Chapter 10
CHECKING OCCLUSAL CONTACTS, OCCLUSAL SCHEMES, ALTERING THE VERTICAL DIMENSION
Checking of Occlusal Contacts
Restorations must be checked in the mouth for occlusal contacts. Castings should be cemented with a mixture of two parts Vaseline dispensed from a 2 ml syringe, to one part each of Tempbond catalyst and base.1 Porcelain inlays and onlays are usually checked following cementation, to reduce the possibility of fracture. However, if it is anticipated that laboratory polishing will be required, the restoration can be tried in using a silicone fit checker (Fitchecker-G. C. Dental Ind. Co.) as a supporting base. There is still the possibility of inducing fracture, but less than in the absence of the fit checker. Four techniques are unsed for checking contacts:
- Occlusal tapes.
- Shimstock.
- Sandblasted surfaces.
- T-scan.
Occlusal Tapes
It is sometimes helpful to administer 30 mg of propantheline bromide (Pro-Banthine) one hour prior to the appointment (see Premedication – Chapter 8) to reduce the salivary flow.
The teeth are dried with a MediWipe (Kleenex Ltd.). Fifteen micron black on black and red on red tapes are used (Occlusal tape GHM – Occlusion, Pruf-Folie, 22 mm). The tape is held between the teeth with the aid of Miller’s forceps (GHM) (Fig 10-1a) and the mandible guided to centric relation contact position, intercuspal position or any excursive position requiring checking.
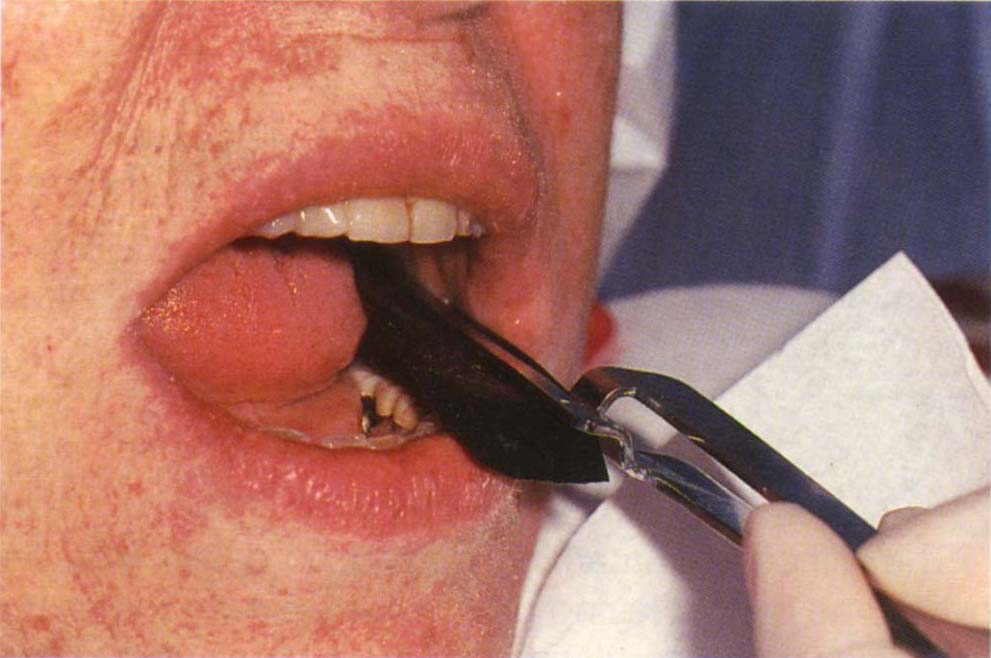
Fig. 10-1a GHM tape in Miller’s forceps. Note that the tape is held flat by the long beaks of the forceps. The tape is inserted by the chairside assistant whilst the dentist manipulates the mandible.
The occlusion is assessed by examining the marks on the teeth (Fig 10-1b) and by holding the tape to the light when small perforations in the marking ink will be seen which, with experience, can be located on the teeth. It was reported by Kelleher, in 1978,2 that the density of the colour of the mark on the tooth is not related to the force of contact, and that heavier contacts tend to spread the mark peripheral to the actual contacting area, with the latter being devoid of ink.

Fig. 10-1b Black marks on teeth.
The difficulty of marking glazed porcelain may be overcome by first laying down blue marking ink using very thick, soft articulating paper, such as, thick blue articulating paper (Dentsply Ltd.). If the red GHM tape is then used, it will mark well on the blue surface (Fig 10-1c). Sometimes, when used alone, the GHM tape will mark satisfactorily if lightly coated with Vaseline.
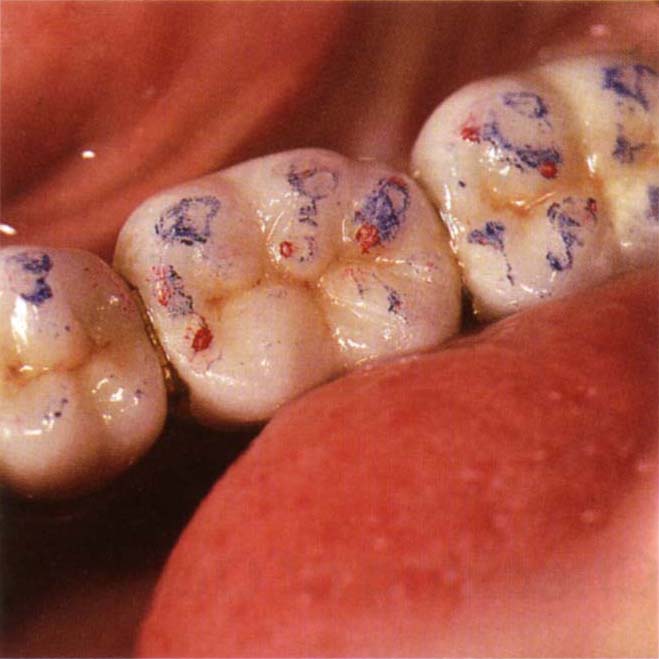
Fig. 10-1c Red marks on the blue surface which was laid down by the patient rubbing the teeth on thick soft blue articulating paper. This is useful for marking porcelain.
Shimstock
This 12 micron foil can be held in mosquito forceps and placed between the teeth (Fig 10-1d) (GHM). On closure, resistance when pulling the foil buccally indicates tooth contact. However, with mobile teeth it must be appreciated that shimstock, like marking tape, will indicate tooth contacts on teeth which are not necessarily initial contacts. If the initial contacts are indeed on mobile teeth, these teeth will be depressed, the secondary contacts on other teeth will than appear to be primary contacts.

Fig. 10-1d Shimstock between the teeth, held in Mosquito forceps. Resistance implies tooth contact. Mobile adjacent teeth may be depressed bringing the test teeth into contact yet solid casts would not show the contacts.
Sandblasted Surfaces
For gold occlusal surfaces, sandblasting with 15 micron aluminium oxide will produce a matt finish which will readily mark, making contacts easy to observe without the use of tape, the contacts appear as shiny areas.
T-Scan (Fig 10-1e)
According to the manufacturers (Tex Scan Inc.), this electronic device enables tooth contacts to be observed on a monitor screen and it also indicates relative forces on each of these contacts (Figs 10-1f+g). However, in a study of two volunteers, Lyons et al. (1992)3 concluded that ‘a given tooth contact force can produce a different column height each time it is recorded, it is clear that column heights are largely irrelevant and simply serve to indicate the presence of a contact and not the force of the contact’. Hsu et al. (1992) reported ‘the sensor did not have uniform sensitivity throughout the surface and that it was not reliable in recording occlusal contacts.4 Furthermore, the number of recorded occlusal contacts varies between different sensors and within the same sensor between trials’.
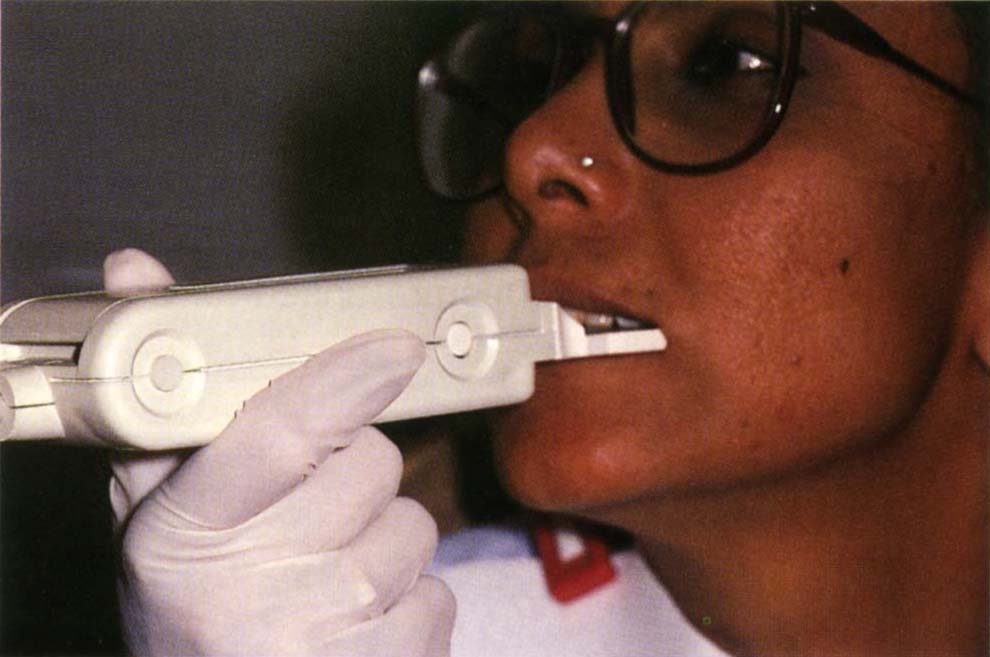
Fig. 10-1e T Scan handpiece.
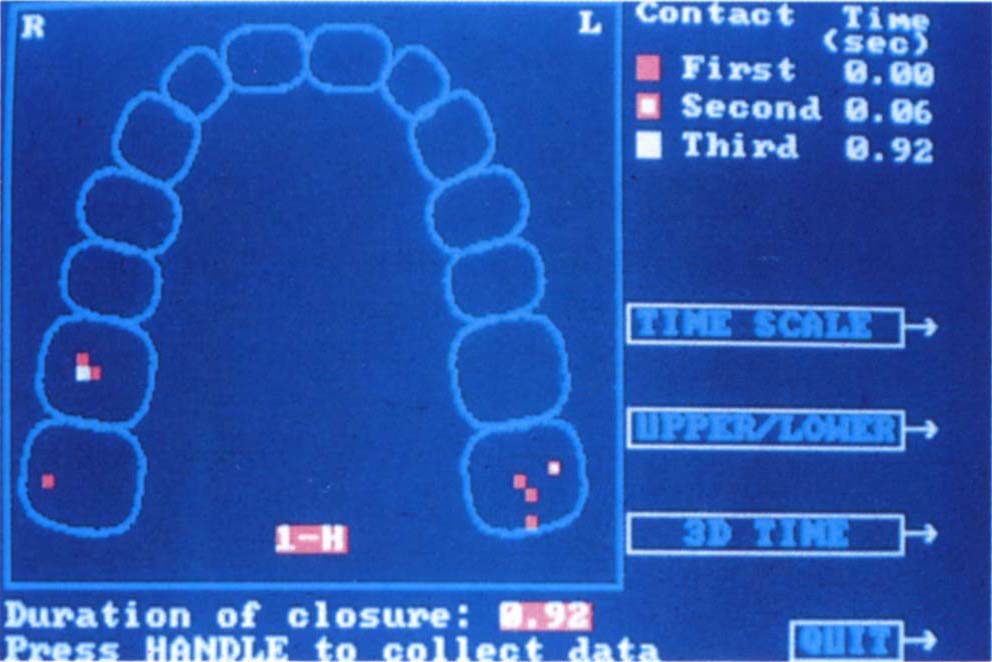
Fig. 10-1f Screen showing primary, secondary and tertiary contacts and their location.
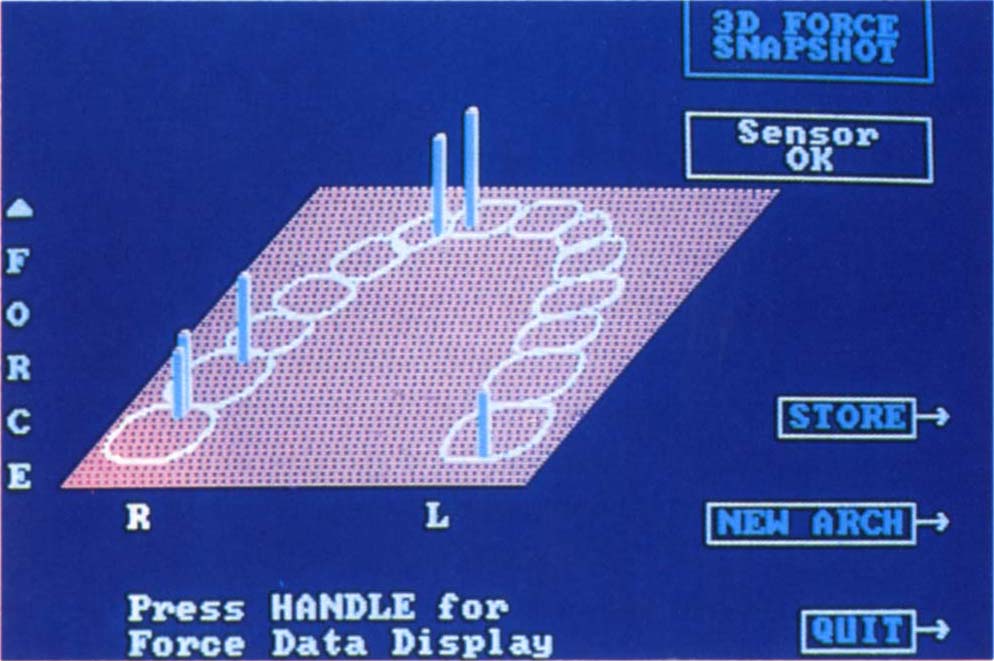
Fig. 10-1g Screen showing force mode. The higher the bar the greater the force. Whether there is an accurate correlation between bar height and force requires further investigation, however in its dynamic function, this mode is particularly useful for detecting non-working contacts.
However, using the dynamic mode, this instrument has been found useful in locating non-working side contacts and working side contacts between the lingual cusp of mandibular teeth and the palatal cusp of maxillary teeth. One disadvantage is that the size of the holder which is placed in the mouth can influence the patient’s ability to close their mouth freely and naturally. The T-Scan identifies the approximate location of contact, but tape marking is required for exact location. This is a useful instrument when used in conjunction with tapes, shimstock and sandblasted surfaces.5
Occlusal Schemes
The clinician must prescribe the precise form of the occlusal contacts to be provided on the restorations. There are several possibilities and thought must be given to the detail of the occlusal scheme prescribed. The reasons for considering the occlusion are:
- Facial arthromyalgia (Temporomandibular Disorders).
- Periodontitis.
- Mobility.
- Bruxism.
- Osseointegrated fixtures.
- Tooth stability.
- Comfort.
- Mechanical failure of restorations, teeth, fixtures.
- To maintain control and thereby a predictable sequence of treatment.
Facial Arthromyalgia
See Chapters 26 and 27. There is no published controlled evidence to support the traditional view that occlusal disharmonies are aetiologic, nor that their removal will remove symptoms more effectively than placebo adjustment. Alteration of the occlusion with the prime objective of treating the facial arthromyalgia cannot be recommended. Management of the patient with facial arthromyalgia who requires re-restoration because of failure of existing restorations is considered in Chapters 26–28.
Periodontitis
See page 225. Alteration of the occlusion with the prime objective of treating periodontitis cannot be recommended.
Mobility
Increasing mobility or mobility that concerns the patient may require occlusal management (see page 80).
Bruxism
Wruble et al. (1989) highlighted the inaccuracy of measuring and recording bruxism in many published dental studies, invalidating the conclusions.6 These authors also emphasise the central aetiology for the initiation of bruxism. Holmgren et al. (1993) reported that although TMD symptoms were reduced by occlusal splint therapy, bruxism continued on the splint.7 There is no published controlled evidence to support the view that alteration of the occlusion will eliminate bruxism. However, alteration of the occlusion can influence on which sites a patient bruxes. If, for example, bruxism occurs on the first molar and this tooth were extracted, then it obviously will no longer occur at this site. Occlusal management aims to direct the forces generated during bruxism through those areas of teeth, restorations and fixtures that are best suited to accept them thereby reducing: mechanical failure; mobility; and wear.
Osseointegrated Fixtures
See Chapter 33. Patients are less able to detect occlusal contacts on fixtures than teeth. Occlusal overload can result in mechanical and biological failure of fixtures.
Tooth stability
Posterior deflective contacts or loss of posterior occlusal support can result in drifting of the maxillary incisors. Movement of unsplinted teeth can result in opening of proximal contacts and food packing.
Comfort
It has been demonstrated that it is possible to detect on teeth an 8 to 10 micron occlusal discrepancy and that a 60 micron discrepancy is always detected.8–9 Tactile sensitivity is approximately three times less on fixtures.10 Occlusal interferences cause discomfort in the teeth.11–12 It can be concluded that on a tooth-supported restoration, small occlusal discrepancies can be detected and cause discomfort. The level of detection may be related to arousal, the phlegmatic patient being relatively unaware, whereas the anxious tense patient being very sensitive. The awareness and discomfort are very pertinent reasons for paying attention to the occlusion, but should not be confused with facial arthromyalgia.
Mechanical Failure
There is no published controlled evidence which demonstrates that management of the occlusion can reduce the incidence of mechanical failures in the restored dentition. However, Williamson et al. (1983) have demonstrated that elimination of lateral posterior contacts decreases the activity of the elevator muscles.13 Furthermore, disclusion prevents lateral forces being applied to posterior restorations during bruxism (see page 290). Until proven otherwise, it is prudent to minimize forces that can cause mechanical failure and hence attention should be paid to the occlusion.
Maintain Control
Correct occlusal management enables the clinician to maintain control over: the patent’s jaw relationships; the space between opposing restorations; the direction of forces applied to the restorations and the location of those forces on the restoration. This enables treatment to proceed in a predictable manner.
Basic Principles
Regardless of the type or number of restorations, the occlusal scheme to be employed must be decided before restoration. The different schemes have common aims which are:
- Teeth position should remain stable following restoration: the arrangement should be as in Figure 10-2a and not as in Figure 10-2b, in which instability can occur with tilting of teeth.
- The restoration must not introduce new deflective contacts.
- There should be simultaneous contact between the restoration and other teeth in the IP, with neither high spots nor lack of occlusion. It should be noted that small high spots may remain undetected by the clinician since the tooth is intruded following initial contact.
- There should be no non-working side contacts on the restoration as these produce rotational forces on the tooth and restoration (Figs 10-2c+d), but their removal is dependent on there being working side contacts to ‘pick up’ the guidance.
- There should not be working side interferences on the restoration (these often occur on lingual cusps and are difficult to detect).
- The anterior guidance should be in harmony with the temporomandibular joints and musculature and should not introduce an occlusal interference.
- Occlusal forces should be directed through the strongest areas of the restorative material and tooth.
- Occlusal forces should be directed along the long axes of teeth.
Fig. 10-2 Tooth to tooth stability. Buccolingual diagram (BU = buccal, L = lingual).
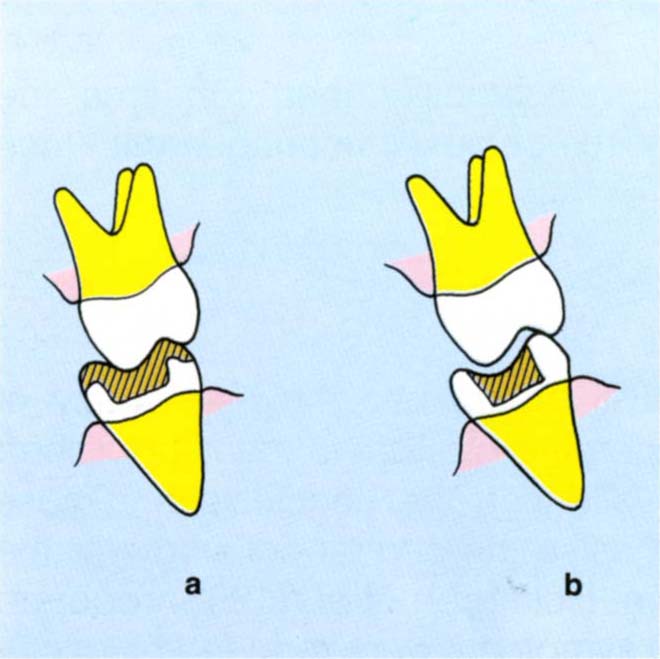
Fig. 10-2a Stable relationship between a restoration and the opposing tooth. Compare this with
Fig. 10-2b where the relationship is unstable.
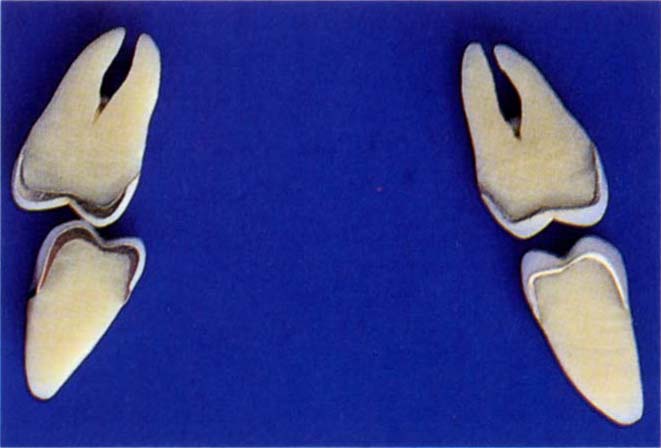
Fig. 10-2c Non-working contact on a crown causes rotational forces during any bruxist activity. This can uncement the crown or cause fracture of porcelain as these forces will be horizontal and unfavourable.
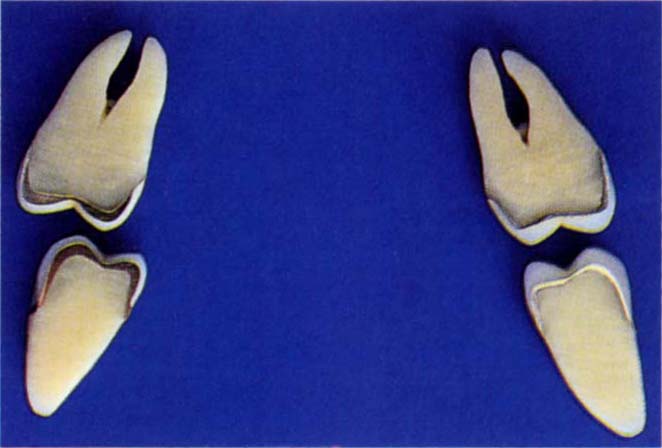
Fig. 10-2d (i) Disclusion removes horizontal forces during bruxism.
Fig. 10-2d (ii) Disclusion on non-working side but there is a working side interference between the lingual cusps. If viewed from the buccal aspect, it would appear that there was disclusion on the working side.
There are Essentially Two Approaches to Treatment, Namely:
• Conformative
• Reorganized
The reader is advised to read the section commencing ‘Adaptation’, Chapter 4, to refresh his understanding of the effects of removing deflective contacts, before continuing with this section.
Conformative Approach
Restorations are fabricated to the existing jaw relationships.14 With this approach minimal adaptation, if any, will be needed by the patient. The restoration should ‘fit into’ the existing neuromuscular patterns. Tooth form can be altered, but the following guidelines are observed:
The Existing Intercuspal Position is Maintained
The objective is to retain the existing intercuspal position.
Wherever Possible, Techniques must be Used which Facilitate the Fabrication of New Restorations which Fit into the Existing Intercuspal Position
Techniques for restoring to the intercuspal position are described in Chapter 12.
Techniques are Used which Enhance Retention of the Existing Intercuspal Position (Chapter 12)
Not only should the new restorations conform to the existing intercuspal position, but they should also help retain it, that is, existing deflective contacts (contacts which alter the closure from one path to another) may need to be copied on the new restorations. Deflective contacts on teeth which are not to be re-restored are left.
If the patient has a large horizontal : vertical ratio, particularly in conjunction with a previous history of clicking of the TMJ which has now resolved, it is not sensible to remove deflective contacts, since distal repositioning of the condyle could result in an altered condyle/meniscus relationship, possibly with recurrence of the click. Techniques should be used which enable the deflective contacts to be built back into the new restorations. This requires more laboratory and surgery time and this must be anticipated.
Remove Deflective Contacts if on One or Two Teeth are to be Restored
Deflective contacts alter closure from one path to another. Their removal will frequently result in a new habitual path of closure terminating in a new intercuspal position (Figs 10-2e–j). In a patient with a large vertical : horizontal ratio, or a large horizontal : vertical ratio in which the horizontal component is less than 1 mm and the patient is not occlusally aware, if one or two of the teeth to be re-restored are deflective contacts it may be sensible to remove these contacts some time before re-restoration, to allow the mandible to adopt a slightly altered path of closure if ‘the muscles so desire’ – and then work to the new intercuspal position. If this procedure is not carried out there is a danger that such change will take place during the temporary stage, as a result of tooth preparation leading inevitably to removal of deflective contacts. The occlusion on the definitive restorations will then differ from that fabricated in the laboratory. Rarely is it possible to exactly copy the deflective contacts on the temporary restorations. For a phlegmatic patient, this may not be of consequence, but for any occlusally aware patient it may introduce time-consuming complications. It must be pointed out that this is not occlusal equilibration, merely adjustment of one or two inclines prior to restoration. It is obviously a slight modification of the conformative concept, since the intercuspal position that is being restored to differs slightly from the original intercuspal position. However, it does avoid clinical complications and should be seriously considered.
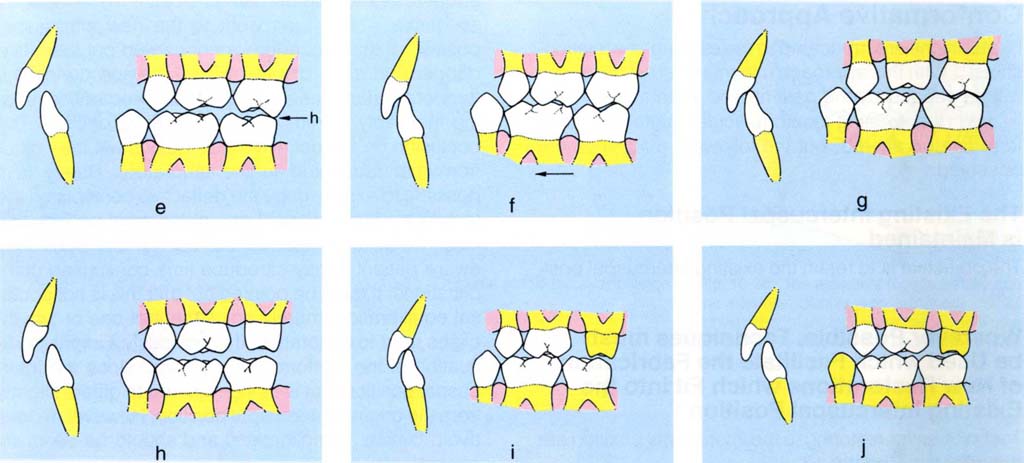
Figs 10-2e to j Diagrams to illustrate several possibilities when crown preparations are made: (e) CRCP initial contact 27-37 (H); (f) IP – the mandible is more anterior than in (e), avoiding the deflective contact between 27 and 37; (g) 26 prepared for crown, the deflective contact has not been touched and, therefore, the IP is retained; (h) 27 prepared for crown, in so doing the deflective contact has been removed; (i) the original IP may be retained and there is room for the restoration; (j) adaptation may occur, the mandible moving along a new path of closure, resulting in insufficient room for the restoration.
Removal of Non-Working Side Contacts Prior to Re-Restoration
As can be seen from Figures 10-2k–m, a non-working side contact tends to guide the mandible during lateral excursion. Removal of the existing restorations decreases the vertical component of the movement pathway, since now the condyle in the fossa will be guiding the movement. The preparation may contact the opposing tooth. There will be insufficient space for the restoration in lateral excursion, so that cementation of the restoration creates a new non-working side contact (Fig 10-2m). If the patient is occlusally aware, or under stress, adaptation will almost certainly be slow and discomfort is likely, since the original contact to which the patient will have gradually adapted was probably long standing. In response to the patient’s complaint of discomfort, frequently the restoration is ground, either exposing metal beneath porcelain, or perforating the casting. The technician is often blamed, whereas the fault was the clinician’s for not recognizing the problem originally.
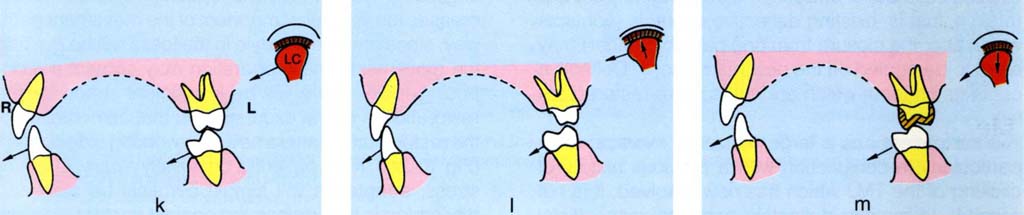
Fig. 10-2k to m The effect of not removing a non-working side contact. Buccolingual diagram through three levels (LC = left condyle, F = left fossa; R = right, L = left). Section through 13, 43, 27, 37 and the left condyle and fossa. If a non-working side contact is not eliminated prior to tooth preparation, it is probable that a new non-working contact will be introduced by a restoration. This is due to the reseating of the condyle in the fossa with a reduction of intra-occlusal space and a shallower path of mandibular movement. This is particularly liable to occur if the last tooth in the arch is prepared. It is advisable to remove the contact prior to preparation, provided that there is a tooth on the other side to provide anterior guidance.
Non-working side contacts can only be removed prior to re-restoration, if there are teeth on the working side available to ‘pick up’ the guidance. If no such teeth are present, removal of the non-working side contacts is impossible and more time should be set aside to: copy the existing non-working side contacts; fabricate temporary restorations; fabricate the definitive restorations and check them at the time of fitting.
Reorganized Approach
Deflective contacts and occlusal interferences (contacts which inhibit a smooth movement of the mandible when carrying out excursive movements with the teeth in contact) are removed, allowing the muscles of mastication to move the mandible free from the proprioceptive influence of these contacts. The general sequence of treatment in a reorganized approach (Figs 10-3a, h) is:
1) Stabilize the jaw and posterior tooth relationships.
2) Check.
3) Determine the anterior guidance.
4) Check.
5) Restore the anterior teeth.
6) Check.
7) Restore the posterior teeth.
Fig. 10-3 Reorganized approach – all posterior teeth and the maxillary anteriors to be restored.
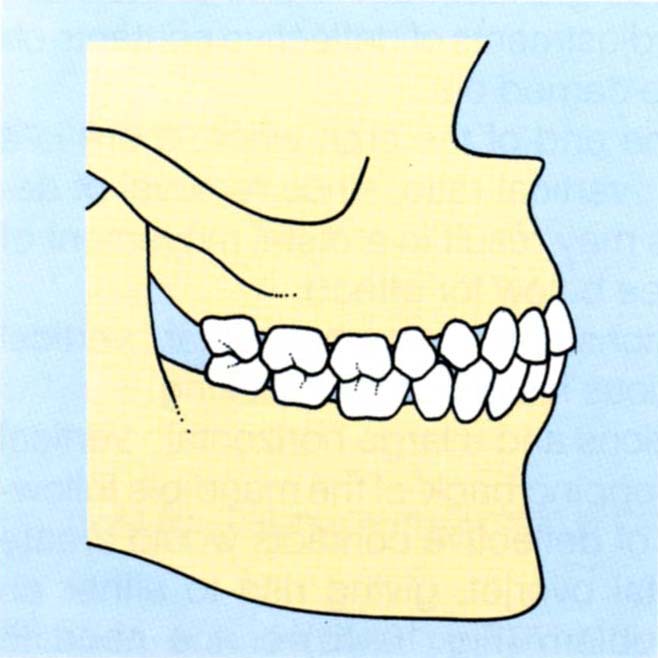
Fig. 10-3a The intercuspal position.
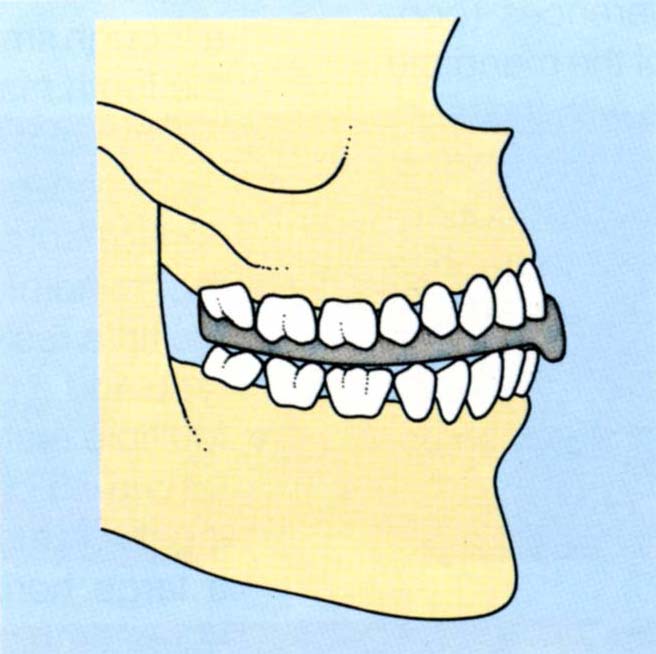
Fig. 10-3b Occlusal stabilization appliance fitted.
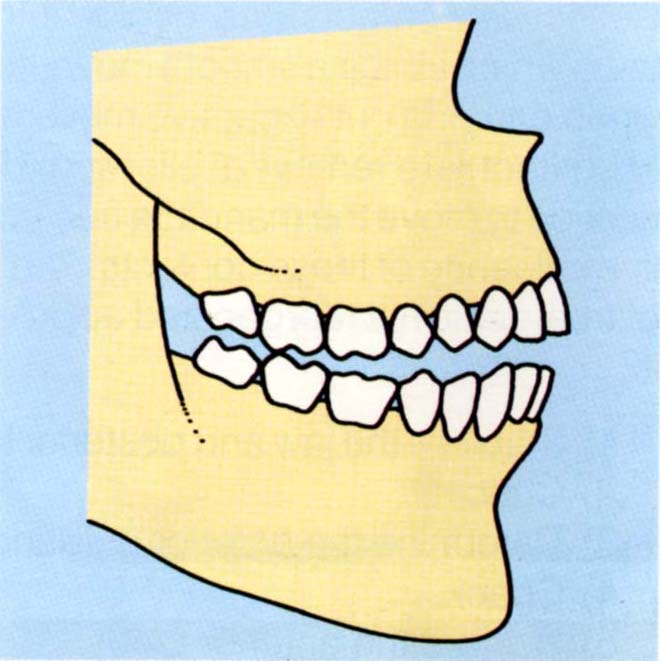
Fig. 10-3c The mandible moves distally and the condyle distally and superiorly. Small movements can introduce large defective contacts. Removal of the appliance reveals deflective contacts.
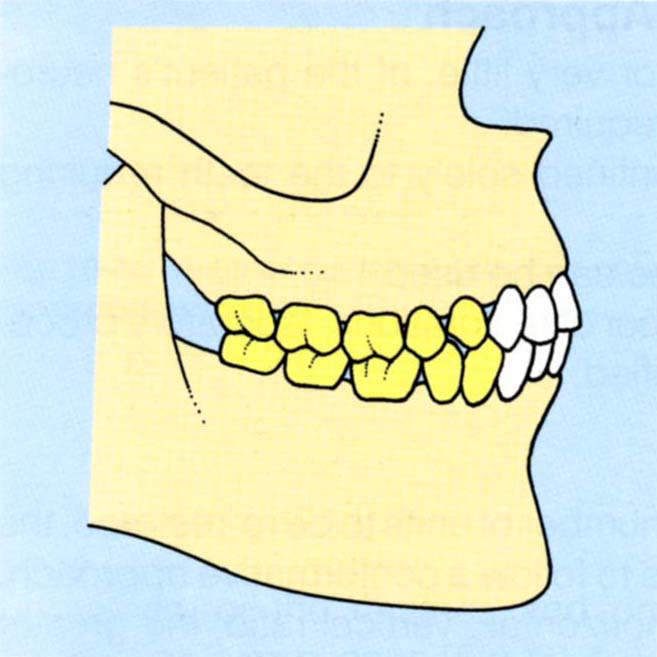
Fig. 10-3d The occlusion is equilibrated and the patient checked for comfort. The posterior teeth are prepared and provided with temporary restorations followed by provisional restorations (yellow) to stabilize tooth to tooth and mandibulo/maxillary relationships.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


