In the management of a patient’s orthodontic treatment, the devil is frequently in the details. In completing a patient’s orthodontic treatment, barring any significant complications imposed by skeletal discrepancies, missing teeth, or other conditions, a clinician may spend as much time completing the details as in making the major corrections related to crowding and space closure. Frequently, patients start to become impatient with the process, particularly if the remaining treatment involves second-order and third-order changes in the posterior dentition, which they usually cannot see.
Although necessary adjustments to address these details may not become evident until a certain stage in treatment, many of these details can be foreseen in the original diagnosis and treatment plan, as well as during bracket selection and placement. Although many authors have written extensively on the finishing details in orthodontic treatment, adequate attention has not been given to the potential impact of proper bracket selection and placement on these details.
OBJECTIVE VERSUS SUBJECTIVE ASSESSMENT
Only some of the finishing details discussed here involve variables that are quantifiable and therefore can be measured objectively. For example, the desirable overbite at the end of treatment could be identified as either 2 or 3 mm, with reasons cited for either preference. At the end of treatment, it would also be possible to measure (quantify) this variable. Also at the end of treatment, there should be no open spaces in the dental arches, unless the space is specifically targeted for subsequent buildup of a tooth with a restoration; the presence or absence of spaces can be quantified.
A number of other variables involve a high degree of subjectivity, partly because of the personal preferences of patients and clinicians and partly because of the difficulty in quantifying them because of the difficulty in obtaining objective measurements. For example, the degree of mesiodistal tip on the maxillary anterior teeth can be varied to a certain degree, with some differences in the esthetic outcome. Indeed, a range of possible axial inclinations for the maxillary anterior teeth would result in an esthetic appearance that could be pleasing to the patient or the clinician, without significant impact on stability or the patient’s long-term dental health and function. Similarly, clinicians may have differing viewpoints on the desirable axial inclinations of the posterior teeth in the transverse plane of space. Most patients are unlikely to give this much thought, but the functional outcome for the patient would clearly be different. Now add, for example, the difficulty in measuring the actual buccolingual inclination of a molar, let alone the difficulty in achieving a consensus on a reference plane to make such measurements.
The point is simple: certain factors in the finishing of an orthodontic case will affect primarily the esthetics of the finished result, other variables will influence primarily the patient’s long-term dental health and function, and yet another set of variables will affect both. Some factors are quantifiable and therefore measurable. Other clinical details are more subjective, and either difficult or impossible to quantify. Further, a significant range of orthodontic opinions exists regarding both the appearance and the function of the treatment result, as evidenced by differing opinions between a practitioner of the “Tweed” philosophy and another practitioner of the “Bioprogressive” school of thought. The anterior torque values vary significantly between these two practitioners, with an identifiable difference in the esthetics and the function of the treatment results.
Andrews was among the first to present a structured assessment of the treatment result. His definition of the “six keys to normal occlusion” constituted the first real effort to tabulate specific variables that could be measured in the finished orthodontic result. Indeed, this was the foundation of the then-nascent process of developing pretorqued and preangulated appliances. Before that time, torque, tip, and offsets were not “measured,” only visually assessed.
THREE-DIMENSIONAL GRAPHIC ANALYSIS
Many pretorqued and preangulated appliance systems are currently available to the orthodontic practitioner. These prescriptions are based on a foundation of clinical principles, as well as the personal and philosophical preferences of the individual clinician. However, objective documentation on the efficacy of these various prescriptions has been lacking in the literature, and most of the evidence presented appears to be anecdotal. Further, a clinician wanting to test a specific prescription must treat a sample of patients over a minimum of 2 to 3 years, to appreciate the clinical details—a cumbersome approach.
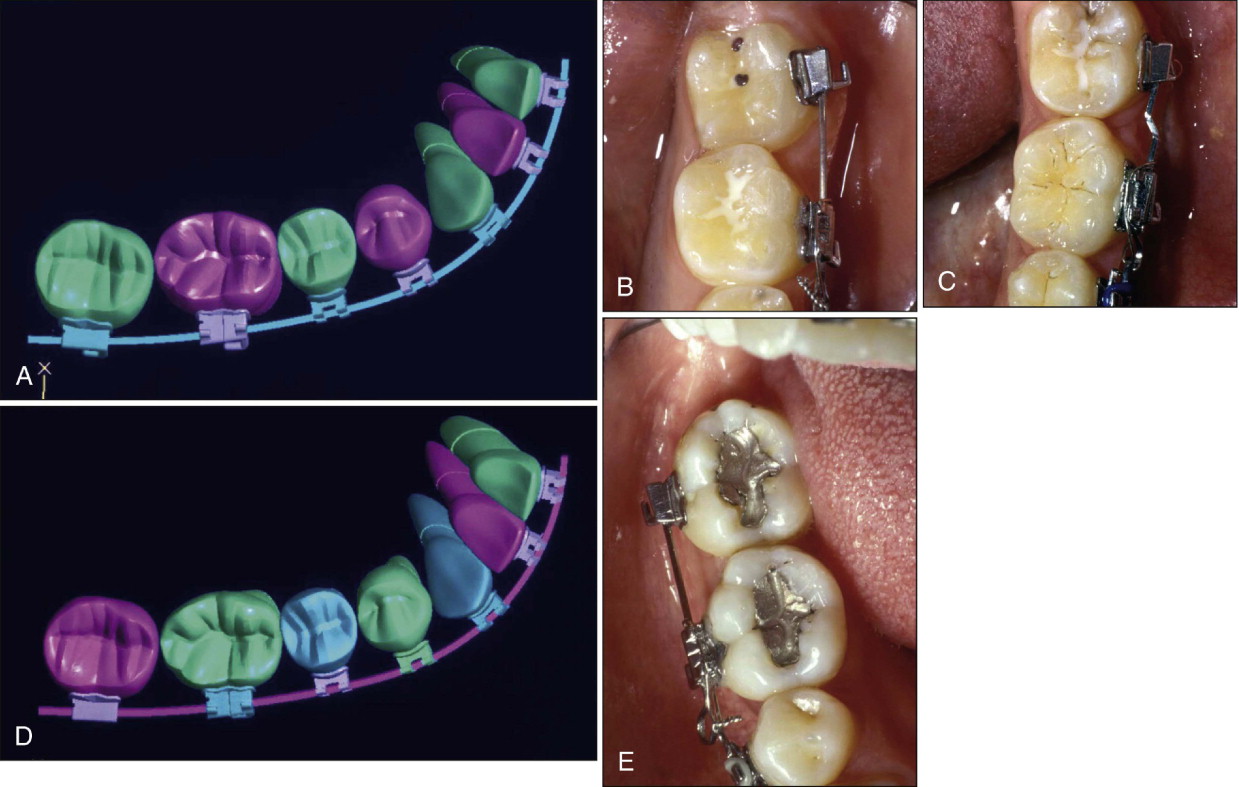
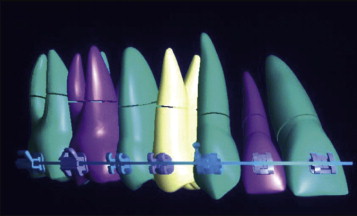
Therefore the authors goal was to construct a virtual dentition ( Fig. 7-1 ), progress to the development of a virtual occlusion, and then test the efficacy of the appliance design on the virtual dentition before applying it to the patient. This also allowed objective comparison of the effects of different torques, angulations, and prescriptions.
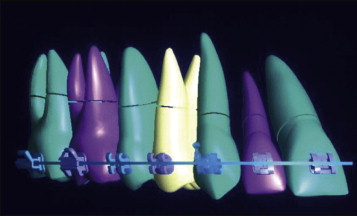
The purpose of this process was straightforward. Instead of extrapolating treatment results influenced by patient compliance, variations in morphology, and other uncontrollable factors, the impact of appliance designs would be evaluated by creating a standardized virtual dentition free of these influences. Standardized virtual appliances were then applied to this dentition to study the outcome of specific bracket placement, torque, and tip application, varying one factor at a time. For example, with the rest of the dentition and the appliance kept as a constant, a single tooth was identified for variation of the selected torque in the bracket ( Fig. 7-2 ), allowing measurement of the impact of the changed variable on the tooth’s finished position. Conversely, to study the impact of a specific orthodontic prescription on the entire dental arch, the dentition could be kept as a standard, and the entire appliance system changed; thus the impact on the combined axial inclinations in all three planes of space could be studied by rotating the model in each plane.
Opinions still differ on assessment of occlusal function and the functional aspects of the occlusion. However, it is widely accepted that “balancing interferences” are undesirable during lateral movements, for both periodontal reasons and concerns about the impact on temporomandibular function. Some authors have identified the impact of occlusal dysfunction associated with a significant lateral shift of the mandible. These functional aspects of occlusal function are usually viewed as “quantifiable,” but are not always easy to measure.
THREE-DIMENSIONAL GRAPHIC ANALYSIS
Many pretorqued and preangulated appliance systems are currently available to the orthodontic practitioner. These prescriptions are based on a foundation of clinical principles, as well as the personal and philosophical preferences of the individual clinician. However, objective documentation on the efficacy of these various prescriptions has been lacking in the literature, and most of the evidence presented appears to be anecdotal. Further, a clinician wanting to test a specific prescription must treat a sample of patients over a minimum of 2 to 3 years, to appreciate the clinical details—a cumbersome approach.
Therefore the authors goal was to construct a virtual dentition ( Fig. 7-1 ), progress to the development of a virtual occlusion, and then test the efficacy of the appliance design on the virtual dentition before applying it to the patient. This also allowed objective comparison of the effects of different torques, angulations, and prescriptions.
The purpose of this process was straightforward. Instead of extrapolating treatment results influenced by patient compliance, variations in morphology, and other uncontrollable factors, the impact of appliance designs would be evaluated by creating a standardized virtual dentition free of these influences. Standardized virtual appliances were then applied to this dentition to study the outcome of specific bracket placement, torque, and tip application, varying one factor at a time. For example, with the rest of the dentition and the appliance kept as a constant, a single tooth was identified for variation of the selected torque in the bracket ( Fig. 7-2 ), allowing measurement of the impact of the changed variable on the tooth’s finished position. Conversely, to study the impact of a specific orthodontic prescription on the entire dental arch, the dentition could be kept as a standard, and the entire appliance system changed; thus the impact on the combined axial inclinations in all three planes of space could be studied by rotating the model in each plane.
Opinions still differ on assessment of occlusal function and the functional aspects of the occlusion. However, it is widely accepted that “balancing interferences” are undesirable during lateral movements, for both periodontal reasons and concerns about the impact on temporomandibular function. Some authors have identified the impact of occlusal dysfunction associated with a significant lateral shift of the mandible. These functional aspects of occlusal function are usually viewed as “quantifiable,” but are not always easy to measure.
SELECTION OF BRACKETS AND TUBES
Although clinicians generally accept that the choice of brackets and bracket systems influences the treatment outcome, the impact of bracket choice and placement on specific finishing details has been inadequately addressed. This point can be illustrated by studying a simple finishing detail that frequently requires significant treatment time and can occasionally vex the clinician.
It became increasingly apparent over the past 20 years that the mandibular second molars ought to be aligned properly within the dental arches at the completion of orthodontic treatment. Although patients would neither recognize nor be concerned about the alignment of the second molars, clinicians are certainly aware of the long-term periodontal and dental health consequences of poorly positioned and poorly inclined mandibular second molars.
Consider, then, that the clinician has a choice of molar tubes from which to select the specific appliance to use on patients. Some clinicians might promote placement of a mandibular first molar tube with a distal offset, providing a mesial-out rotation on the molar and presumably improving the alignment of the dental arch. This harkens back to the days when molar offsets routinely had to be placed in archwires because non-preadjusted appliances did not account for variations in morphology.
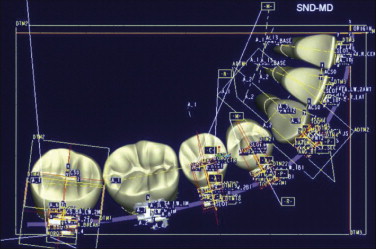
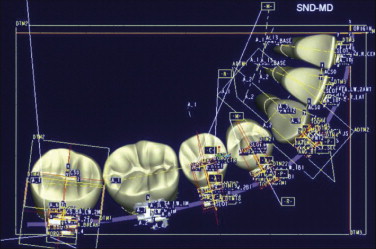
However, if we use a mandibular first molar tube with a distal offset and then study the impact on the contact point between the first and second molars, it becomes quickly apparent ( Fig. 7-3, A and B ) that an undesirable distolingual rotation of mandibular first molar will be expressed. Clinically, this generally requires compensation by putting an offset in the archwire ( Fig. 7-3, C ). The net result is that the archwire adjustment became necessary to undo the movement expressed by the offset built into the tubes. This would therefore argue for a molar tube that does not have a distal offset ( Fig. 7-3, D and E ), because this seems to deliver the desirable outcome in establishing a proper contact relationship between the mandibular first and second molars.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses