The respiratory system
Publisher Summary
This chapter presents the physiological study results of the respiratory system. The lungs and respiratory passages, or airways, are an invagination of the body surface specifically modified for the easy and rapid transfer of the respiratory gases—oxygen and carbon dioxide—to and from the blood. Air is moved actively through the nose, passes the oro-nasal cavity, and then reaches the trachea that divides into a right and a left bronchus both of which subdivide into bronchioles. These divide into smaller and smaller branches until they terminate in bubble-like sacs, the alveoli. These are formed of a single layer of epithelial cells and profusely covered with capillaries. The lungs are enclosed in a double layer of fibrous and elastic tissue called the pleura. Blood reaches the lungs from the right side of the heart through the pulmonary arteries and returns to the left atrium in the pulmonary veins. The bronchioles and bronchi have a separate blood supply. The only tissue in the lungs apart from the alveolar membranes and the tissues of blood vessels, bronchi and bronchioles, is the small amount of fibrous and elastic tissue that supports the alveoli. Ventilation also is greatest at the base of the lungs and least at the apices but the difference is relatively much less than for perfusion.
Although the word respiration is derived from the Latin for breathing, the term has been widened to include those biological oxidations necessary for energy production. Respiration, then, includes inspiration and expiration (the movement of air in and out of the lungs), the exchange of oxygen and carbon dioxide at the lung membranes, the transport of oxygen and carbon dioxide to and from the tissues of the body, and the chemical processes of oxidation of foodstuffs. The last of these topics is usually dealt with by biochemists rather than physiologists.
The apparatus of breathing
where P is tThe vascular tubing he pressure inside the bubble tending to expand it, T is the tension in the bubble wall tending to contract it, and r is the radius of the bubble. This Law (already mentioned in Chap. 7 to explain some of the characteristics of the heart and blood vessels) predicts that if the surface tension of a bubble remained constant the pressure needed to maintain the bubble would increase as the radius decreased. Thus small bubbles collapse more readily than large bubbles. Collapse of the alveoli is prevented because the surface tension of the surfactant decreases as its film thickness increases. As the alveoli are deflated and decrease in radius, the surfactant lining spread over a smaller surface increases in thickness and lowers the surface tension to equilibrate the forces on the alveolar walls. The total surface area of the alveoli is of the order of 60 m2. The blood flow to the lungs is the same as that to the whole of the systemic circulation: 51/min at rest, rising to 251/min during exercise. Blood reaches the lungs from the right side of the heart via the pulmonary arteries (which carry deoxygenated blood after its return to the heart) and returns to the left atrium in the pulmonary veins. The bronchioles and bronchi have a separate blood supply. The only tissue in the lungs apart from the alveolar membranes and the tissues of blood vessels, bronchi and bronchioles, is the small amount of fibrous and elastic tissue which supports the alveoli.
The lungs are enclosed in a double layer of fibrous and elastic tissue called the pleura. Between the inner layer attached to the lungs themselves and the outer layer attached to the walls of the thorax is a film of fluid. Were the pleura not present to connect the lungs to the thoracic wall, the lungs would be relaxed and much smaller. The chest wall, on the other hand, would expand to give a thoracic cavity with a greater than usual volume. Because chest wall and lungs are held in apposition by the pleura, both are under tension – the chest wall pulled inwards, and the lungs pulled outwards. An equilibrium therefore exists between the opposing pulls of the elastic tensions in these two structures. This is transmitted to the fluid layer between the pleura: the surface tension of this fluid layer prevents the lungs collapsing inwards on themselves. In other words, there is a negative or sub-atmospheric pressure in the potential space between the layers of the pleura. This is the intrapleural pressure. Stretching of the lung tissues helps to maintain the patency of the alveoli because it draws in air to fill them. The lungs themselves have no muscle tissue; changes in their size and shape depend upon the muscular activity of the thorax transmitted to them by the flexible linkage formed by the pleura. This linkage is broken if the layers of the pleura are separated, as for example when air gains admittance to the pleural cavity, either as a result of physical damage to the chest wall or by deliberate injection into the space. When this happens the visceral and parietal layers separate, the nearby lung collapses inward by virtue of its own elasticity and the chest wall recoils outward. This condition, termed pneumothorax, is sometimes induced deliberately to allow a part of the lung tissue to rest. If the pleural space is resealed the air will eventually be absorbed into the bloodstream. The link between lungs and thorax can also be affected by infection or damage to the pleura when this results in formation of fibrous tissue between the two layers – an adhesion – which prevents their movement relative to each other and impairs the normal functioning of the lung locally.
The thorax itself is made up of the ribs and the intercostal muscles, and is separated from the abdominal cavity by the dome-shaped muscle of the diaphragm. There are two layers of intercostal muscles, the external intercostals which slope downward and forward, and the internal intercostals which slope downwards and backwards. Since the ribs themselves slope downwards and forwards from the spine and can rotate at the joints with the vertebrae, the intercostal muscles can change the shape of the thorax when they contract. The external intercostals raise the ribs, rotating the moveable front portion upwards and thus increasing the antero-posterior dimension of the thorax. The internal intercostals have the reverse effect. Thus the external intercostals assist in producing the increase in thoracic volume needed for inspiration. The main muscle of quiet breathing, however, is the diaphragm. This is dome-shaped with its fibres running from their attachment at the lower border of the rib-cage to their insertion into the central tendon. Contraction of the fibres reduces the height of the dome, by pulling the central tendon downwards (Fig. 8.1).
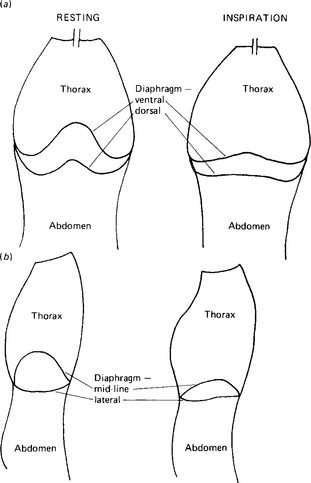
Figure 8.1 Diagram to show the changes in dimensions of the thorax during inspiration. the changes in horizontal dimensions are exaggerated in order to show them more clearly, (a) the thorax before (left) and during (right) inspiration; (b) sagittal section through the thorax before (left) and during (right) inspiration.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



