Vertical Root Fractures
Introduction
Vertical root fracture (VRF) is a term used to describe longitudinally orientated cracks or fractures originating within the tooth root. The fracture may involve proximal and/or aproximal surfaces (Pitts and Natkin, 1983; Colleagues for Excellence; American Association of Endodontists, 2008). Although VRFs are more commonly associated with endodontically treated teeth (Llena-Puy et al, 2001), they can also occur in non-endodontically treated teeth (Zadik et al, 2008; Chen et al, 2008).
An incomplete VRF may be defined as a longitudinal fracture line where there has been no separation of the root fragments; generally, these VRFs have not extended to form a communication between the root canal and the periodontal ligament. Whereas with complete VRFs the root fragments are separable (Rivera and Walton, 2007; Brady et al, 2014). By its very nature, an incomplete VRF will have a narrower width compared to a complete VRF. The prognosis of a tooth with a complete VRF is generally very poor (Zadik et al, 2008).
The prevalence of VRF is more commonly reported in endodontically treated teeth than in vital teeth (Chan et al, 1999; Cohen et al, 2003). Between 20% and 32% of endodontically treated teeth are extracted due to VRFs (Caplan and Weintraub, 1997; Chen et al, 2008).
In some instances, a diagnosis of VRF may be confirmed clinically with the aid of a dental operating microscope; for example, a complete VRF running along the pulp chamber floor, or externally on the buccal/lingual root surface. However, it is not uncommon for the diagnosis to be more challenging, especially with incomplete VRFs (Cohen et al, 2003; Chavda et al, 2014). Incorrect diagnosis may lead to inappropriate management. A recent systematic review concluded that there was a lack of evidence-based data regarding the diagnostic accuracy of commonly used clinical and conventional radiographic examinations for detecting VRFs (Tsesis et al, 2010).
Early diagnosis of VRF is essential to allow the appropriate management of the affected tooth, and ideally improve its prognosis.
Conventional radiography
Currently, periapical radiography is the imaging system of choice for assessing teeth with suspected VRFs (Junqueira et al, 2013; Bechara et al, 2013). However, due to the limitations of conventional radiographic imaging, periapical radiography will only detect a VRF if the root fragments are displaced (complete VRF) (Meister et al, 1980), and the X-ray beam passes through the fracture line (Rud and Omnell, 1970; Kambungton et al, 2012). With an extensive VRF, there may be complete separation of the fractured root fragments (Pitts and Natkin, 1983; Moule and Kahler, 1999), which may be detected radiographically (Fig 11-1).
The radiographic appearance of a VRF is dependent on the position of the fracture within the root and the degree of displacement of the fracture. The narrower the fracture line, the less likely it is to be detected (Meister et al, 1980; Brady et al, 2014). Even with the aid of parallax radiographs, complete and incomplete VRFs with minimal displacement are not readily identifiable in either endodontically treated (Patel et al, 2013) or non-endodontically treated teeth (Brady et al, 2014). The overall accuracy of both digital (solid-state and phosphor plate) and conventional radiographs in detecting VRFs is similar. There is a higher accuracy in unfilled root canals but the presence of radiodense gutta-percha and/or metal posts reduces the diagnostic accuracy of periapical radiographs (Nascimento et al, 2015a).
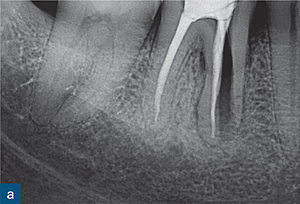
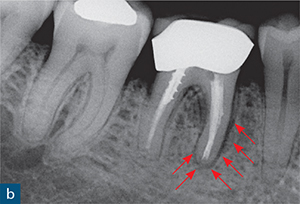
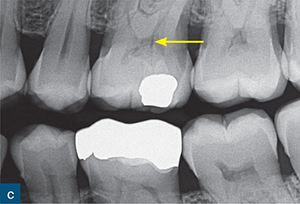
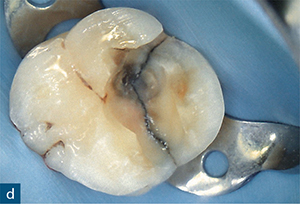
Fig 11-1 (a) Periapical radiograph of a root filled mandibular first molar. A complete separation of the mesial root indicates a complete VRF. (b) Periapical radiograph of a symptomatic root filled mandibular molar with a ‘J’-shaped radiolucency (red arrows). (c) A bitewing radiograph reveals signs of a fracture (yellow arrow), which is confirmed clinically (d).
Table 11-1 Radiographic features suggestive of vertical root fractures.
 Visible separation of root
Visible separation of root
 Isolated angular bone loss at crestal level
Isolated angular bone loss at crestal level
 Widening of periodontal ligament space on one or more aspects of root
Widening of periodontal ligament space on one or more aspects of root
 ‘J’-shaped periradicular radiolucency
‘J’-shaped periradicular radiolucency
 Periradicular radiolucency in furcation region
Periradicular radiolucency in furcation region
 Floating retrograde root end root filling
Floating retrograde root end root filling
 Sinus tract pointing to root apex
Sinus tract pointing to root apex
Conventional radiographic systems have high specificity but low sensitivity in the detection of VRFs ex vivo (Tsesis et al, 2008; Patel et al, 2013). The specific type of image receptor used (plain film versus digital receptors) appears to have no significant effect on the diagnostic accuracy of periapical radiography in the detection of artificially created VRFs in single-rooted teeth (Tsesis et al, 2008; Tofangchiha et al, 2011). In contrast, one study suggested that, in multirooted teeth, digital sensors produce more diagnostically accurate images in the detection of VRFs compared to plain film radiographs (Kondylidou-Sidira et al, 2013).
Basic digital manipulation of the radiographic images (e.g. zooming in, colourising, and inverting) has been shown to improve the detection of simulated VRFs in non-root filled teeth when compared to the raw image (Nascimento et al, 2015b). However, similar image manipulation has no significant effect on diagnostic yield in root filled teeth (Kositbowornchai et al, 2001; Kamburoğlu et al, 2010; Tofangchiha et al, 2011).
It has been reported that ‘floating’ retrograde root end fillings that are no longer seated within the root end may be a sign of a VRF (Pitts and Natkin, 1983). However, this is more likely to occur with amalgam retrograde root end fillings than with more contemporary materials, such as mineral trioxide aggregate (MTA) and biodentine.
Although the identification of a VRF within the root is challenging, certain features in the adjacent periradicular bone may indicate a VRF (Table 11-1). These include: localised angular bone loss at the crestal level (Testori et al, 1993; Nicopoulou-Karayianni et al, 1997; Tamse et al, 1999; Lustig et al, 2000); an extensive periradicular radiolucency, also known as a ‘halo’- or ‘J’-shaped periradicular radiolucency (Tsesis et al, 2010) (Figs 11-2 and 11-3); an isolated radiolucency in the furcation region of molar teeth; thickening of the periodontal ligament space on one aspect of the root or a sinus tract (Figs 11-3 and 11-4), which can be traced radiographically to the VRF (Tamse et al, 2006).
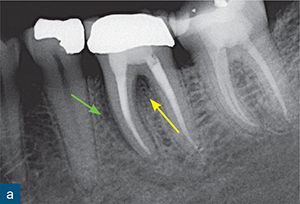
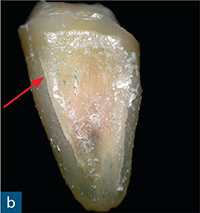
Fig 11-2 (a) Periapical radiograph of a root filled mandibular molar with a subtle radiolucency running along the mesial aspect of the mesial root (green arrow), and a radiolucency in the furcation region (yellow arrow); note a VRF cannot be seen within the root. (b) The extracted root with an incomplete VRF (red arrow).
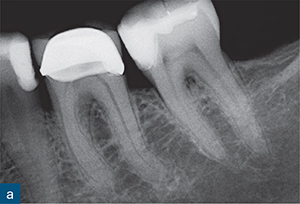
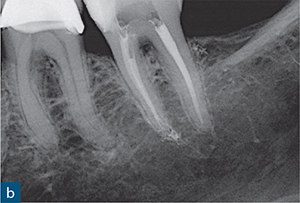
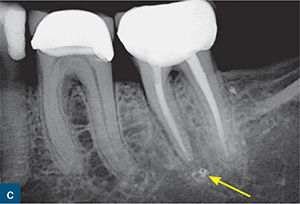
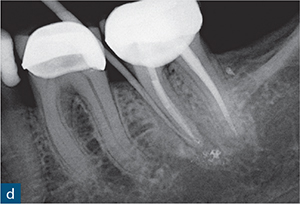
Fig 11-3 (a) Diagnostic radiograph and (b) post-obturation radiograph of a root-treated mandibular second molar; note that the periapical tissues appear to be healthy. (c) At 3 years post-treatment, the patient presents with low-grade pain localised to this tooth; the periapical radiograph reveals widening along the mesial aspect of the mesial root and an associated periapical radiolucency (yellow arrow). (d) An isolated probing depth on the mesial aspect of the tooth is tracked with a gutta-percha point.
Cone beam computed tomography
There are conflicting results on the overall diagnostic accuracy of cone beam computed tomography (CBCT) when used to detect VRF (Hassan et al, 2010; Fayad et al, 2012; Neves et al, 2014).
Ex vivo studies
Ex vivo studies have demonstrated that CBCT is more accurate than periapical radiography in the detection of VRF in extracted human teeth (Hassan et al, 2009, 2010; Özer 2010; Özer et al 2011; Kamboroğlu et al, 2010). However, the diagnostic accuracy of CBCT may have been higher in these studies due to the size of the artificially created fractures (complete fractures), which were wider and more easily identifiable than clinically occurring, incomplete fractures. In a clinical situation, it has been suggested that these simulated complete VRFs would be detected clinically, and therefore a CBCT scan would not be required to confirm the diagnosis (Patel et al, 2013).
A recent series of ex vivo studies compared the diagnostic accuracy of CBCT and conventional radiographs for detecting incomplete and complete VRFs with a predetermined range of widths (Patel et al, 2013; Brady et al, 2014). The fractures created in these two studies were up to four times narrower than in the study conducted by Özer (2011). The overall sensitivity of periapical radiography and CBCT in the detection of VRFs (regardless of the fracture dimensions) in teeth without root fillings was 0.63 and 0.87, respectively, while in root filled teeth it was 0.45 and 0.53, respectively. The presence of a root-filling material resulted in a reduction of specificity in both imaging techniques (Patel et al, 2013). Furthermore, Brady et al (2014) found that CBCT was more accurate than parallax periapical radiography for detecting incomplete VRFs in non-endodontically treated teeth.

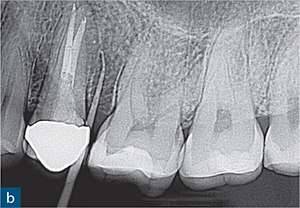
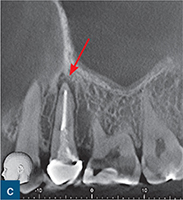

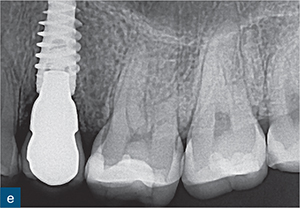
Fig 11-4 (a) Periapical radiograph of a symptomatic root filled mandibular second premolar; (b) with a gutta-percha point tracking the buccal sinus. There are no abnormal signs on either radiograph. (c and d) Reconstructed CBCT sagittal images reveal a well-defined periapical radiolucency (red arrow), and distinct widening of the periodontal ligament (yellow arrow) on the distal aspect of the root. (e) This tooth was subsequently extracted and replaced with an implant-retained crown. (Implant placement by Dr Fiona Mackillop.)
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


