Chapter 7
Apical Periodontitis
Introduction
Apical periodontitis (AP) is an acute or chronic inflammatory condition occurring around the root of a tooth. It is caused by microbial infection of the root canal space and is characterised by destruction of the periradicular bone (Huumonen and Ørstavik, 2002). Prevalence studies on AP show that, depending on the age and location of the population, up to 80% of individuals may be affected with AP when conventional radiography is used to assess the periapical status of their teeth (Kabak and Abbott, 2005). While acute AP is commonly diagnosed from its clinical presentation, the diagnosis of chronic AP is usually dependent on the presence of radiographic signs of the disease.
The ability of radiographs to accurately detect signs of AP is essential for diagnosis, treatment planning, assessment of outcome, and epidemiological studies. Currently, the accepted reference standard for the radiological detection of AP is periapical radiography (European Society of Endodontology, quality guidelines, 2006). However, several studies have highlighted the limitations of conventional radiography for detecting AP (Bender and Seltzer, 1961a; Patel et al, 2009; Tsai et al, 2013).
Limitations of conventional periapical radiography
In a series of ex vivo investigations, Bender and Seltzer (1961a, b) concluded that simulated AP lesions confined to the cancellous bone could not be readily identified on radiographs (Fig 7-1). This was due to the lesions being masked by the overlying denser cortical bone (i.e. anatomical noise); other research groups reported similar results (Pauls and Trott, 1966; Schwartz and Foster, 1971). However, in a post-mortem study using human specimens, Brynolf (1967) found that AP confined to the cancellous bone in the anterior maxilla region could be detected using periapical radiographs. In some instances, it may be possible to detect destruction within the cancellous bone without associated loss of cortical or junctional bone (Shoha et al, 1974).
For AP to be detected radiographically, the bone loss has to reach a ‘critical threshold’ in relation to the surrounding bone. If the ratio of healthy (mineralised) bone to demineralised bone (i.e. AP) reaches this critical level, then AP will be detected. The ratio will depend on several factors, including: the density of the bone; the nature of cancellous and cortical bone; the X-ray beam angulation; the exposure parameters; and the nature of the lesion (i.e. size and degree of demineralisation). These factors not only vary depending on the position of the lesion within the jaw, but also between the maxilla and mandible, as well as between individuals. For example, the mineral density of the posterior mandible region is higher than the anterior maxilla region. Therefore, a small volume of demineralised bone may be readily identifiable in the anterior maxilla, but not in the more radiodense posterior mandible.
A second angled (parallax) radiograph has been suggested to improve the ability to diagnose periapical lesions (European Society of Endodontology, quality guidelines, 2006; Vertucci and Haddix, 2010). However, there is limited evidence that parallax radiographs do improve the detection of periapical lesions (Soğur et al, 2012). Recently, Davies et al (2015a) compared the ability of single radiographs, two parallax radiographs, and cone beam computed tomography (CBCT) to detect AP in vivo, and revealed periapical lesions in 41%, 38% and 68% of radiographic systems, respectively. Using CBCT as a reference standard, these results suggest that there is no increased accuracy in detecting AP with parallax radiographs compared to a single view. However, Kangasingam et al (2016a) found that the combination of two additional (parallax) images, with mesial and distal horizontal angulations, did improve the detection of AP lesions when compared to a single view. In this study, block dissection and histopathological analysis of the periapical tissues in relatively fresh (unpreserved) human cadavers was used as the reference standard (Figs 7-1 and 7-2).
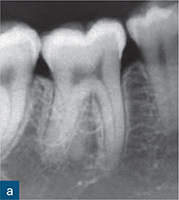

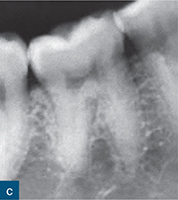




Fig 7-1 Despite the use of parallax radiographs, AP is not readily identifiable regardless of whether a film or digital radiographic system is used. (a) Conventional film-centred view; (b) mesial shift (-10 degrees); (c) distal shift (+10 degrees), as well as (d) digital imaging system centred view; (e) mesial shift and (f) distal shift. None of these images detected an existing periapical lesion associated with the distal root. Histopathological examination of the same distal root (g) showed AP: decalcified root structure with necrotic apical pulp and granulomatous tissues (magnification 4×; H&E staining). Yellow arrow showing area of inflammation with bone resorption, GT = granulomatous tissue, D = dentine, PDL = periodontal ligament (Kanagasingham et al [2016a], submitted for publication, Int Endod J).
With digital periapical radiographic systems, the image produced is dynamic and can therefore be enhanced (contrast/brightness) to potentially improve its diagnostic yield (Kullendorff et al, 1996). Several well-designed ex vivo studies have shown that there is no difference in the ability to detect artificially created periapical lesions using conventional radiographic films and digital sensors (Kullendorff and Nilsson, 1996; Stavropoulos and Wenzel, 2007; Özen et al, 2009). In the abovementioned autopsy study using human cadavers, Kangasingam et al (2016a) also found no statistical difference between the accuracy of parallax digital and conventional (film) periapical radiographs, for assessing AP. However, single digital periapical radiographs were found to be more accurate than single conventional radiographs.
‘Enhancing’ radiographic images (e.g. colourising and inverting) with software also does not appear to improve the detection of periapical lesions (Barbat and Messer, 1998).
Detection of apical periodontitis
Numerous ex vivo studies with reference standards in both animal (Stavropoulos and Wenzel, 2007) and human (Özen et al, 2009; Patel et al, 2009; Tsai et al, 2013) models have conclusively demonstrated that CBCT is a significantly more accurate imaging system than periapical radiography for detecting the presence (sensitivity) of artificially created bone lesions. All ex vivo studies have the disadvantage of not truly mimicking the ‘real-life’ clinical situation. However, the advantage of such studies is that standardised periapical defects have been intentionally created, thus giving a reference standard that allows imaging techniques to be assessed with more confidence (Fig 7-3).



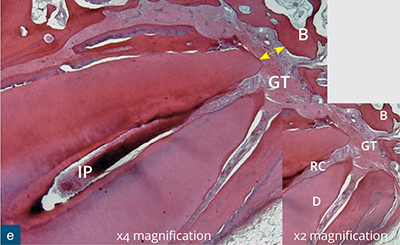
Fig 7-2 Digital periapical radiographs, centred view (a), mesial shift (b) and distal shift (c) do not detect any periapical lesion associated with the maxillary right first premolar. Coronal (d) reconstructed CBCT images shows a periapical radiolucency associated with the buccal (yellow arrow) root. (e) Diagnosis of apical periodontitis (AP) was confirmed from the histopathological examination. The histopathological examination of the specimen with X2 magnification; H&E staining showing: Highly inflammed pulp with granulation tissue at apical area (Kanagasingham et al (2016b) submitted for publication, Int Endod J).

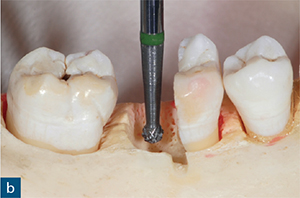
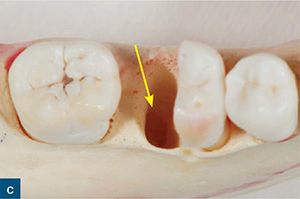

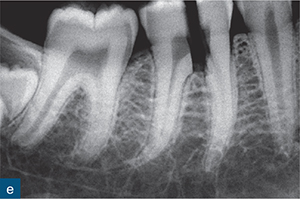

Fig 7-3 (a) A dry human mandible model used to simulate periapical lesion. (b) The distal root of the mandibular first molar has been sectioned; and (c) atraumatically extracted to allow a standardised simulated periapical lesion (yellow arrow) to be created within the cancellous bone with a laboratory bur and handpiece. (d) The distal root has been re-seated. (e) The digital periapical radiograph does not reveal the presence of a 2-mm diameter periapical lesion within the cancellous bone. (f) A reconstructed sagittal CBCT image clearly reveals the simulated periapical lesion (yellow arrows) on the distal root.
Using similar methodology to Brynolf (1967), Kanagasingam et al (2016b) assessed the accuracy of single, parallax digital radiographs and CBCT for diagnosing AP in fresh human cadavers using histology as the reference standard. In total, 86 teeth were assessed (Fig 7-2). The specificity of all the imaging systems was excellent, i.e. all imaging techniques could correctly detect healthy periapical tissues. However, the sensitivity of digital radiographs varied from 0.27 to 0.38, depending on whether a single view or parallax views, respectively, were assessed. This compared to a sensitivity of 0.89 for CBCT. The overall accuracy of the digital radiographic techniques was 0.5 for a single view and 0.58 for parallax views, and there was a significantly higher accuracy (0.92) for CBCT.
Several clinical studies have concluded that the diagnostic accuracy of CBCT in the detection of AP is superior to that of periapical radiography (Low et al, 2008; Patel et al, 2012a). Lofthag-Hansen et al (2007) examined and compared the periapical status of teeth with suspected endodontic disease using CBCT and periapical radiography. The authors reported that 38% more periapical lesions were detected with CBCT. Subsequent studies have reported similar findings (Bornstein et al, 2011; Abella et al, 2012). Patel et al (2012a) compared the prevalence of AP lesions associated with the roots of teeth with primary endodontic disease. CBCT was able to identify lesions of AP in 28% more teeth than periapical radiographs (Fig 7-4). Similar findings have been reported for endodontically treated teeth (Davies et al, 2015a).
Assessment of the outcome of endodontic treatment
It follows that the superior diagnostic accuracy of CBCT over conventional radiography in the detection of AP permits a more accurate and objective assessment of the outcome of endodontic treatment. Liang et al (2011) compared the outcome of endodontic treatment using periapical radiographs and CBCT 2 years after treatment. They found that a favourable outcome was reached in 87% of cases assessed with periapical radiographs, compared to only 74% of cases assessed with CBCT; the 13% difference being attributed to the superior sensitivity of CBCT in detecting AP. Patel et al (2012b) compared the outcome of primary endodontic treatment carried out on 132 teeth 1 year after treatment. The ‘healed’ rate (absence of radiolucency at review) of the treated teeth was 87% and 62.5% when assessed using periapical radiographs and CBCT, respectively. When more relaxed criteria (i.e. healing and healed) were used to assess outcome, the percentage of teeth demonstrating a reduction in the size of the associated apical radiolucency was 95.1% and 84.7% for conventional radiography and CBCT, respectively. Paula-Silva et al (2009b) assessed the outcome of root canal treatment in dogs and found a 44% lower success rate when the periapical tissues were assessed with CBCT (35%), compared with periapical radiographs (79%).
Davies et al (2015b) reviewed the outcome of secondary (re-treatment) carried out in 98 teeth 1 year after re-treatment with conventional radiographs and CBCT. They found that there was a significantly different success rate between radiographs (93%) and CBCT (77%).
Radiographic appearance of apical periodontitis
Conventional radiography
While long-standing lesions of AP with significant bone destruction are generally readily discernible on conventional radiographs, incipient lesions of AP are often much more difficult to identify. Alterations to structures of the apical periodontium, such as the medullary bone trabeculae, the periodontal ligament (PDL) space, and the lamina dura may be early indicators of AP (Gröndahl and Huumonen, 2004). As such, an appreciation of the normal radiographic appearance of these structures is essential.


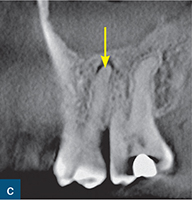
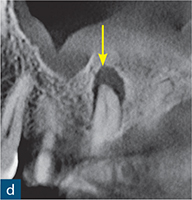
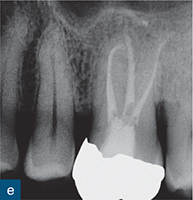

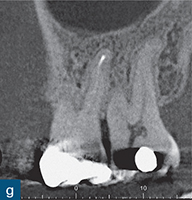
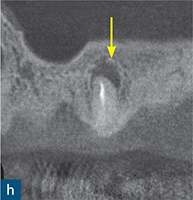
Fig 7-4 A 72-year-old male patient has symptoms of a poorly localised and intermittent dull ache associated with the maxillary left quadrant. Clinical examination is unremarkable, and all maxillary left premolar and molar teeth give a delayed response to sensitivity testing. (a) A periapical radiograph of the maxillary left quadrant reveals sclerosis of the root canals of the maxillary left premolar and molar teeth, although there are no radiographic signs of AP. A CBCT scan was taken to aid diagnosis, and reconstructed coronal images of the (b) mesiobuccal, (c) distobuccal, and (d) palatal canals clearly show signs of AP associated with the maxillary left first molar, while periapical tissues associated with the other teeth appeared normal. A diagnosis of chronic AP was made for this tooth; root canal treatment was carried out in a single visit. A 1-year follow-up radiograph (e) revealed healthy periapical tissues (no change from pre-treatment radiograph), while the 1-year follow-up reconstructed coronal CBCT images revealed complete healing of the pre-treatment periapical lesions on the (f) mesiobuccal and (g) distobuccal roots, and incomplete healing on the (h) palatal root.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



