Craniosynostosis and the abnormalities associated with this clinical entity pose significant challenges to the treating craniofacial and neurosurgeons caring for patients with these conditions. Ever since Lannelongue first introduced the concept of surgically treating this condition, surgeons have struggled to develop the best possible techniques . At our craniofacial center we have also used many approaches extending from minimally invasive to extensive calvarial vault remodeling techniques . Although technically rewarding at the time of surgery, the extensive calvarial vault remodeling techniques are almost universally associated with increased blood transfusion rates, massive facial swelling, bruising, and longer hospital stays. Furthermore, the results associated with these procedures are mixed at best and often times with poor outcomes when patients are followed longitudinally into their early adulthood.
About 15 years ago we decided to change our approach and began treating patients at the earliest age possible using endoscope-assisted minimally invasive procedures followed by helmet therapy for 1 year. The concept is simple and involves allowing the rapidly growing brain of an infant to reshape the craniofacial skeleton and correct the deformities associated with the prematurely closed suture. The corrective process is aided by the helmet once the stenosed suture is released, and the brain is allowed to resume its normal shape as it grows rapidly. The surgical techniques and the helmet therapy vary with each suture type and are described in detail in this article.
Sagittal suture
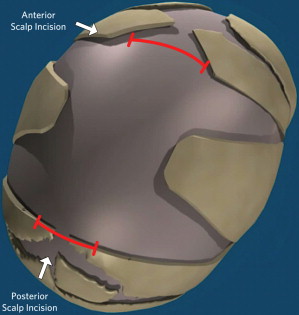
Because of predetermined genetic forces that lead the skulls of patients with sagittal synostosis to revert back to a scaphocephalic shape within a year after treatment with any procedure, we do not perform a single linear strip craniectomy. In essence, we remove a large portion of the calvarial vault extending from the anterior fontanelle to the lambda. The width of the craniectomy is inversely proportional to the child’s age. In a several-weeks-old baby, the width of the craniectomy may be as much as 5 to 6 cm, whereas in patients aged 6 months or older, it may be 2 to 3 cm. In addition, we create bilateral barrel-stave type osteotomies behind the coronal suture and in front of the lambda. These osteotomies allow for immediate increase in the euryon-to-euryon distance and cephalic index (CI).
The patient is placed in the modified prone position in a padded beanbag with a viscoelastic pad. The first scalp incision, measuring between 2 and 3 cm, is made about 2 cm behind the anterior fontanelle, transversely across the sagittal suture. Subgaleal dissection is done with a needle tip bovie and the visualization of a zero-degree 4-mm rigid endoscope (Karl Storz, Germany). A rhinoplasty lighted retractor can also be used to develop the subgaleal plane. Care is taken not to disrupt or remove the pericranium because this leads to unnecessary blood loss and poor visualization. A second incision of similar length and direction is made in front of the lambda. In a comparable method, subgaleal plane dissection is undertaken until the entire area between the lambda and anterior fontanelle is developed.
A pediatric craniotome is used to create a 7-mm burr hole on one side of each incision. The dura is freed from the overlying bone using a #1 Penfield dissector across the stenosed suture. An osteotomy is created with a 5-mm angled Kerrison rongeur. Anteriorly, a wedge of bone extending to the anterior fontanelle is then removed. This maneuver allows for the introduction of a 4-mm rigid, 30°-angled endoscope under the bone. Separation of the dura from the overlying bone is done with the aid of an insulated suction tube and extends sequentially until the posterior osteotomy is reached. Gentle sweeping motion is used as the suction tube is used to separate the dura from the bone. Whenever a perforating vein of moderate to large caliber is encountered, it may be directly coagulated under full visualization, with bipolar forceps. Because the naturally occurring fibers connecting a patent suture to the dura are absent in craniosynostosis, separating these 2 structures under endoscopic visualization is a relatively easy maneuver.
Once the dura has been fully separated from the bone, a pair of parallel osteotomies are made using Mayo scissors (Teleflex Inc, PA, USA). Because of the patient’s young age, the bone is relatively thin and easy to cut. In older patients with thicker cranium, bone-cutting scissors may be used to make the osteotomies. The bone may be folded or cut in half to remove it through the anterior scalpincision. The wedge osteotomies are done at the level of each incision and extended laterally and inferiorly toward the squamosal suture. Care is taken not to make the osteotomy too close to the coronal or lambdoid suture and risk a dural tear ( Fig. 1 ); once the bony cuts are made, osseous hemostasis is achieved using a suction-cautery bovie unit (Valley Lab, Valley Forge, PA, USA).
This unit is set at 60 W and allows for rapid and efficient hemostasis. Often, multiple passes are needed until all of the bleeding and oozing stops, and the bone is cauterized until it turns black. No untoward effects have been found with this approach, and it has no effect on new bone regeneration. Further hemostasis is obtained using Surgiflo (Johnson & Johnson, New Brunswick, NJ, USA). Before skin closure, the surgical field is inspected with the endoscope to document complete hemostasis and look for dural tears. The galea is closed with 4-0 Monocryl (Ethicon, Inc, Somerville, NJ, USA), and the skin is sealed with DERMABOND (Ethicon, Inc, Somerville, NJ, USA).
Coronal suture
After induction of general anesthesia, the patient is intubated and placed in the supine position on a pediatric horseshoe head holder. Corneal protectors with ophthalmic lubricant are used to prevent corneal abrasions or damage. A 2-cm incision is made halfway (over the stephanion) between the anterior fontanelle and the pterion on the side and across the stenosed suture. Subgaleal dissection is undertaken toward the anterior fontanelle with the aid of a rhinoplasty lighted retractor or a 0° rigid endoscope. The same maneuver is used to reach the area of the pterion and the squamosal suture on the affected side.
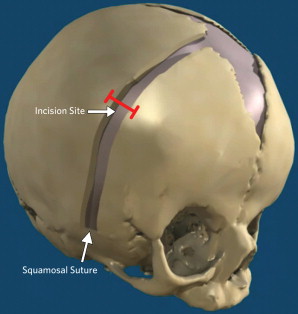
The pediatric craniotome is used to create a 7-mm burr hole at the incision. The burr hole is enlarged longitudinally along the suture axis using Kerrison rongeurs (5 mm). A 30° rigid endoscope is then inserted under the bone and first directed medially toward and up to the anterior fontanelle. The endoscope is then removed and redirected inferiorly and laterally toward and behind the pterion to reach the open squamosal suture. A 6- to 7-mm osteotomy is made with a combination of scissors and bone rongeurs, making sure that it extends all the way down to the squamosal suture ( Fig. 2 ). Failure to do so prevents the orbitofrontal complex from moving forward and inferiorly. Although at the beginning of our series part of the sphenoid wing was removed, we have found this to be unnecessary and no longer do so. Osseous hemostasis is achieved using the suction-electrocautery unit as described in the sagittal section.
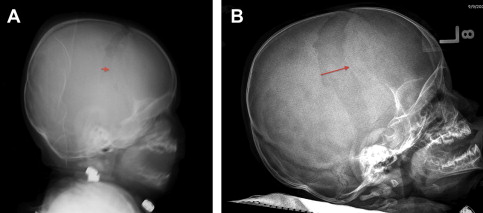
The dura overlying the coronal suture area seems to reossify at a different rate than the one over the vertex. Early on we made osteotomies as wide as 2 cm but found that it took much longer for the bone to fully reossify, and some patients were left with small areas of nonossification. In addition, the growing brain moves the frontal bone forward up to 2 to 2.5 cm, leaving a large area devoid of bone ( Fig. 3 ). As such, we limit our osteotomy to the width of the bone or Kerrison rongeurs (6 mm). The surgical area is inspected with the endoscopes, and the galea is closed with Monocryl and the skin with DERMABOND; Surgiflo and liquid thrombin (Gen Trac Inc, Middleton, WI, USA) are used to obtain complete hemostasis.
Coronal suture
After induction of general anesthesia, the patient is intubated and placed in the supine position on a pediatric horseshoe head holder. Corneal protectors with ophthalmic lubricant are used to prevent corneal abrasions or damage. A 2-cm incision is made halfway (over the stephanion) between the anterior fontanelle and the pterion on the side and across the stenosed suture. Subgaleal dissection is undertaken toward the anterior fontanelle with the aid of a rhinoplasty lighted retractor or a 0° rigid endoscope. The same maneuver is used to reach the area of the pterion and the squamosal suture on the affected side.
The pediatric craniotome is used to create a 7-mm burr hole at the incision. The burr hole is enlarged longitudinally along the suture axis using Kerrison rongeurs (5 mm). A 30° rigid endoscope is then inserted under the bone and first directed medially toward and up to the anterior fontanelle. The endoscope is then removed and redirected inferiorly and laterally toward and behind the pterion to reach the open squamosal suture. A 6- to 7-mm osteotomy is made with a combination of scissors and bone rongeurs, making sure that it extends all the way down to the squamosal suture ( Fig. 2 ). Failure to do so prevents the orbitofrontal complex from moving forward and inferiorly. Although at the beginning of our series part of the sphenoid wing was removed, we have found this to be unnecessary and no longer do so. Osseous hemostasis is achieved using the suction-electrocautery unit as described in the sagittal section.
The dura overlying the coronal suture area seems to reossify at a different rate than the one over the vertex. Early on we made osteotomies as wide as 2 cm but found that it took much longer for the bone to fully reossify, and some patients were left with small areas of nonossification. In addition, the growing brain moves the frontal bone forward up to 2 to 2.5 cm, leaving a large area devoid of bone ( Fig. 3 ). As such, we limit our osteotomy to the width of the bone or Kerrison rongeurs (6 mm). The surgical area is inspected with the endoscopes, and the galea is closed with Monocryl and the skin with DERMABOND; Surgiflo and liquid thrombin (Gen Trac Inc, Middleton, WI, USA) are used to obtain complete hemostasis.
Metopic suture
The patient is placed in the supine position on a cerebellar horseshoe head holder. Corneal protectors and ophthalmic lubricant are used as described earlier. The forehead and face are prepped with providone-iodine solution. A 2- to 3-cm incision is made across the metopic suture behind the hairline but in front of the anterior fontanelle. The incision is taken down through the galea, and the subgaleal plane is dissected with a needle tip bovie extending all the way to the nasion from the anterior fontanelle. This procedure can be done with malleable insulated scalp retractors and a 0° rigid endoscope. A pediatric craniotome is used to create a 7-mm burr hole, which is then enlarged longitudinally with 6-mm Kerrison rongeurs. A 30°-angled endoscope is inserted under the bone to develop the epidural space plane of dissection. About half way down the forehead, prominent bridging veins are often found, which extend from the sagittal sinus to the bone. These veins can be a source of significant bleeding, if not promptly and properly cauterized. The generous use of Surgiflo and gelfoam soaked with thrombin can assist in achieving successful hemostasis. Care must be taken that the epidural plane is dissected all the way to the nasofrontal suture as well as to the anterior fontanelle. The osteotomy is then made with a combination of Mayo scissors and bone-cutting rongeurs and must extend all the way down to the nasofrontal suture ( Fig. 4 ). Failure to do so leads to an unsuccessful result. Hemostasis is achieved as described earlier using the suction-electrocautery unit (set at 60 W), Surgiflo, and thrombin. The area is carefully inspected for bleeding bridging veins, oozing diploë, or dural tears. The galea and skin are closed as described earlier.
Immediate postoperative care
The patients are extubated and given intravenous morphine and rectal acetaminophen to help control postoperative pain. The patients are taken to the pediatric unit where they are observed overnight. Most patients experience various degrees of pain or discomfort during the first 8 hours after surgery. Soon afterward all patients settle down, begin oral intake appropriately and are ready for discharge the following morning. If the patient is nursing, he/she is allowed to attempt to do so immediately after surgery, and many are able to do so without difficulties. The patients are placed on an alternative schedule of ibuprofen and acetaminophen every 3 hours for the next 3 days. Typically, only a small amount of swelling is seen at the surgical site, and bruising is almost never observed.
Helmets
The use of helmets is integral to the success of our treatment protocol. In the case of sagittal synostosis, the treatment can be divided into 3 phases. The first phase occurs immediately after surgery and lasts for 6 to 8 weeks. During this period, the CI of the head is allowed to increase markedly from preoperative levels. The aim of the second phase is to overcorrect the head shape and obtain a high CI (>80). The third phase is used to maintain the overcorrected shape and to counteract the naturally occurring tendency to return to a scaphocephalic shape. The total treatment lasts until the patient is about 18 months old. We have found that the head shape and CI of the patients remain stable over time once they reach the 18-month mark. This finding is certainly true for all of the patients who have been followed into their early teenage years. Any facial or scalp swelling is allowed to decrease during the first 72 hours, and then the patient is scanned using the infrared STARscanner (Orthoamerica, Orlando, FL, USA). The scanned data are forwarded to the manufacturing facility at Orlando, where the helmet is made and shipped back the next day. The helmets are manufactured with the commercially available resin Surlyn (DuPont, Wilmington, DE, USA), which is a thermoplastic ionomer resin and the random copolymer (ethylene-co-methacrylic acid) ( Fig. 5 ). The properties of the resin make it an ideal material for molding cranial helmets. The helmet shell is made of Surlyn, and the inner padding is made of an ethylene acetate lining. Reston foam pads (3M, St Paul, MN, USA) are used to keep the helmet from shifting inappropriately. The orthotist makes the necessary adjustments, and then the patient starts wearing the helmet for a sequentially increasing duration until it is worn for about 23 hours per day. New helmets are made and fitted as the infant rapidly grows, and the head shape changes to reach the desired form ( Fig. 6 ).




