A 30-year-old woman sought treatment for malpositioned mandibular incisors; the roots were positioned outside the alveolar bone, related to severe localized gingival recession. She had been previously treated orthodontically and subsequently underwent 2 gingival grafts. The new treatment included torquing the roots back within the alveolar bone and referral to a periodontist for a gingival graft. In this clinical report, the possible spontaneous improvement of gingival recession is discussed. A hypothesis described in the literature is called the “creeping attachment” phenomenon. The literature includes conflicting reports about the cause-and-effect relationship between orthodontics and gingival recession. This clinical example reports spontaneous improvement of gingival recession after correction of tooth positioning in the alveolar bone. A gingival graft can be performed after adequate root positioning in the alveolar bone housing, thus increasing the chance of achieving more favorable results.
The relationship between orthodontics and gingival recession is controversial, and conclusive evidenced-based research is still lacking in the literature. Numerous factors play roles in the development of gingival recession, and the etiology is often multifactorial. The available scientific literature presents varying points of view on the relationship between orthodontics and gingival recession. Some recent studies have found no cause-and-effect relationship; thus, one cannot determine whether gingival recession is a consequence of orthodontic treatment. On the other hand, a recent article evaluated patients with gingival recession and found that teeth that are out of their bony housing are more likely to have this problem. Although there is research addressing this topic, few case reports show the consequences or sequelae of orthodontics and gingival recession.
Another controversial issue in the literature is whether it is possible to have spontaneous improvement in gingival recession after orthodontic movement. This phenomenon has been demonstrated in the literature related to growing patients; the evidence for adult patients is scarce.
The aim of this article is to present a clinical example of a 30-year-old woman who was referred to the orthodontic clinic at Salvador, Brazil, for treatment of malpositioned mandibular incisors related to severe localized gingival recession. The patient had insufficient labiolingual positioning of the mandibular anterior roots in the alveolar bone and inadequate control of torque. Our treatment consisted of torquing the root lingually within the alveolar bone and subsequent referral to a periodontist for a gingival graft. We also discuss the spontaneous improvement of gingival recession and the associated hypothesis described in the literature called the “creeping attachment” phenomenon.
Case report
The patient was a 30-year-old woman with no notable medical history, no use of medications or tobacco, and good oral hygiene. Her chief complaint was her fear of losing her mandibular right central incisor because of severe gingival recession and mobility. She previously underwent 3 years of treatment with another orthodontist and 2 consecutive gingival grafts that yielded unsatisfactory results. Informed consent was obtained, and the patient was aware that loss of the mandibular right central incisor was a possibility.
The retreatment intraoral photographs showed a Class I malocclusion with an adequate posterior relationship, good arch form, satisfactory overjet and overbite relationships, and no midline discrepancies. The mandibular arch had minor crowding. Her mandibular right central incisor root was severely torqued labially and displayed 4 mm of gingival recession and moderate tooth mobility ( Figs 1 and 2 ). According to Miller’s classification of gingival recession, her mandibular right central incisor was described as Class II, with the marginal recession extending to or beyond the mucogingival junction with no loss of interdental bone or soft tissue. Additionally, the mandibular right central incisor had excessive lingual root torque. The patient had a bonded mandibular lingual retainer, with an excessive amount of adhesive.

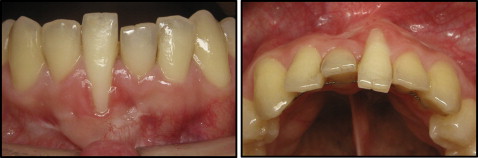
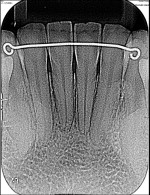
The panoramic radiograph showed that all teeth were present, the sinuses appeared to be within normal limits, and there was no intraosseous or periapical pathology. The periapical radiographs displayed a slight bone loss at the alveolar crests between the mandibular incisors ( Fig 3 ).

The overall goal of treatment was to correct the torque of the mandibular central incisors and obtain adequate labiolingual and mesiodistal root positions within the alveolar bone. Functionally, the aim was to maintain the posterior occlusion and focus attention on the mandibular dentition. Once the roots were aligned within the alveolar bone, the patient would be referred to a periodontist for a gingival graft.
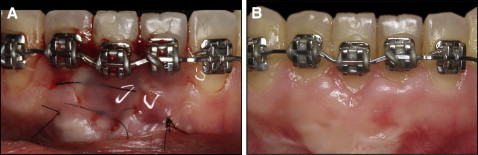
Before the orthodontic treatment, the lingual mandibular fixed retention was removed, and the patient was referred to the periodontist for a thorough evaluation. After the periodontal assessment, fixed conventional 0.022 × 0.025-in slot edgewise appliances were placed in the mandibular arch. Initially, the mandibular right lateral and left central incisors were excluded to increase the interbracket distance and allow for gentler forces during torque expression. An initial 0.016-in nickel-titanium archwire was placed for leveling and aligning. Next, a 0.019 × 0.025-in rectangular stainless steel archwire was placed passively with consistent lingual root torque in the mandibular left central incisor ( Fig 4 ). The lingual root torque was added progressively for 4 months. At this stage, the gingiva of the mandibular right central incisor showed early signs of spontaneous gingival improvement. Appliances were then placed on the remaining mandibular incisors; for these teeth, specifically the left central incisor, labial root torque was placed, while the right central incisor root was continuously torqued lingually ( Fig 5 ). After 7 months, the spontaneous gingival recession improvement continued as the right central incisor root achieved a satisfactory position ( Fig 6 ).



Although the gingival status after the orthodontic movement improved significantly, we kept the decision to proceed with the gingival graft for 4 reasons.
- 1.
With the connective tissue graft, we increased the amount of keratinized gingiva; this improved the quality and quantity of the periodontal tissues and allowed for the graft to facilitate biofilm control and make brushing more comfortable.
- 2.
According to the photos before the graft ( Fig 6 ), the gingival recession after treatment improved, but there was still a small root exposure. Thus, with the root exposed to the oral environment, the tooth was more prone to erosion, abrasion, root caries, and hypersensitivity.
- 3.
According to the patient’s chief complaint, she wished for the best approach that would allow for the combination of optimal function and esthetics. Although the gingival recession was not located in the esthetic zone, the patient was concerned about it.
- 4.
The use of Emdogain (Straumann, Andover, Mass), a biological product made up of a unique group of active proteins, naturally and predictably regenerates lost tooth attachment. The use of this product in graft surgical techniques aims to regenerate periodontal tissues such as cementum, periodontal ligament, and alveolar bone in recession defects, as shown previously.
Therefore, before debonding, the patient was referred to a periodontist for a gingival graft. The surgical technique was performed with a coronal flap associated with a connective tissue graft harvested from the palate and sutured over the root. The flap was coronally positioned to cover the connective tissue graft and sutured ( Fig 7 ). A bonded 3-3 fixed retainer was delivered after treatment. Orthodontic treatment time was 16 months.
The postorthodontic intraoral photographs show maintenance of overbite, overjet, and posterior occlusion, and improvement in the crown and root positions of the 2 main malpositioned mandibular incisors. Although the patient showed some spontaneous gingival recession improvement throughout treatment, the results after the gingival graft displayed nicely contoured gingiva around the mandibular incisors and an acceptable esthetic result with no signs of tooth mobility ( Fig 8 ).

The final panoramic and periapical radiographs showed favorable root parallelism with no signs of root resorption or bone loss near the mandibular incisors ( Fig 9 ).
The 1-year follow-up intraoral photos show a stable result with the periodontium within normal limits ( Fig 10 ).

Discussion
The etiology of gingival recession is multifactorial. Previous studies have identified that poor oral hygiene, periodontal disease, use of tobacco, inadequate restorations, frenal pull, and insufficient tooth position can be factors in the progression of gingival recession. Also, researchers have concluded that if orthodontic treatment is performed inaccurately, it can lead to gingival recession. Based on information provided by the patient, she had no gingival recession before her previous orthodontic treatment. Although the literature has demonstrated that dental position is not related to gingival recession, this phenomenon, associated with plaque accumulation or dental brush trauma, can play a vital role. Therefore, it can be hypothesized that the etiology of the gingival recession in our patient was related to plaque accumulation or toothbrush trauma and to previous orthodontic treatment with subsequent placement of the mandibular incisor roots outside the alveolar bone.
The direct correlation between orthodontic treatment and gingival recession has been strongly debated. Previous studies have found no relationship between incisor proclination and the development of gingival recession. The authors of 1 study surveyed 380 mandibular incisors after Herbst therapy and found that only 12 teeth (3%) experienced new or exacerbated recession. They concluded that there was no relationship between incisor proclination and the development of gingival recession. In another article, a similar result was found: gingival recession of the mandibular central incisors did not significantly increase during orthodontic treatment.
Although those findings show no strong correlation, the literature suggests that some aspects—eg, initial position, inclination, and gingival thickness —could play important roles for increasing the likelihood of gingival recession. Yared et al concluded that a final incisor inclination greater than 95° and a free gingival margin thickness less than 0.5 mm were directly related to more severe recession in the mandibular central incisors. Interestingly, their study showed that thickness of the marginal gingival is more relevant than incisor inclination. Also, Slutzkey and Levin evaluated patients with a history of periodontal disease and reported that the extent and severity of gingival recession show strong correlations to previous orthodontic treatment. In a recent systematic review, researchers found that teeth that are more proclined showed higher incidence and severity of gingival recession.
Tugnait and Clerehugh discussed the importance of tooth position in the alveolar bone; as long as teeth are moved within that bony housing, the risk of recession is minimal. A recent study showed that after orthodontic treatment, all teeth with greater than 3 mm of gingival recession displayed alveolar bone dehiscence and prominent facial tooth contours. It was suggested that teeth malpositioned beyond the alveolar bony housing were strongly correlated with gingival recession. In this clinical example, the tooth was positioned beyond the alveolar bone; this might have contributed to the progression of the gingival recession. The treatment objective was, through a multidisciplinary approach, to correct the tooth positioning (orthodontics) and the gingival defect (periodontics with a gingival graft).
Orthodontic edgewise mechanics were used to correct the torque of the mandibular incisor roots to within the alveolar bone. Initially, the teeth adjacent to the mandibular right central incisor were not bonded in order to increase interbracket distance. Studies have shown that when the interbracket distance is increased, the load deflection rate is decreased, creating a more flexible system. Another option described in the literature is to use resilient archwires such as titanium-molybdenum alloy. This strategy was vital to achieve progressive torque control because the goal was not only to control the force magnitude, but also to minimize the magnitude of the couple created in the bracket slot. This approach was advantageous for this patient because of the lack of bone on the buccal aspect of the mandibular incisor. To maintain the arch length and prevent proclination of the mandibular incisors during torque expression, loops were placed mesial to the molars, and the archwire was tied back.
For this patient, the importance of torque control was paramount; although numerous prescriptions of brackets are available, clinicians should customize the torque expression for each patient. Although for this patient, standard edgewise mechanics were used, some authors have suggested other strategies, such as bonding brackets upside down to obtain a desired torque expression.
During the orthodontic treatment, the progress photos show that as the mandibular right central incisor root was torqued lingually, the gingiva began to spontaneously cover the root surface. This type of phenomenon is rare and not corroborated in the literature. Engelking and Zachrisson demonstrated in an animal study that moving mandibular incisors to a more normal environment might improve alveolar bone levels. Nevertheless, they did not find any improvement in the periodontal soft tissues such as gingival recessions.
Although no research has shown spontaneous correction of gingival recession after orthodontic correction in adults, studies have shown that after gingival grafts, the amount of recession can significantly decrease over time.
It was hypothesized that the spontaneous root coverage in this patient could be related to 2 factors: the creeping attachment phenomenon and the bridging mechanism. With creeping attachment, researchers have determined that the following factors seem to influence this phenomenon: width of the recession, position of the graft, bone loss, position of the tooth, and the patient’s hygiene. Another means by which recession can heal as a result of soft-tissue grafting of the denuded root surface is by the bridging mechanism. Essentially, the remaining tissue over an avascular surface will escape necrosis and survive by receiving circulation from capillaries in the vascular portion of an adjacent recipient site. Miller explained that the single most important factor for survival of the grafted tissue over the avascular root surface is adequate blood supply from the tissues adjacent to the graft bed.
Surprisingly, this patient had undergone several attempts at periodontal grafting after her previous orthodontic treatment. After we carefully analyzed her medical and dental history as well as the results of the second orthodontic treatment, we assumed that the prior gingival graft failures could be attributed to a combination of the roots being outside the alveolar bone and the lack of blood supply.
What makes this clinical example somehow unique is that the creeping attachment phenomenon did not occur right after the grafting, but after the orthodontic movement. Therefore, it might be postulated that after the position of the tooth improved, the existing vascular tissues healed over time. An additional hypothesis that could be added to the literature is that because the root was labially placed, the gingival tissue was stretched and experienced a diminished blood supply. In addition, as the tooth was torqued lingually into a more normal environment, the stretched gingival tissue loosened and began to cover the exposed root surface.
The spontaneous root coverage in this patient was in contrast to a recent article that stated that gingival recession is not reversible. Some studies have even shown spontaneous improvement of gingival recession in children with or without treatment. In children, as teeth are moved lingually, the width of the attached and keratinized gingiva increases, whereas the clinical height of the crown decreases. In contrast, as teeth move facially, the gingival width decreases. In another study, the researchers proved that mandibular incisor gingival recession in children often improves over time, and reparative treatment in the developing dentition might not be necessary. In a follow-up study, they indicated that the children with persisting gingival recession were more likely to have a larger basal bone discrepancy between both arches and more proclined and irregularly positioned mandibular incisors. Essentially, their particular facial morphology and jaw relationship predisposed them to an inability for spontaneous correction of gingival recession. It has been hypothesized that spontaneous correction of gingival recession in children is due to growth. Although our patient had spontaneous improvement of gingival recession after correction of tooth positioning, up to this point, no evidence of the effectiveness of such a technique has been demonstrated in randomized clinical trials or case series studies.
When both gingival surgery and orthodontic treatment are planned to correct a gingival recession, it is important to consider the timing of the gingival graft. Based on the results of this clinical example, we recommend that a gingival graft should be performed only after ideal tooth positioning in the alveolar bone housing, thus increasing the chances of achieving favorable results. In addition, Kokich reported that it is important to do the periodontal graft surgery before removing the orthodontic appliances to allow for postoperative fine-tuning of the gingival margins. According to this suggestion, we referred the patient for graft surgery before debonding.
After the orthodontic retreatment and placement of the tooth within the bony housing, the patient was referred for a gingival graft. After evaluation of the final photos, it appears that our objective and the patient’s chief complaint were accomplished.
The goal of orthodontic treatment is not only to straighten teeth, but also to achieve ideal root positioning for long-term stability and a favorable environment in the periodontium. During treatment, the orthodontist must carefully control the torque, while taking into account the anatomy of the initial position of the teeth and the surrounding alveolar bone. Ultimately, the orthodontist must provide a customized torque for each patient.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


