Introduction
Patients affected by cleft lip and palate often have complaints of snoring and respiratory difficulties during sleep. The purposes of this study were to evaluate nasopharyngeal, oropharyngeal, and total airway volumes of patients affected by unilateral cleft lip and palate and to compare them with a well-matched control group without unilateral cleft lip and palate using cone-beam computed tomography.
Methods
The study sample consisted of 60 patients (26 girls, 34 boys) divided into 2 groups: unilateral cleft lip and palate (20 boys, 10 girls; 8 right sided, 22 left sided; mean age, 14.6 ± 3.2 years) and no cleft (control group; 14 boys, 16 girls; mean age, 14.8 ± 2.8 years). Nasopharyngeal, oropharyngeal, and total airway volumes of the subjects in both groups were calculated 3 dimensionally with cone-beam computed tomography. Group differences in relation to cleft side, sex, and cleft presence were statistically tested at P <0.05.
Results
Patients affected by unilateral cleft lip and palate had similar airway volumes regardless of the side of the cleft. In addition, no statistically significant differences were found between the sexes in the 2 groups. Patients affected by unilateral cleft lip and palate had smaller nasopharyngeal, oropharyngeal, and total airway volumes when compared with the control group. The difference for oropharyngeal airway volume (−4036.7 mm 3 ) was statistically significant ( P <0.05), whereas nasopharyngeal volume (−21.6 mm 3 ) and total airway volume (−4057.3 mm 3 ) differences were not significant ( P >0.05).
Conclusions
Patients affected by unilateral cleft lip and palate had decreased volumes of oropharyngeal ( P <0.05) and total ( P >0.05) airways compared with the well-matched control group without unilateral cleft lip and palate.
Clefts involving the lip or palate are the most common congenital malformations of the craniofacial region, accounting worldwide for around 15% of all congenital malformations. A cleft lip and palate (CLP) can be either unilateral (UCLP) or bilateral (BCLP); however, an isolated cleft palate involves only the secondary palate. Although clefts have not been completely explained yet, genetic and environmental factors might be responsible for their etiology and pathogenesis.
Patients affected by CLP usually have complaints of snoring and respiratory difficulties during sleep, as stated by their parents. It was also stated that patients affected by CLP had increased incidence of mouth breathing and hypopnea during sleep. According to Imamura et al, adenoidal tissues were significantly larger in the juvenile patients affected by UCLP than in the control group of age-matched patients without clefts. Patients with respiratory difficulties are at increased risk for cardiovascular and cerebrovascular diseases, hypertension, and excessive sleepiness during the daytime, and thus the evaluation of the pharyngeal airway in patients affected by CLP is important.
The authors of several studies evaluated the pharyngeal airways in patients affected by clefts; some were performed on 2-dimensional (2D) radiographs. Lateral cephalometric films are the most commonly used method for the evaluation of airways because of their simplicity, availability, and low cost. However, lateral cephalometric films suffer from severe limitations including 2D interpretation of 3-dimensional (3D) structures, distortion, low reproducibility because of difficulties in landmark identification, differences in magnification, and superposition of bilateral craniofacial structures. Thus, the validity of this diagnostic approach to examine the airway seems to be questionable compared with 3D evaluations with computed tomography (CT) and cone-beam CT (CBCT). Recently, CBCT has become a well-accepted diagnostic technique for the evaluation of airways because of its lower radiation doses and faster image acquisition times compared with the CT technique. In a systemic review, it was indicated that 3D analysis of the upper airway with CBCT can be accurate and reliable. In addition, Aboudara et al stated that CBCT is a simple and effective method for the evaluation of the upper airway.
Recently, a few CBCT studies have assessed the pharyngeal airways in patients affected by unrepaired isolated cleft palate and CLP. Of them, 1 study included 10 adolescent patients with UCLP and 4 patients with BCLP. Another study included 19 juvenile patients affected by cleft lip with or without cleft palate; 16 patients had unilateral and 3 had bilateral cleft lip with or without cleft palate. In addition, those patients were all treated by rapid maxillary expansion (RME) before the study. In light of the information from El and Palomo, RME creates a significant increase in the nasal passage airway. Thus, the aims of our study were to evaluate pharyngeal airway volumes of patients affected by UCLP and to compare our findings with a well-matched control group without UCLP using 3D analysis on CBCT.
Material and methods
A retrospective study was performed on CBCT radiographs of 60 patients (26 girls, 34 boys; mean age, 14.7 ± 3.1 years) who were randomly selected from the archive of the Department of Oral and Maxillofacial Radiology, Erciyes University, Kayseri, Turkey. CBCT scans used in this study were part of the diagnostic records collected because of orthodontic treatment need (skeletal or dental malocclusions, and maxillary canine impaction), and no patient was contacted or CBCT image taken for the purpose of this study. All patients’ parents had signed an informed consent agreeing to the use of the data for scientific research before dental or orthodontic treatment, and ethical approval was obtained from local ethics committee of Erciyes University.
The sample size was calculated based on the method described by Pandis, a significance level of 0.05, and a power of 95% to detect a difference of 2 cm 3 (±2 cm 3 ) for the oropharyngeal volumes between the groups. The power analysis showed that 27 patients were required in each group. To increase the power of the study, we included the records of the 30 patients in each group. The patients were divided into 2 groups: (1) 30 patients affected by complete UCLP (20 boys, 10 girls; 8 right sided, 22 left sided; mean age, 14.6 ± 3.2 years) and (2) 30 patients (14 boys, 16 girls; mean age, 14.8 ± 2.8 years) with no clefts as the control group. The patients in the control group had dental (determined from plaster models) and skeletal (determined from SNA, FH-NA, SNB, FH-NB, and ANB measurements) Class I relationships, no severe hyperdivergence (SN-GoMe, <38°), and no symptoms of upper airway obstruction (using an anamnesis form). All patients affected by UCLP had the same surgical procedure (lip and hard-tissue closures) before 3 years of age. The patients in both groups had no previous orthodontic treatment, orthognathic surgery, trauma, syndromes, or tonsillectomy and adenoidectomy.
All images used in our clinic were taken in a standard position in a supine position using the same device (NewTom 5G; QR, Verona, Italy). Scanning times were 14 to 18 seconds, collimation height was 13 cm, exposure time was 3.6 seconds, and voxel size was 0.3 mm 3 . The patients were asked to bite with maximum interdigitation but not to swallow and not to move their heads or tongues during scanning. The 3D images were transformed to DICOM format and reconstructed with the Simplant Pro software (version 13.0; Materialise, Leuven, Belgium).
Each 3D-rendered image was then reoriented using the Frankfort horizontal plane as its horizontal reference plane, which was constructed from the right and left porions, which are located in the most laterosuperior point of the external auditory meatus and the right orbitale, the most inferior point of the lower margin of the bony orbit. The sagittal reference plane was constructed from nasion and the midorbital point, perpendicular to the horizontal reference plane. The axial plane was constructed from nasion, perpendicular to the horizontal and sagittal planes.
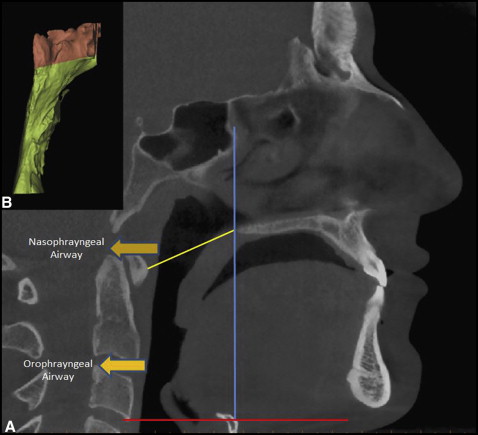
The borderlines of the pharyngeal airway consisted of the anterior border, which is a vertical plane through the posterior nasal spine, perpendicular to the sagittal plane. The posterior border was the posterior wall of the pharynx, and the inferior border was a plane tangent to the most caudal medial projection of the third cervical vertebra, perpendicular to the sagittal plane. A plane perpendicular to the sagittal plane through the posterior nasal spine and the lower medial border of the first cervical vertebra divided the pharyngeal airway into 2 segments: upper (nasopharyngeal airway) and lower (oropharyngeal airway) compartments. The 3D volumetric measurements described above ( Fig ) were performed with the Simplant software by an experienced maxillofacial radiologist (A.E.S.) randomly without knowing whether the patient was affected by UCLP. Craniofacial measurements (SNA, FH-NA, SNB, FH-NB, ANB, and SN-GoMe) were performed on cephalometric films obtained from the CBCT images.
Statistical analysis
To determine the random error associated with digitizing the measurements, 18 radiographs (30% of the data) were selected randomly. All procedures such as landmark identification, tracing, and measurements were repeated 3 weeks after the first examination by the same investigator (A.E.S.) without knowing the first measurements. Intraclass correlation coefficients were performed to assess the reliability of the measurements as described by Houston. In addition, the differences between the 2 readings by the same investigator were tested to estimate the systemic error with the paired t test.
After the Kolmogorov-Smirnov test to test the normality of the measurements, parametric tests were used to analyze the data. The Student t test was performed to compare airway volumes, craniofacial measurements (SNA, FH-NA, SNB, FH-NB, ANB, and SN-GoMe) between the UCLP and control groups, and airway volumes between the sexes in each group. The Mann-Whitney U test was performed to compare left- and right-sided UCLP patients for pharyngeal airway volumes. The sex distribution was tested by means of the Pearson chi-square test. All statistical analyses were made with the SPSS software package for Windows 98 (version 10.0; SPSS, Chicago, Ill) at P <0.05.
Results
The coefficients of reliability of the measurements were above 0.992 for the volumetric measurements (0.992-0.997) and above 0.990 for the cephalometric measurements (0.990-0.997). The results of paired t tests showed no significant differences between the first and second examinations, confirming that all measurements were free of systemic errors ( P >0.05).
Table I shows the demographic values of the patients in both groups and confirms that the UCLP and control groups were matched for chronologic age and sex distribution as tested by the Student t test and the Pearson chi-square test, respectively. Patients affected by UCLP had decreased SNA ( P <0.01), FH-NA ( P <0.01), and ANB ( P <0.001) measurements, and increased SN-GoMe ( P <0.001) and FH-NB ( P <0.01) measurements compared with the control group.
| Cleft group | Control group | P | |
|---|---|---|---|
| Number ∗ | |||
| Male | 20 | 14 | |
| Female | 10 | 16 | 0.118 |
| Chronologic age (y) † | 14.6 ± 3.2 | 14.8 ± 2.8 | 0.846 |
| SNA (°) † | 77.1 ± 3.2 | 79.6 ± 3.3 | 0.003 |
| FH-NA (°) † | 88.0 ± 3.4 | 91.8 ± 3.9 | 0.001 |
| SNB (°) † | 77.3 ± 3.0 | 77.1 ± 3.6 | 0.757 |
| FH-NB (°) † | 91.8 ± 3.9 | 89.3 ± 2.3 | 0.004 |
| ANB (°) † | −0.1 ± 3.1 | 2.5 ± 1.0 | 0.000 |
| SN-GoMe (°) † | 37.4 ± 5.5 | 32.7 ± 3.0 | 0.000 |
∗ Results of the Pearson chi-square test comparing the distribution of the sexes.
Table II shows the comparisons of nasopharyngeal, oropharyngeal, and total airway volumes between left- and right-sided UCLP patients. Since there were fewer right-sided UCLP patients (8) than left-sided UCLP patients (22), the Mann-Whitney U test was performed, and it showed no significant difference between right- and left-sided clefts ( P >0.05). In addition, the comparisons between the sexes for both groups showed no significant difference ( P >0.05; Table III ). Therefore, the volumetric measurements were pooled for further statistical comparisons between the UCLP and control groups.
| Nasopharyngeal airway (mm 3 ) | Oropharyngeal airway (mm 3 ) | Total airway (mm 3 ) | |
|---|---|---|---|
| Right-sided cleft (8 patients) | 7463.1 ± 4130.3 | 13189.0 ± 10103.5 | 20653.1 ± 13343.9 |
| Left-sided cleft (22 patients) | 6398.2 ± 2761.5 | 8607.5 ± 4469.9 | 15006.0 ± 5793.6 |
| P ∗ | 0.421 | 0.092 | 0.113 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


