Structure of the Oral Tissues
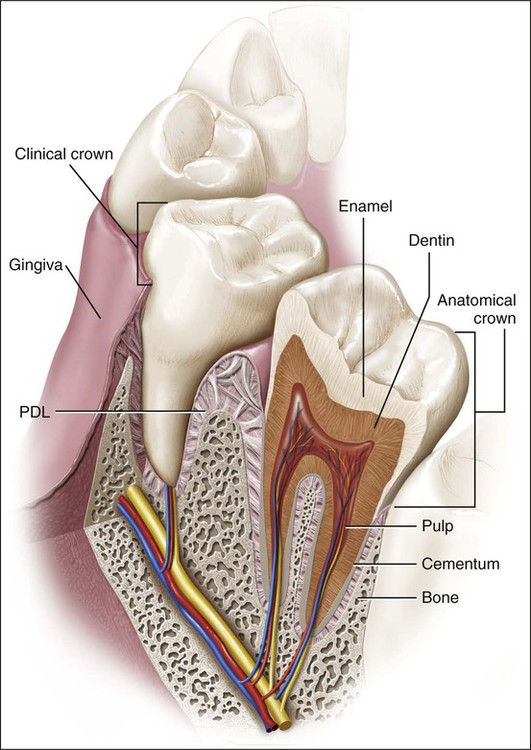
This chapter presents an overview of the histology of the tooth and its supporting tissues (Figure 1-1), setting the stage for more subsequent detailed consideration. The salivary glands, the bones of the jaw, and the articulations between the jaws (temporomandibular joints) also are discussed.
The Tooth
The tooth proper consists of a hard, inert, acellular enamel formed by epithelial cells and supported by the less mineralized, more resilient, and vital hard connective tissue dentin, which is formed and supported by the dental pulp, a soft connective tissue (Figures 1-1 and 1-2). In mammals, teeth are attached to the bones of the jaw by tooth-supporting connective tissues, consisting of the cementum, periodontal ligament (PDL), and alveolar bone, which provide an attachment with enough flexibility to withstand the forces of mastication. In human beings and most mammals, a limited succession of teeth still occurs, not to compensate for continual loss of teeth but to accommodate the growth of the face and jaws. The face and jaws of a human child are small and consequently can carry few teeth of smaller size. These smaller teeth constitute the deciduous or primary dentition. A large increase in the size of the jaws occurs with growth, necessitating not only more teeth but also larger ones. Because the size of teeth cannot increase after they are formed, the deciduous dentition becomes inadequate and must be replaced by a permanent or secondary dentition consisting of more and larger teeth.
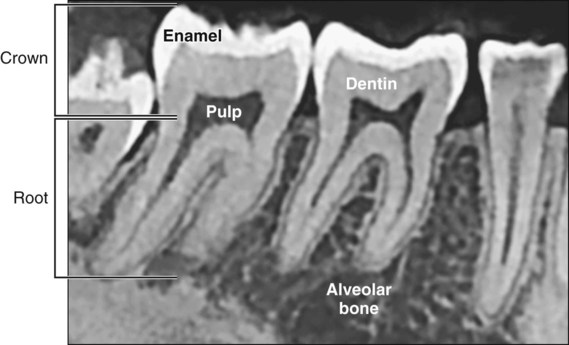
Anatomically the tooth consists of a crown and a root (see Figures 1-1 and 1-2); the junction between the two is the cervical margin. The term clinical crown denotes that part of the tooth that is visible in the oral cavity. Although teeth vary considerably in shape and size (e.g., an incisor compared with a molar), histologically they are similar.
Enamel
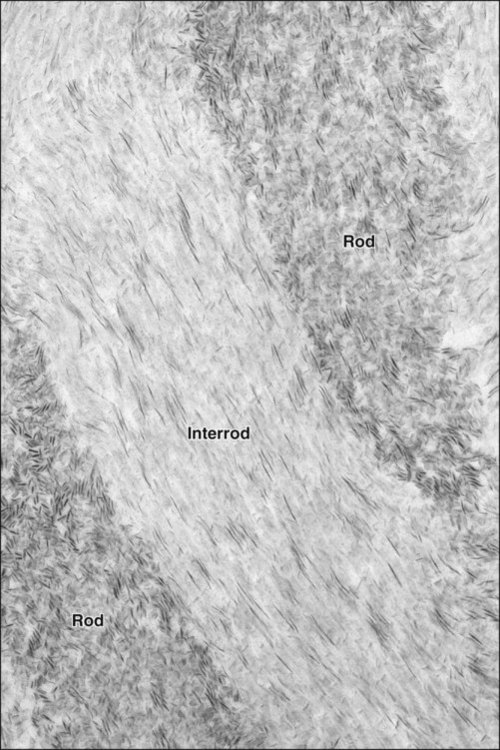
Enamel has evolved as an epithelially derived protective covering for the crown of the teeth (Figures 1-1 and 1-2). The enamel is the most highly mineralized tissue in the body, consisting of more than 96% inorganic material in the form of apatite crystals and traces of organic material. The cells responsible for the formation of enamel, the ameloblasts, cover the entire surface of the layer as it forms but are lost as the tooth emerges into the oral cavity. The loss of these cells renders enamel a nonvital and insensitive matrix that, when destroyed by any means (usually wear or caries), cannot be replaced or regenerated. To compensate for this inherent limitation, enamel has acquired a high degree of mineralization and a complex organization. These structural and compositional features allow enamel to withstand large masticatory forces and continual assaults by acids from food and bacterial sources. The apatite crystals within enamel pack together differentially to create a structure of enamel rods separated by an interrod enamel (Figure 1-3). Although enamel is a dead tissue in a strict biologic sense, it is permeable; ionic exchange can occur between the enamel and the environment of the oral cavity, in particular the saliva.
Dentin
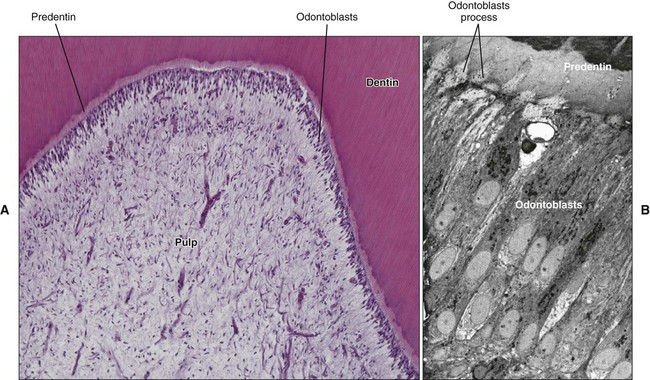
Dentin is a mineralized, elastic, yellowish-white, avascular tissue enclosing the central pulp chamber (Figure 1-4; see also Figures 1-1 and 1-2). The mineral is also apatite, and the organic component is mainly the fibrillar protein collagen. A characteristic feature of dentin is its permeation by closely packed tubules traversing its entire thickness and containing the cytoplasmic extensions of the cells that once formed it and later maintain it (Figure 1-4, B). These cells are called odontoblasts; their cell bodies are aligned along the inner edge of the dentin, where they form the peripheral boundary of the dental pulp (Figure 1-4, A). The very existence of odontoblasts makes dentin a vastly different tissue from enamel. Dentin is a sensitive tissue, and more importantly, it is capable of repair, because odontoblasts or cells in the pulp can be stimulated to deposit more dentin as the occasion demands.
Pulp
The central pulp chamber, enclosed by dentin, is filled with a soft connective tissue called pulp (Figure 1-4, A). Histologically, it is the practice to distinguish between dentin and pulp. Dentin is a hard tissue; the pulp is soft (and is lost in dried teeth, leaving a clearly recognizable empty chamber; see Figure 1-2, A). Embryologically and functionally, however, dentin and pulp are related and should be considered together. This unity is exemplified by the classic functions of pulp: it is (1) formative, in that it produces the dentin that surrounds it; (2) nutritive, in that it nourishes the avascular dentin; (3) protective, in that it carries nerves that give dentin its sensitivity; and (4) reparative, in that it is capable of producing new dentin when required.
Supporting Tissues of the Tooth
The tooth is attached to the jaw by a specialized supporting apparatus that consists of the alveolar bone, the PDL, and the cementum, all of which are protected by the gingiva (see Figure 1-1).
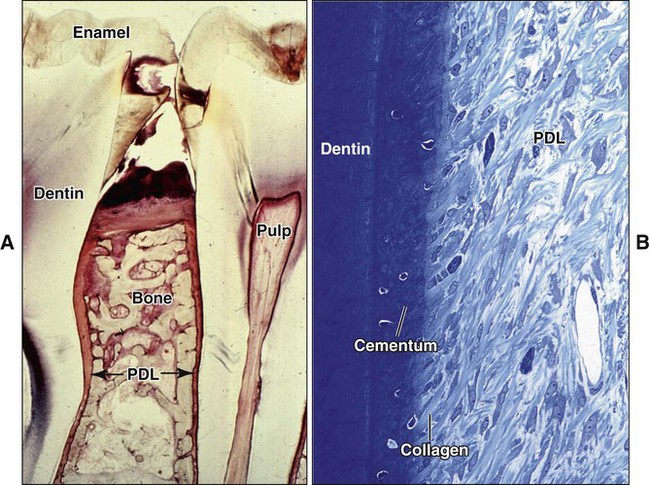
Periodontal Ligament
The PDL is a highly specialized connective tissue situated between the tooth and the alveolar bone (Figure 1-5). The principal function of the PDL is to connect the tooth to the jaw, which it must do in such a way that the tooth will withstand the considerable forces of mastication. This requirement is met by the masses of collagen fiber bundles that span the distance between the bone and the tooth and by ground substance between them. At one extremity the fibers of the PDL are embedded in bone; at the other extremity the collagen fiber bundles are embedded in cementum. Each collagen fiber bundle is much like a spliced rope in which individual strands can be remodeled continually without the overall fiber losing its architecture and function. In this way the collagen fiber bundles can adapt to the stresses placed on them. The PDL has another important function, a sensory one. Tooth enamel is an inert tissue and therefore insensitive, yet the moment teeth come into contact with each other, we know it. Part of this sense of discrimination is provided by sensory receptors within the PDL.
Cementum
Cementum covers the roots of the teeth and is interlocked firmly with the dentin of the root (see Figures 1-1, 1-2, and 1-5, B). Cementum is a mineralized connective tissue similar to bone except that it is avascular; the mineral is also apatite, and the organic matrix is largely collagen. The cells that form cementum are called cementoblasts.
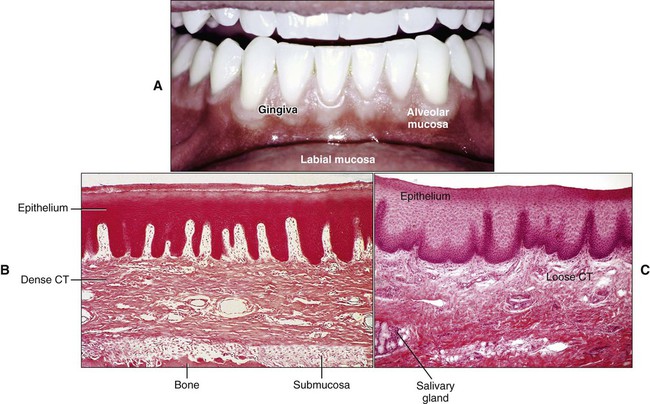
Oral Mucosa
The oral cavity is lined by a mucous membrane that consists of two layers: an epithelium and subjacent connective tissue (the lamina propria; Figure 1-6). Although its major functions are lining and protecting, the mucosa also is modified to serve as an exceptionally mobile tissue that permits free movement of the lip and cheek muscles. In other locations it serves as the organ of taste.
Histologically, the oral mucosa can be classified in three types: (1) masticatory, (2) lining, and (3) specialized. The masticatory mucosa covers the gingiva and hard palate. The masticatory mucosa is bound down tightly by the lamina propria to the underlying bone (Figure 1-6, B), and the covering epithelium is keratinized to withstand the constant pounding of the food bolus during mastication. The lining mucosa, by contrast, must be as flexible as possible to perform its function of protection. The epithelium is not keratinized; the lamina propria is structured for mobility and is not tightly bound to underlying structures (Figure 1-6, C). The dorsal surface of the tongue is covered by a specialized mucosa consisting of a highly extensible masticatory mucosa containing papillae and taste buds.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses