Use of incisions that minimize visible scars is an important principle of craniomaxillofacial surgery. To accomplish this goal, the coronal incision and scalp flap are frequently used during combined craniomaxillofacial and neurosurgical procedures.
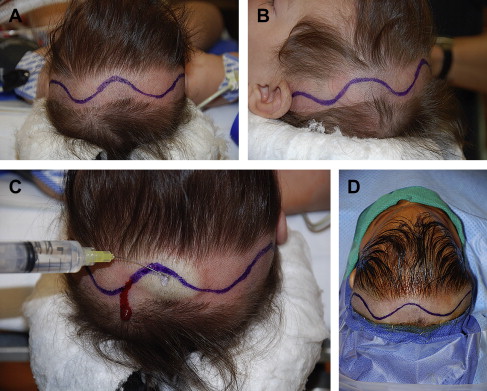
Prior descriptions of the coronal scalp flap include an incision just behind the hairline with the lateral components of the approach created in the pre-auricular areas: the hairline of the patient being a primary consideration in the placement of the incision for the flap. Although anterior extension of the midportion of the coronal flap was considered to enhance flap retraction and access to the midface, the resulting scar may subsequently become obvious with male pattern baldness. Over time, this scalp flap technique has been refined with the introduction of a postauricular location. An important technical point is for the surgeon to understand that a more posterior placement of the incision will not limit access to the orbital structures. The amount of exposure of the cranio-orbital skeleton is related proportionately to the inferior extent of the incision and not necessarily to a more anterior position. The incision is placed from one auricular area to the other and the degree of skeletal exposure required for a given procedure dictates the inferior extent of the incision. When access to the zygoma and infraorbital rims is necessary, the incisions must be extended further inferiorly. The incision is outlined within the postauricular region to more effectively conceal the postsurgical scar. The authors’ preference is to place the incision behind the top of the vertex of the head rather than carrying it toward the forehead ( Fig. 1 ) . The use of a postauricular coronal incision eliminates visible scars in the preauricular area and decreases risk to the frontal branch of the facial nerve in reoperated patients. The postauricular placement of the incision is also desirable in children because of the tendency for the coronal incision scar to migrate forward with subsequent ongoing growth of the cranial vault.
When secondary operations are performed in cases where a previous coronal scalp flap has been used, it is preferable to reincise thru the original scar. Although it may be tempting to place the incision in a different location, consideration must be given to the effect of the previous scar on flap perfusion and wound healing.
Use of a zigzag (Stealth modification) incision avoids a straight-line scar and is particularly useful in camouflaging the scar within the surrounding hair-bearing scalp. The authors favor a variation of this technique using a curvilinear incision design. Unless meticulous attention is paid to hemostasis during the initial dissection, additional blood loss associated with a greater incision length may offset the benefit.
Surgical technique
The patient’s head is positioned on a Mayfield horseshoe-shaped headrest. Removal of hair is not mandatory. The authors will frequently clip a small strip of hair, approximately 1.5 cm in width along the location of the coronal scalp incision (see Fig. 1 ). This makes the initial dissection and subsequent closure easier with less interference from longer hair. In infants, no hair removal is necessary. When hair removal is performed, it should be done with sterile, disposable clippers. Shaving should be avoided, as it produces increased epithelial damage to the skin and contributes to an increased incidence of infection.
A curvilinear incision is outlined with a surgical marker and the patient’s head and face are prepped and draped in sterile fashion. The proposed incision line is injected with a dilute solution of 0.5% lidocaine with 1:200,000 epinephrine to aid with hemostasis. The injection is limited to the subgaleal region along the incision line. This reduces bleeding and helps initiate dissection along the subaponeurotic plane. The scalp has a rich vascular supply and so dissection is performed in segments with meticulous attention to hemostasis. Adequate hemostasis is especially important in infants and young children because of the potential loss of their blood volume. The conventional approach to minimizing blood loss during opening has been to apply hemoclips to the edge of the flap. Bipolar electrocautery is used to obtain hemostasis; this has a minimal effect on the adjacent peripheral hair follicles.
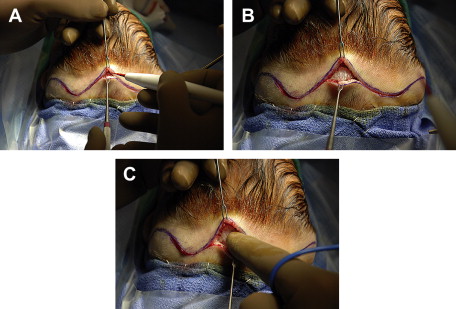
The use of monopolar electrocautery was previously contraindicated because of the increased risk of destroying regional hair follicles, which results in alopecia and a more visible scar. The authors’ preferred approach involves the use of a #15 surgical blade to create the initial skin incision. Further dissection through the subcutaneous tissues and galea aponeurotica is performed using the monopolar electrocautery with a fine-tipped Colorado needle on low-energy settings (Cut 8 and Coag 10) ( Fig. 2 ). Because dissection with the Colorado needle is done below the level of the skin and dermis, there is no damage to hair follicles. This technique also dramatically minimizes blood loss and obviates the need for the use of vascular clips ( Fig. 3 ). The authors frequently open an entire coronal scalp flap incision using this technique with less than 5 mL of blood loss.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


