Chapter 6
Vital pulp therapy for primary molars
Jane A. Soxman
The goal of vital pulp therapy is to remove the infected coronal pulp tissue while preserving the healthy radicular pulp. Vital pulp therapy is recommended in primary molars with extensive caries, complaint of unprovoked spontaneous pain, and with carious or mechanical pulp exposure during caries excavation. Vital pulp therapy is contraindicated with radicular pathology, a sinus tract due to abscess, excessive mobility, presence of purulent material or necrosis in the coronal pulp chamber, or inability to obtain complete hemostasis when performing the pulp therapy (American Academy of Pediatric Dentistry, 2014; Winters et al., 2008). The use of a model to describe the pulpotomy procedure to a parent/guardian when obtaining informed consent for the procedure is helpful. Informed consent should include the need for local anesthesia, rubber dam, and a full-coverage crown (Kilgore International) (Figure 6.1a, b).
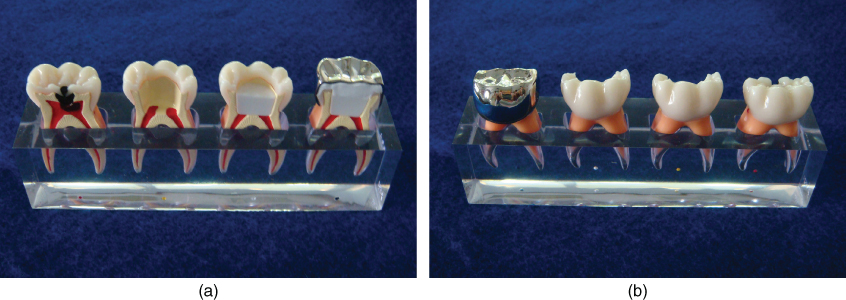
Figure 6.1 (a, b) Pulpotomy and stainless steel crown model viewed from different sides.
Radiographic evaluation
A periapical radiograph should be obtained before performing vital pulp therapy to confirm the health of the radicular pulp, internal or external root resorption, and evaluate caries progression if a period has elapsed since the initial treatment plan (Figure 6.2a). Internal resorption is always associated with extensive inflammation in the primary dentition. The roots of the primary molar are very thin; if internal resorption can be seen on a radiograph, a perforation has usually occurred, and extraction is indicated. The same criteria apply for external resorption (Camp, 2011) (Figure 6.2b).
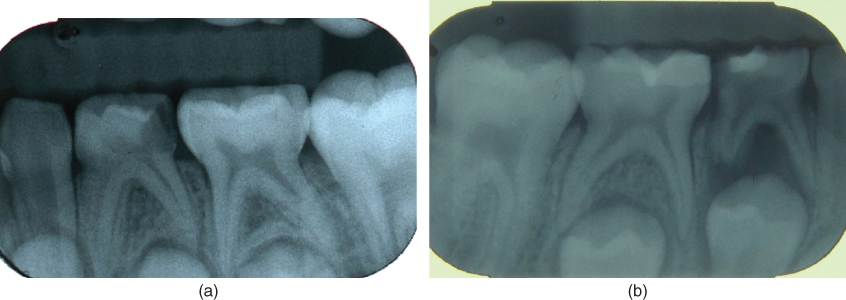
Figure 6.2 (a) Periapical radiograph of mandibular left first primary molar with carious pulpal involvement. (b) Periapical radiograph with internal and external root resorption.
Local anesthesia
Local anesthesia with infiltration in the maxilla and inferior alveolar nerve (IAN) block in the mandible should be administered. In some cases, buccal infiltration alone may provide adequate anesthesia in the mandible, but if a child is crying from the outset, IAN should be performed. If the child appears to be comfortable, with no complaint of pain until the pulp chamber is uncovered, providing immediate additional local anesthesia is indicated. If the discomfort is minimal, a few drops of 2% xylocaine with 1 : 100,000 epinephrine dispensed into the coronal chamber provides adequate anesthesia to continue the procedure without another injection.
Rubber dam isolation
The rubber dam should be routinely used when performing vital pulp therapy. The rubber dam provides a throat partition and protects the oral tissues from exposure to medicaments or injury with the bur or instruments. Multiple colors, nonlatex, and varying thicknesses in 5 × 5 in.2 pediatric size are available. The use of a thicker gage rubber dam may provide a better seal around the clamp and improved retraction of the surrounding oral tissues. The rubber dam clamp should be ligated with floss to facilitate retrieval should the clamp become dislodged before or during placement of the rubber dam. The W8A rubber dam clamp is typically an ideal fit for a second primary molar (Figure 6.3). If there is difficulty placing the rubber dam over the clamp intraorally, a winged clamp may be used. The rubber dam is placed on the clamp extraorally and then placed on the molar as a single unit with the rubber dam forceps (Figure 6.4a and 6.4b). The portion of the rubber dam covering the wings of the clamp is slipped off with an instrument and tucked beneath the wings for good moisture control (Figure 6.4c). Because the tooth is anesthetized, the rubber dam may be referred to as a blanket, to cover the sleeping tooth, when performing “Tell–Show–Do” with a young child. The slit technique may be used to restore a quadrant (Figure 6.5).
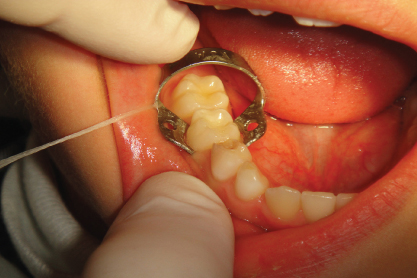
Figure 6.3 W8A rubber dam clamp ligated with floss.
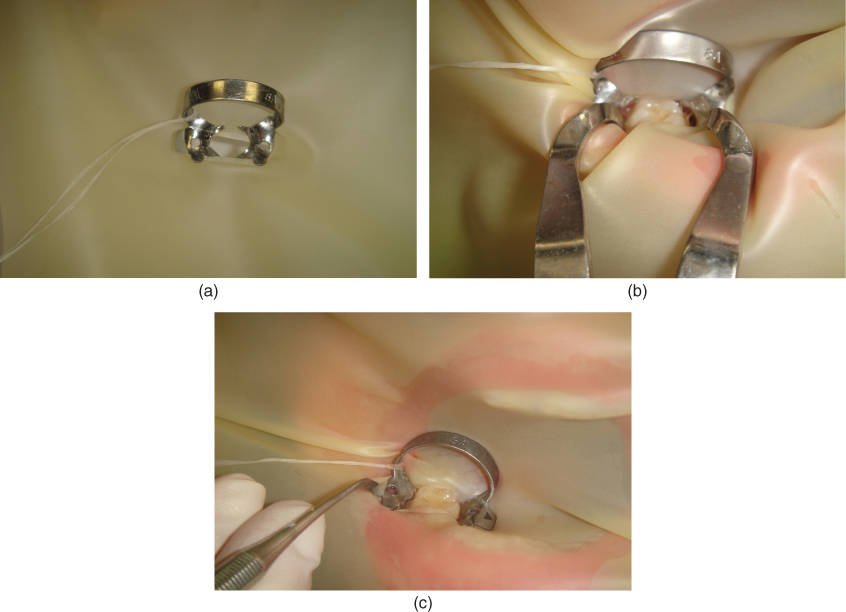
Figure 6.4 (a) Rubber dam placed on winged clamp extraorally. (b) Rubber dam and winged clamp placed intraorally as a unit. (c) Removing rubber dam from wings of clamp.
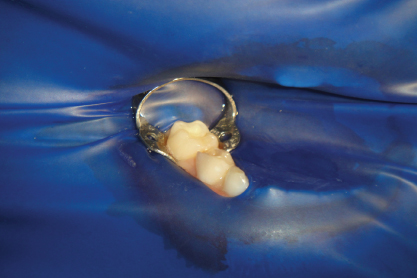
Figure 6.5 Slit technique for rubber dam with floss ligated to clamp under rubber dam.
Procedure
Complete caries removal is recommended before entering the coronal pulp. By removing the peripheral caries and prepping from the periphery toward the pulp chamber, the infected tissues will not further contaminate the coronal pulp (Winters et al., 2008).
A full-coverage crown is the restoration of choice. Occlusal reduction recommended for the type of crown selected (stainless steel, zirconia, or preveneered) is performed before unroofing the coronal pulp (Figure 6.6).
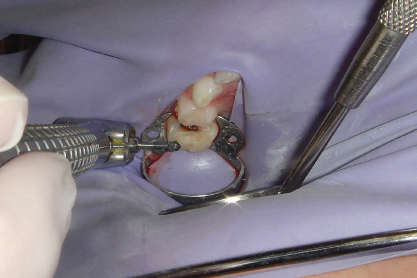
Figure 6.6 Occlusal reduction with large round bur.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


