A common dilemma in adult orthodontic treatment is deciding how best to treat missing posterior teeth. One treatment option is to orthodontically close the space. But closure can be difficult, especially if the open space is in the maxillary posterior area, because tooth movement through the maxillary sinus is limited. The increased difficulty of moving teeth in the maxillary sinus is similar to moving a tooth in the atrophic posterior mandibular ridge. If space closure is selected as a treatment method, proper mechanics and light forces should be applied. In this article, we report movement of teeth through the maxillary sinus and discuss various implications related to orthodontic treatment in the maxillary sinus.
The maxillary sinus, located in the body of the maxilla, is the largest and the first of the paranasal sinuses to develop. The development of the maxillary sinus starts about the third month of fetal life and ends its growth around 20 years of age with the eruption of the third molars. The maxillary sinus is typically pyramidal in shape with the base of the pyramid being the nasal antral wall, and its apex extending into the zygoma. It can be considered as having 3 walls, a floor, and a roof. The roof of the sinus is the floor of the orbit, and its floor is the alveolar process of the maxilla. The floor of the maxillary sinus is similar to cortical bone because it is a layer of compact bone lined with the periosteum.
In adults, the size of the maxillary sinus is variable in its extension. Its floor extends between adjacent teeth or individual roots in about half of the population, creating elevations in the antral surface or protrusions of root apices into the sinus. In these cases, the thickness of the sinus floor is noticeably reduced. According to a histologic study by Wehrbein and Diedrich, most roots that protrude radiographically into the sinus are actually enveloped by a thin cortical layer with perforations in 14% to 28% of the cases.
Maxillary premolar, molar, and occasionally canine roots can project into the maxillary sinus. Kwak et al reported that the topographic anatomy of the root apices of the maxillary molars are located closer to the inferior wall of the sinus than the premolar root apices. The distance from the root apex to the inferior sinus wall is the shortest in the second molar area. In orthodontics, when tooth roots protrude into the maxillary sinus, they can cause moderate apical root resorption and greater tipping during intrusive or horizontal movement of teeth across the sinus floor.
This case report presents a man, age 31 years 1 month, with maxillary sinus pneumatization from previous extractions. He was treated with bodily movement of teeth through the sinus floor.
Case report
A male patient, age 31 years 1 month, was referred to the clinic in Okayama, Japan, for evaluation of space closing of his missing teeth. He had a convex profile and a Class II skeletal pattern. He was in good general health and had no history of major systemic diseases or dental trauma. He reportedly had had 3 premolars extracted in preparation for orthodontic treatment when he was an adolescent but did not follow through with treatment because he could not afford it at that time.
He was missing 2 maxillary second premolars and the mandibular right first premolar. He had a deep overbite and a 5.5-mm overjet with a Class I molar relationship on the right side and a full Class II molar relationship on the left side, along with a mesiolingual rotation of his maxillary first molars. He also had a Class II canine relationship on both sides ( Fig 1 ).

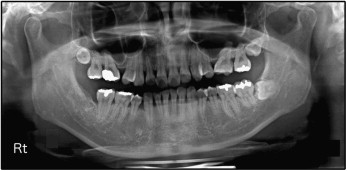
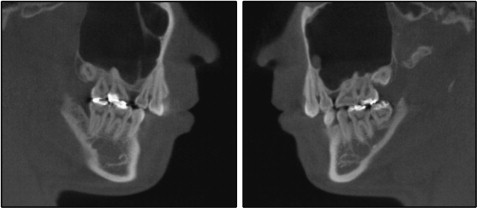
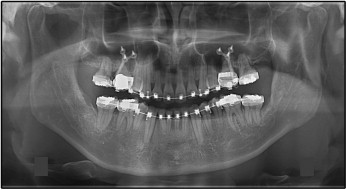
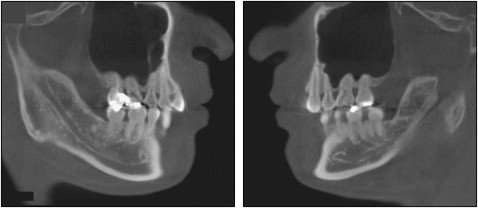
A panoramic radiograph showed no caries, and all third molars were present except for the mandibular right third molar. Some areas demonstrated blunted and short root apices. The maxillary first molars were tilted mesially. There was postextraction sinus pneumatization in both maxillary second premolar areas ( Fig 2 ). The relationship between the roots of the maxillary posterior teeth and the maxillary sinus was assessed by using cone-beam computed tomography (CBCT) ( Fig 3 ).
The treatment objectives were to obtain normal overbite and overjet, establish a Class I canine relationship, and close the spaces where the extracted teeth had been in the maxillary arch, with acceptable root parallelism.
After the initial orthodontic consultation, the patient was referred to an oral surgeon to extract all third molars. However, he wanted to have his third molars extracted after the leveling stage. Preadjusted appliances with 0.022-in self-ligating brackets (In-Ovation; GAC, Bohemia, NY) were bonded for leveling and alignment. The maxillary arch was leveled with continuous archwires, starting with 0.014-in nickel-titanium and working up to 0.019 × 0.025-in beta-titanium with 0.016 × 0.022-in titanium molybdenum alloy intrusion archwires ( Fig 4 ).

After 6 months of treatment, when the anterior bite was open, 0.022-in self-ligating brackets were bonded on the mandibular anterior segment. After 8 months of treatment, the patient chose skeletal anchorage system treatment to solve his dental problems. The skeletal anchorage system is composed of titanium anchor plates and monocortical screws that are temporarily placed in the jaw as absolute orthodontic anchorage. A Y-shaped anchor plate (Orthoanchor SMAP; Dentsply-Sankin, Tokyo, Japan) was bilaterally implanted at the zygomatic buttresses, and skeletal anchorage system mechanics were applied to upright the maxillary first molars and distalize the maxillary canines and first premolars. After approximately 1 year of skeletal anchorage system treatment, he finally had all his third molars extracted. The remaining maxillary anterior teeth were retracted with a T-loop while maintaining maximum anchorage on the posterior segments with the skeletal anchorage system ( Fig 5 ). During the finishing stage, final detailing of the occlusion was accomplished with 0.016 × 0.022-in steel archwires in conjunction with posterior up-and-down elastics ( Fig 6 ).
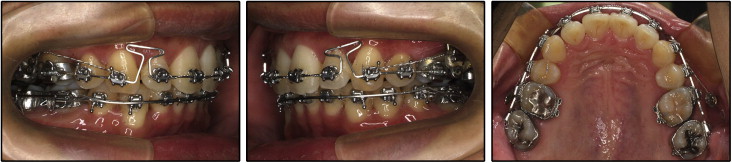
Fixed retainers were placed from canine to canine in the mandible and from lateral incisor to lateral incisor in the maxilla after debonding. Wraparound removable retainers were also delivered to secure the stability of both arches. Total treatment time for this patient was 30 months.
The posttreatment records indicate that the treatment objectives were achieved. A Class I canine relationship was established with a canine-protected occlusion, and acceptable overbite and overjet were achieved. The posterior spaces were successfully closed ( Fig 7 ).

The posttreatment panoramic radiograph shows proper space closure and acceptable root parallelism. There were no significant signs of bone resorption compared with pretreatment. However, some areas showed signs of apical root resorption ( Fig 8 ).

At the 1-year follow-up, the patient had a stable occlusion, and the orthodontic treatment results were maintained ( Fig 9 ). A 3-dimensional radiograph shows fairly stable results ( Fig 10 ).

Discussion
The shape and size of the maxillary sinuses can change because of many factors. One of the most common causes is when maxillary posterior teeth are extracted. This causes an inferior expansion of the maxillary sinus and leads to pneumatization of the sinus.
Pneumatization is a physiologic process that occurs in all paranasal sinuses during the growth period, causing them to increase in volume. Pneumatization of the sinus after extractions is an important consideration for diagnosis and treatment planning for dental implants, endodontic procedures, and orthodontic treatment. Wehrbein and Diedrich described a positive correlation between the length of root projection into the maxillary sinus as observed on panoramic radiographs and the amount of pneumatization after extraction. Sharan and Madjar reported that extraction of the maxillary second molars led to greater expansion than did extraction of the maxillary first molars. They also reported that extractions of 2 or more adjacent posterior teeth caused greater sinus expansion.
Pneumatization of the maxillary sinus also occurs when mandibular posterior teeth have been missing for a long time, resulting in overeruption of the opposing maxillary posterior teeth. In such situations, orthodontic molar intrusion with temporary anchorage devices might prevent invasive prosthodontic reduction with root canal treatment or posterior segmental osteotomy and thereby successfully intrude the maxillary posterior teeth through the maxillary sinus cortical floor.
The relationship between the roots of the maxillary posterior teeth and the maxillary sinus can be assessed by various techniques such as panoramic radiography and CBCT. Panoramic radiography is a commonly used imaging technique in dentistry because it allows visualization of various anatomic structures, is low cost, and has wide availability. It does have disadvantages that include convoluted images caused by superimposed anatomic structures, horizontal and vertical magnification, and a lack of cross-sectional information. CBCT overcomes these limitations by providing multiplanar images with uniform low magnification, but it has disadvantages that include higher doses of radiation, high cost, and limited availability. In our case study, the anatomic correlation between the dental roots and the alveolar bone was examined with both panoramic radiography and CBCT.
The topography of the inferior wall with the maxillary root apices varies according to a patient’s age, size, amount of pneumatization of the maxillary sinus, and status of dental retention. The thickness of the inferior wall of the sinus and its relationship with the adjacent teeth is crucial for orthodontic tooth movement. This information provides a basis for the application of appropriate forces in orthodontic tooth movement and predicting the amount of tooth movement through the maxillary sinus.
Knowledge of the cortical thickness of the buccal and palatal alveolar plates plus the inferior wall thickness of the maxillary sinus is important in periapical surgery or dental implantation. Kwak et al reported that the distance between the apex of the buccal root and the buccal alveolar plate was shortest in the maxillary first premolar area and longest on the mesiobuccal root in the maxillary second molar area.
Considering the topographic anatomy of the maxillary sinus, it is still debatable whether orthodontic movement can be done through the dense cortical bone of the maxillary sinus. Wehrbein et al reported that orthodontic movement through the maxillary sinus was limited, but other authors reported that teeth can move through the anatomic limitations such as cortical bone, suture, or sinus.
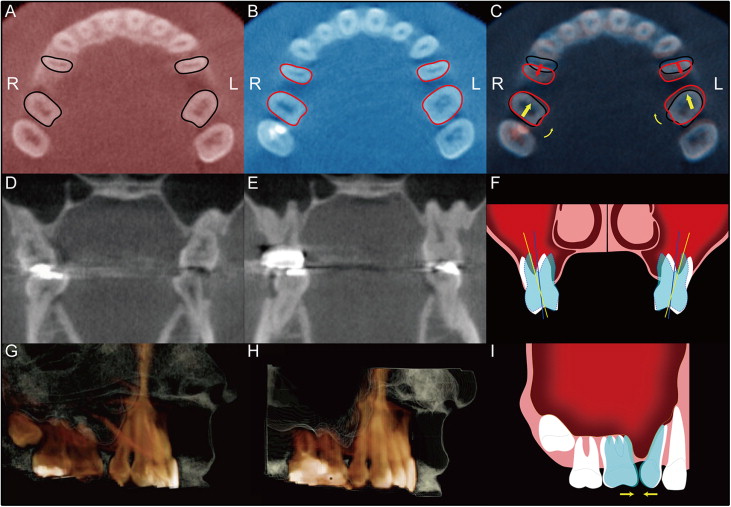
From our study, the representative CBCT scans showed the following: the axial section images were obtained by making a cut at the maxillary first molar cementoenmael junction level. Red and blue color images show pretreatment and posttreatment, respectively. Tooth movement was demonstrated by superimposing the pretreatment and posttreatment images. According to this, the first molars rotated mesially and moved slightly forward through the maxillary sinus, whereas the first premolars moved distally ( Fig 11 , A-C ).