Chapter 6
Assessment of Root Canal Anatomy
Introduction
Anatomical variations exist with each tooth type and may be a result of differences in ethnic background, age and gender of the population being investigated (Cleghorn et al, 2006). Variations in canal number, configuration, curvature, and presence of accessory roots may pose both diagnostic and clinical challenges (Kulild and Peters, 1990; Vertucci, 2005). An awareness and understanding of root canal anatomy is essential to facilitate endodontic risk assessment and treatment planning.
At present, conventional periapical radiography is regarded as the best clinical practice for preoperative assessment of root canal anatomy (European Society of Endodontology, 2006). However, two-dimensional imaging only permits visualisation of the dentition in the mesiodistal plane. The buccolingual plane (i.e. the third dimension) may not be fully appreciated (Patel, 2009). The diagnostic yield of conventional radiography may be improved by taking additional radiographic views with changes in horizontal angulation (parallax principle) (Vertucci, 2005; Davies et al, 2015). However, even parallax periapical radiographs do not always provide sufficient information on root canal anatomy (Khedmat et al, 2010; Soares de Toubes et al, 2012).
Cone beam computed tomography (CBCT) overcomes these limitations by enabling visualisation of the third dimension, while at the same time eliminating superimposition of overlying dentoalveolar anatomy. The information from a CBCT scan provides the clinician with a more in-depth understanding of the true morphology of root canal systems, including anatomic aberrations (Abella et al, 2011; Zhang et al, 2011). Several studies have concluded that CBCT increases the detection of root canals compared to single and parallax periapical radiography (Cheung et al, 2013; Davies et al, 2015). A recent study demonstrated that both charge-coupled devices (CCDs) and photostimulable phosphor (PSP) plates missed one or more root canals in 40% of anterior and posterior teeth when compared to CBCT (Matherne et al, 2008).
An in vitro study by Neelakantan et al (2010) concluded that CBCT analysis of the anatomy and morphology of root canal systems is as accurate as the modified canal staining and clearing technique. Michetti et al (2010) found that there is a high correlation between the information provided by CBCT image reconstructions and histologic examination, which was used as the reference standard.
CBCT has been reported to have comparable accuracy to microcomputed tomography in the analysis of internal and external root geometry (Domark et al, 2013; Paes da Silva Ramos Fernandes et al, 2014). Current evidence appears to validate the reliability and accuracy of CBCT as a tool to assess root canal anatomy.
Complex anatomy
Incisor and canine teeth
CBCT assessment of maxillary central and lateral incisors in a Turkish population reported the prevalence of a supplemental canal in between 0.3% and 3.2% of the study sample. In the same study maxillary canines were shown to have a second canal in 3% of male and 1% of female subjects (Altunsoy et al, 2014). This study also reported a significantly higher prevalence of two canals in maxillary anterior teeth in males.
Mandibular incisors have been shown to exhibit complex anatomy, with the incidence of a supplemental canal in these teeth reported to be as high as 40% (Benjamin and Dawson, 1974). Common variations include oval and flattened canals, which have been reported to be more difficult to disinfect and obturate (Wu et al, 2000). A recent study concluded that CBCT was significantly better than conventional radiography at identifying canals with oval-shaped cross-sections (Paes da Silva Ramos Fernandes et al, 2014).



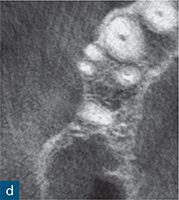
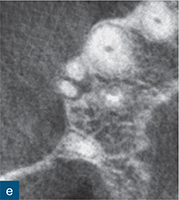
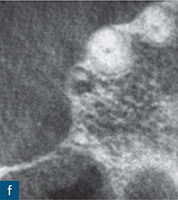



Fig 6-1 (a) Preoperative intraoral photograph of symptomatic right maxillary first premolar, which had been previously root canal treated. (b and c) Two periapical radiographs with differing horizontal beam angles showed that the buccal and palatal canals had been root filled. CBCT axial (d to f) and sagittal (g and h) views revealed the presence of an untreated third root, the mesiobuccal root, associated with a periapical lesion. The mesiobuccal canal was located, guided by the CBCT images. (i) Non-surgical root canal re-treatment was performed and all three canals were obturated to working length, verified by the postoperative periapical radiograph.
CBCT studies of mandibular incisor teeth in Chinese and Turkish populations found a higher incidence of a second canal in mandibular lateral incisors compared to central incisors and canines (Altunsoy et al, 2014; Lin et al, 2014; Han et al, 2014).
CBCT also revealed that many of these teeth exhibit bifurcations at the middle third root region (Lin et al, 2014).
Premolar teeth
The assessment of root morphology of maxillary first premolars using CBCT has revealed that the predominant form is a single root with two canals that exit the root apex separately. The next most prevalent configuration is two canals coronally, which join at the apex to form a single canal. The incidence of three roots or three canals is 1% (Tian et al, 2012) (Fig 6-1).
CBCT scans of mandibular first and second premolars showed that 100% and 99%, respectively, were single rooted (Park et al, 2013a). The reported prevalence of one, two and three root canals in mandibular premolar teeth was found to be 87%, 11.2% and 0%, respectively (Yu et al, 2012). An unusual C-shaped canal configuration was seen in 1% of the study sample. In contrast, the ability of conventional radiography to accurately assess the root canal anatomy and morphology of premolar teeth appears to be poor. Khedmat et al (2010) reported that periapical radiographs failed to identify more than 70% of premolar teeth with two or more root canals, compared to the reference standard of cross-sectioning the teeth. The authors found that additional buccolingual periapical views may not identify complex anatomy in mandibular premolars.
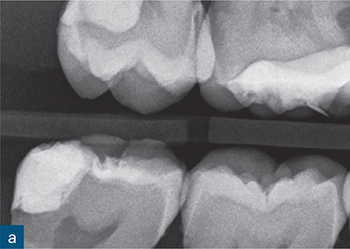
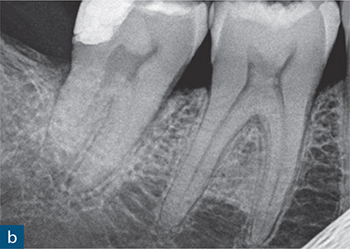
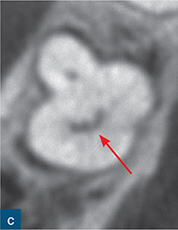


Fig 6-2 (a and b) Bitewing and periapical radiographs of the mandibular right second molar. Due to the buccolingual beam direction of the X-ray, no abnormal anatomy was detected, with the tooth exhibiting separate mesial and distal roots. (c and d) The axial CBCT views demonstrated a C-shaped cross-section as a result of incomplete fusion of the mesial and distal roots. (e) Post-obturation radiograph.
Molar teeth
The complexity of the root canal anatomy of maxillary molar teeth has been extensively reported (Kulild and Peters, 1990; Baratto Filho et al, 2009). Although in vitro studies have reported that more than 70% of maxillary first molars have a second mesiobuccal (MB2) canal (Görduysus et al, 2001; Barton et al, 2003), parallax periapical radiography has been shown to be unreliable in detecting additional canals in maxillary molar teeth (Barton et al, 2003; Davies et al, 2015). In contrast, the use of CBCT resulted in the detection of more MB2 canals, with reported incidence as high as 91% (Kim et al, 2012; Reis et al, 2013). Bilateral symmetry of mesiobuccal roots has been shown to be in the range of 66% to 88% (Kim et al, 2012; Guo et al, 2014).
The reported incidence of MB2 canals in maxillary second molars, assessed using CBCT, is relatively high, ranging between 34% and 42% (Lee et al, 2011; Kim et al, 2012). Kim et al (2012) reported that fused roots occur more frequently in maxillary second molars, with an incidence of 11% (Kim et al, 2012). The same study identified supplemental canals in 1% of distobuccal roots of maxillary first molars and in 2% of palatal roots of second molars.
Mandibular first molar teeth display several anatomical variations. The major variant in this tooth type is the occurrence of a supplemental distolingual root, which has a reported frequency of between 14% and 29% (Abella et al, 2012; Zhang et al, 2011). Tu et al (2007, 2009) demonstrated that CBCT identifies more of these additional roots compared to conventional periapical radiography. Some mandibular first molar teeth also exhibit an isthmus between the mesiobuccal and mesiolingual canals, which can be instrumented to length (Karapinar-Kazandag et al, 2010). This is known as an accessory mesial canal, an anatomical feature that has been identified by CBCT in between 3% and 27% of Chinese and Brazillian populations, respectively (Wang et al, 2010; Soares de Toubes et al, 2012). The in vitro study by Soares de Toubes et al (2012) showed good agreement between CBCT and the dental operating microscope in the detection of accessory mesial canals, compared to parallax digital radiography, which was deemed unreliable for detecting these additional canals.
Mandibular molars with C-shaped canal configurations present distinct endodontic treatment challenges (Fig 6-2). Typically, this canal configuration is found in teeth with fusion of roots either on the buccal or lingual aspect. The incidence of C-shaped canal systems appears to be dependant on the race of the group under examination and was found to be as low as 3% in an American population, and as high as 31% in Chinese and Korean populations (Yang et al, 1988; Seo et al, 2004).
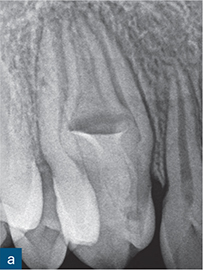
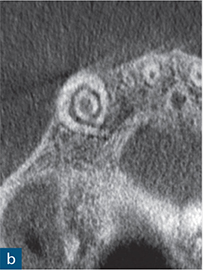


Fig 6-3 (a) Periapical radiograph showing a dens invaginatus of a maxillary right canine. (b and c) CBCT slices were used to reconstruct a three-dimensional (3D) image, which (d) showed no apparent communication between the invagination (blue) and the root canal space (red).
Zheng et al (2011) examined the root morphology and root canal anatomy of mandibular second molar teeth in a Chinese population using CBCT. They reported that 39% of mandibular second molars had fused roots, and 39% had C-shaped anatomy. The authors also noted that the ‘continuous’ and ‘semi-colon’ categories of C-shaped canals have a tendency to divide into multiple canals in the middle and apical regions. C-shaped mandibular molars occurred bilaterally in 81% of the patients studied (Zheng et al, 2011).
Anomalous tooth forms
Genetic, traumatic and environmental factors may cause aberrations in tooth dimension, morphology, position and structure (Brook, 1975). A detailed radiographic examination is essential to determine the existence and nature of the dental anomalies.
Dens invaginatus
Dens invaginatus is a developmental anomaly resulting from epithelial invagination of the crown of the developing tooth before mineralisation. Its prevalence has been reported to be between 0.3% and 10% of teeth, with the maxillary lateral incisor being most commonly affected (Alani and Bishop, 2008). Morphologic variations can range from a minor enamel-lined invagination, to extensive invagination with penetration of the root and communication with the periodontal ligament laterally or at the apical foramen (Oehlers, 1957).
Reconstruction of CBCT data permits a visual and geometrically accurate appreciation of the course of the invagination and how it relates to the main canal(s) of the tooth (Patel, 2010; Nosrat and Schneider, 2015) (Fig 6-3). Case reports have shown how the assessment of CBCT data can allow successful planning of access strategies to the coronal and apical portions of the infected root canal system in cases of dens invaginatus (Durack and Patel, 2011; Capar et al, 2015) (Fig 6-4).
Kfir et al (2013) presented an innovative therapeutic approach by producing precise three-dimensional (3D) models of a tooth with dens invaginatus. These models facilitated the treatment planning process and the trial runs of different treatment techniques prior to clinical implementation. In addition, the authors enhanced the CBCT images with a dynamic 3D video, which clearly illustrated the apical exit of the invagination, its size, and its relationship to the apical foramen of the main root canal.
Taurodontism
Taurodontism is a developmental dental anomaly characterised by vertically enlarged pulp chambers, apical displacement of pulp floors and short roots (Gomes et al, 2012). Taurodontism can occur in between 2.5% and 3.5% of chromosomally normal Caucasians, but is more commonly associated with syndromic patients (Marques-da-Silva et al, 2010). This anomalous tooth form presents challenges for the location of the root entrances, and exhibits variability in the number of root canals, with some reports describing the existence of up to six canals (Sert and Bayirli, 2004). Extreme variations in root canal anatomy among taurodonts, including maxillary and mandibular hypertaurodonts with C-shaped canals, have been identified using CBCT (Fig 6-5) (Radwan and Kim, 2014).



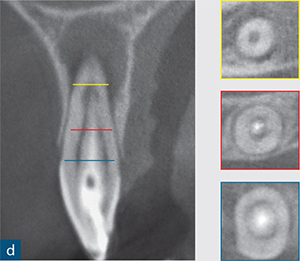
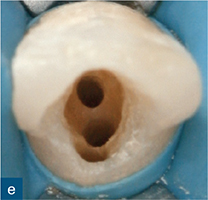

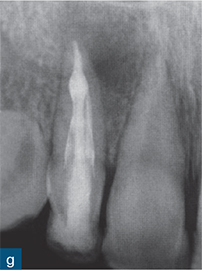

Fig 6-4 (a) Diagnostic periapical radiograph of the invaginated tooth 12. (b) Parallax radiograph. (c) Sagittal reformatted slice of the invaginated tooth. (d) Axial slices at various points denoted on the sagittal section (colour-coded). (e) Access cavity revealing the opening of the invagination (central canal entrance) and the palatal and labial channels created to gain access to the root canal system. (f) Master gutta-percha point radiograph. (g) Post-treatment radiograph. (h) 1-year follow-up revealing complete healing of the periapical radiolucency (courtesy of Durack C, Patel S. The use of cone beam computed tomography in the management of dens invaginatus affecting a strategic tooth in a patient affected by hypodontia: a case report. Int Endod J 2011;44:474–483.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


