movements (“kicking the habit”), insomnia, and other symptoms. Major withdrawal symptoms peak between 48 and 72 hours after the last dose and subside after about a week. Sudden withdrawal by heavily dependent users who are in poor health is occasionally fatal, although heroin withdrawal is considered less dangerous than withdrawal from alcohol, barbiturates, or benzodiazepines.49
Stimulants
Methamphetamine
(Street names: meth, speed, chalk, ice, crystal, glass, or crank)
Drugs in this category are amphetamine or amphetamine-like derivatives. The abuse of methamphetamine, a potent psychostimulant, is an extremely serious and rapidly growing problem. According to the 2003 National Survey on Drug Use and Health, more than 12 million Americans age 12 and older have tried methamphetamine at least once in their lifetimes. The majority of past-year users were between 18 and 34 years of age. Methamphetamine is a powerfully addictive drug and has an extremely high potential for abuse.48
Methamphetamine is a white, odorless, bitter-tasting crystalline powder that easily dissolves in water or al-cohol. The drug was developed during the early twen-tieth century from its parent drug, amphetamine, for use in nasal decongestants, bronchial inhalers, and other medications.
Methamphetamine’s chemical structure is similar to that of amphetamine, but it has more pronounced neurotoxic effects on the CNS. Like amphetamine, it causes increased wakefulness and physical activity, decreased appetite, and a general sense of well-being. The effects of methamphetamine can last 6 to 8 hours. After the initial “rush,” there is typically a state of high agitation that in many individuals can lead to violent behavior. Chronic, long-term use can lead to psychotic behavior, hallucinations, and stroke.
Methamphetamine comes in many forms and can be smoked, snorted, orally ingested, or injected. The drug alters moods in different ways, depending on how it is taken. Immediately after smoking the drug or injecting it intravenously, the user experiences an intense rush or “flash,” which lasts only a few minutes and is described as extremely pleasurable. Snorting or oral ingestion produces euphoria, a high, but not an intense rush. Snorting produces effects within 3 to 5 minutes, and oral ingestion produces effects within 15 to 20 minutes. Methamphetamine is most often used in a “binge and crash” pattern. Tolerance for methamphetamine occurs within minutes, meaning that the pleasurable effects disappear even before the drug concentration in the blood falls significantly, so users try to maintain the high by bingeing on the drug.
In the 1980s, “ice,” a smokable form of methamphetamine, came into use. Ice is a large, usually clear crystal of high purity that is smoked in a glass pipe like crack cocaine. The smoke is odorless, and leaves a residue that can be resmoked, producing effects that may continue for 12 hours or more.
Methamphetamine can cause a variety of cardiovascular problems. These include inflammation of the heart lining, rapid heart rate, irregular heartbeat, increased blood pressure, and irreversible, stroke-producing damage to small blood vessels in the brain. Hyperthermia (elevated body temperature) and convulsions occur with methamphetamine overdoses and, if not treated immediately, can result in death. Methamphetamine abusers also can have episodes of violent behavior, paranoia, anxiety, confusion, and insomnia. Heavy users also show progressive social and occupational deterioration. Psychotic symptoms can sometimes persist for months or years after use has ceased.46,48
Meth Mouth
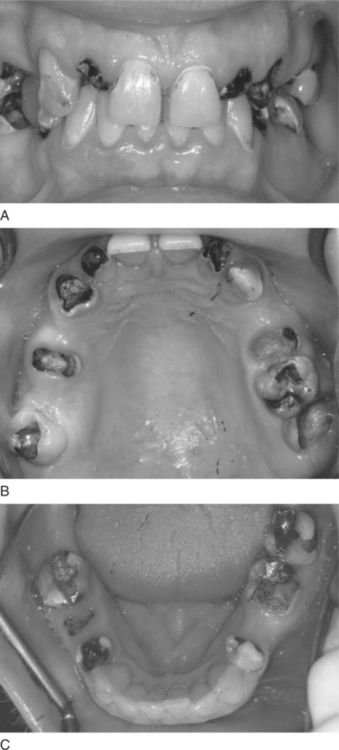
Of great importance to dentists is the increasing number of patients addicted to methamphetamine who exhibit the oral condition known as “meth mouth.” “Meth mouth” is characterized by dry mouth, gingivitis, periodontal disease, cracked teeth, and severe dental caries (Figure 12-1).
The xerostomia seen in these patients is caused by a direct inhibitory effect of methamphetamine on the salivary glands. By itself, diminished salivary flow can contribute to gingivitis, stomatitis, and dental caries. Methamphetamine also has an effect on the microvasculature, impeding the blood supply to the periodontal tissue. Typically superimposed on these physiologic problems are the ill effects of the methamphetamine user’s unhealthy lifestyle choices, including poor oral and general health, poor nutritional intake, and episodes of getting high and passing out or other antisocial behaviors. When high, methamphetamine users frequently exhibit violent behaviors that lead to traumatic injury inflicted upon themselves or others. Methamphetamine users may also commit criminal acts, such as robbery or theft, to support their habit. Poor oral self care and frequent or binge consumption of large volumes of highly sweetened carbonated drinks are also part of the pattern of drug abuse. The latter occurs in a vain attempt to treat dry mouth with large amounts of sugary soda. Generally, caffeinated beverages are preferred as they are also more likely to sustain the meth high between ingestion episodes. Meth users are not inclined to rinse, brush, or floss when high. Collectively, these issues can have devastating consequences in the oral cavity particularly with the development of rampant caries.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses