Oral squamous cell carcinoma traditionally affects older men who smoke and drink. A change in this profile has been reported because of an increased incidence in young nonsmoking and nondrinking patients. The purpose of this article was to describe a series of young nonsmoking and nondrinking patients diagnosed with tongue squamous cell carcinoma who had recently received orthodontic treatment or evaluation. Details regarding diagnosis, treatment, follow-up, and disease evolution are presented, with a review of the pertinent literature. Orthodontists often treat young adults, who have frequent dental appointments and long-term follow-ups. Thus, practitioners should pay special attention to young patients during dental consultations, since the incidence of malignant oral lesions in this segment of the population seems to be increasing.
Squamous cell carcinoma (SCC) accounts for more than 90% of all oral malignancies; it is most common in men in their sixth and seventh decades of life who have used tobacco and alcohol for long periods.
In the overall population, the most common anatomic site for oral SCC is the lower lip, and the intraoral site with the highest incidence is the lateral border of the tongue, followed by the floor of the mouth, the soft palate, the retromolar area, and the gingiva. Early recognition of oral SCC appears to confer a survival advantage and is also associated with less morbidity and requires less mutilating surgery. In this context, several potentially malignant lesions can progress to oral SCC. The 3 most often seen potentially malignant oral lesions are actinic cheilitis, a reddish swelling induced by chronic exposure to sunlight that precedes lower-lip SCC; erythroplakia (red patch), the type of lesion most likely to progress to carcinoma; and leukoplakia (white patch), which can present clinically as nodular leukoplakia, speckled leukoplakia (erythroleukoplakia), or proliferative verrucous leukoplakia. Oral SCC may also present clinically as leukoplakia or erythroplakia but is mainly seen as indurated ulcers or lumps, granular ulcers with tissue infiltration and raised exophytic margins, or a nonhealing extraction socket. Thus, clinicians should be aware when any of these features persist for more than 2 weeks because it might be a sign of oral malignancy.
Recently, evidence based on research in several countries has shown an important increase in the incidence of these tumors among young patients. Despite this evidence, oral SCC and potentially malignant disorders are still considered uncommon in young patients, although one cannot deny the difficulties involved for general practitioners to be able to correctly interpret these lesions, which could result in underestimation of their prevalence during dental care. Thus, oral SCC is generally only diagnosed in more advanced stages and then requires more aggressive treatment, and the prognosis is also worse. However, there are still controversies regarding the prognosis of oral SCC in younger people. Some studies report a favorable clinical prognosis, whereas others show a worse prognosis for young people. Only a few studies have so far focused on gaining a better understanding of oral cancer in young patients. Therefore, the aim of this article was to describe 3 clinical cases of oral SCC diagnosed in nonsmoking and nondrinking patients under 40 years of age who attended an oral medicine center within a short time frame. Interestingly, all the patients had recent orthodontic treatment or evaluation. In addition, a literature review was undertaken to provide more information about the emerging issue of oral SCC in young patients.
Case reports
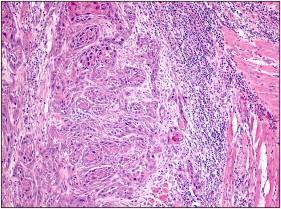
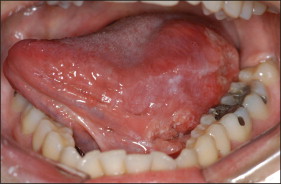
Patient 1 was a 21-year-old white woman, a nonsmoker and nondrinker in the final stage of orthodontic treatment ( Fig 1 ), who came to our clinic at Piracicaba Dental School, Piracicaba, São Paulo, Brazil, complaining about a white spot on her tongue. She reported a mildly uncomfortable sensation associated with the lesion, which had evolved over 6 months. She mentioned that she had asked the orthodontic staff about the lesion and was told that it was not a significant lesion. The intraoral examination showed an erythroleukoplakia on the left lateral border of the tongue, measuring approximately 2.0 × 2.0 cm ( Fig 2 ). An incisional biopsy was performed, and histopathologic analysis showed nests and cords of atypical hyperchromatic and pleomorphic epithelial cells invading deep connective tissue. Atypical mitoses were found in several areas of the analyzed tissue ( Fig 3 ). Thus, the diagnosis of SCC was confirmed, and the patient was referred for medical treatment. Additional examinations did not identify any regional or distant metastases, and the clinical staging of the patient at diagnosis was a T1N0M0 classification. (T describes the size of the primary tumor, N describes regional lymph nodes that are involved, and M describes distant metastasis.) Treatment consisted of a left partial glossectomy associated with homolateral supraomohyoid neck dissection. A reconstruction was immediately performed with microsurgery grafting using a mucocutaneous flap from her left biceps. The patient is still under follow-up and has shown no recurrence or metastasis after 48 months.


Patient 2 was a 34-year-old white man, a nonsmoker and nondrinker, who was referred from a physician to our clinic. He had completed orthodontic treatment with fixed appliances 4 years earlier, but he was not under postorthodontic follow-up. The intraoral examination showed an infiltrative ulcer on the right lateral border of the tongue, and the main diagnostic hypothesis was SCC. The lesion was approximately 4.0 × 3.0 cm in size and was painful on palpation ( Fig 4 ). The diagnosis of oral SCC was confirmed through incisional biopsy and histopathologic analysis. The patient was referred to medical staff, who staged his tumor as T2N0M0. However, he refused the therapeutic proposal of a partial glossectomy with supraomohyoid neck dissection. The patient, of his own accord, went to another physician, who performed a “conservative surgery” with an intraoral approach and without cervical dissection. The histopathologic examination of the surgical sample detected compromised surgical margins, which led the patient to postoperative radiotherapy. However, he also refused adjuvant radiotherapy. The patient died 10 months after the diagnosis from local persistence of the disease and cervical metastasis.

Patient 3 was a 29-year-old white woman, a nonsmoker and nondrinker, who came to our clinic complaining of “a wound on the tongue” that she had observed after an initial orthodontic evaluation, approximately 40 days before coming to our clinic ( Fig 5 ). The lesion was associated with a mildly uncomfortable sensation. The intraoral examination identified a 5.0 × 4.0-cm ulcer on the left lateral border of the tongue, with infiltration to the floor of the mouth and imprecise limits ( Fig 6 ). An incisional biopsy was performed, and histopathologic analysis detected an intense proliferation of atypical epithelial tissue, atypical dyskeratosis, and mitoses associated with necrotic areas, confirming the clinical impression of SCC. She was referred for treatment with medical staff, who staged her tumor as T3N2M0 and performed a left hemiglossectomy associated with bilateral supraomohyoid dissection and postoperative radiotherapy (total dose of 6.100 cGy). The patient had pulmonary metastasis 12 months after treatment and cervical metastasis 16 months after diagnosis. She is currently being treated by palliative chemotherapy in an attempt to control the disease.

Discussion
There are several variations in the literature regarding the criteria for defining a young patient with oral SCC. Apparently, most of the published studies have established the age limit as 40 years. However, many studies have considered age 45 years as the limit. Interestingly, the analyses that considered patients under the age of 45 years found risk factors, sex prevalence, and clinical stages similar to those described for oral SCC in elderly patients. This finding suggests that the ideal age for considering a patient as young for oral SCC is 40 years.
From 1960 to 1990, the incidence of tongue SCC in young Scandinavian adults, ages 20 to 39 years, increased by 5-fold among men and 6-fold among women, diminishing the ratio between the sexes, whereas for elderly patients the values doubled in both sexes. Similarly, patients up to 35 years of age, from different French medical centers, showed a male-to-female ratio of 1.88:1; the normal ratio for elderly patients in France is 10:1. More recently, Patel et al, when studying trends in oral SCC from 1975 to 2007 in the United States, showed that the prevalence of tongue SCC is increasing among young white people 18 to 44 years of age, particularly among women. Thus, according to these authors, young white women might be a new, emerging head and neck cancer-patient population. Interestingly, the mean age at diagnosis of our case series was 28 years (range, 21-34 years); although small, our sample clearly shows some characteristics described above for the clinical profiling of young patients with oral SCC.
Apparently, there are no individualized treatment protocols for young patients with oral SCC; thus, the therapeutic approaches follow the models used for elderly patients (surgery, radiotherapy, and, occasionally, chemotherapy) and are based on the same criteria. Remarkably, recent results have suggested that the lack of a specific treatment protocol could be associated with a negative impact on the prognosis and survival of young patients with oral SCC. The same authors suggested that physicians could be influenced by these patients’ young age during surgical planning; this would cause incomplete tumor resections in an attempt to preserve functioning. As an additional challenge, the small numbers of oral SCC in the young population limits medical experience.
It is suggested that several factors could be related, to a greater or lesser degree, to the clinical behavior of oral SCC in young patients. Among them are a possible enhanced genetic susceptibility to tumors, increased genomic instability, human papillomavirus (HPV) infection, and inadequate therapeutic approaches (conservative surgical procedures).
HPV infection with high-risk types 16 and 18 has been widely reported as a prominent mechanism behind the development of SCC of the oropharynx. However, the role of HPV in the development of oral SCC is still a matter of debate, especially in young patients.
It is difficult to determine whether young adults with oral SCC represent a spectrum or are a distinct group of head and neck cancer patients. Apparently, it seems more likely that they are both, falling into 3 major groups: (1) those in the 40- to 45-year age group who report a high level of risk-factor exposure (tobacco and alcohol) might simply be a continuation of the spectrum seen in older patients; (2) men with oropharyngeal cancer, including many nonsmokers, some of whom are 45 years old, but most are somewhat older, who are an emerging group related to a high risk for HPV infection; and (3) a third distinct group of 40-year-old patients, usually female nonsmokers, with oral cancer. It has been suggested that HPV must be a factor in the latter group, but some studies indicate otherwise. So far, the principal findings in molecular studies of young patients with oral SCC are that the tumors developing in these patients are markedly different at a genetic level, with some studies reporting that high risk for HPV infection might play an important role in carcinogenesis in this group.
Reports suggest that tumors with HPV positivity show improved survival rates, although consensus has yet to be achieved. Further studies to establish the real risk of HPV in the development and clinical behavior of oral SCC in young patients are needed.
Most importantly, the moment of diagnosis is of major importance for a good prognosis, but oral SCC in young patients seems to be frequently diagnosed in its advanced stages, which greatly compromise treatment, quality of life, and survival rates.
The histories of the patients described here illustrate our points in this discussion. Patient 1 was undergoing long-term orthodontic treatment when, independently, her lesion was identified. As an aggravating circumstance, even though she considered it an uncommon oral alteration, the lesion was underestimated by her orthodontic staff. Furthermore, she was not referred for a specialized evaluation. This finding exposes the apparent limitations of many dental clinicians who, during their consultations, do not perform systematic oral examinations on their patients. This evidently impairs the identification of oral lesions, especially lesions located on less-visible anatomic regions, such as the lateral border of the tongue. Nevertheless, the fact that the patient persisted in looking for help and was thus diagnosed at an early stage of the disease probably explains her favorable outcome. Unfortunately, this was not the case with patient 3, who was diagnosed at an advanced stage of the disease. Patient 2, despite his favorable stage of disease at the diagnosis (T2N0M0), died because of the persistence of the disease, which was incompletely treated. This clinical situation suggests that psychosocial factors can motivate young patients to refuse the treatment, negatively influencing the clinical evolution of the disease and, as a consequence, the prognosis.
Analysis of the cases presented in this article, in light of the relevant literature, suggests that oral SCC in young patients is an important issue in contemporary dental practice and that it might represent a distinct clinical entity because of its apparent increase in nonsmoking and nondrinking women. Most importantly, systematic oral examinations are a simple, inexpensive, and potentially important tool for promoting oral and general health.
Recent case reports have strengthened the importance of systematic oral examinations in patients undergoing orthodontic treatment, especially because orthodontists are considered to be well-placed dental specialists to recognize oral lesions at their initial stages of development, since their treatments require frequent dental appointments and long-term follow-ups.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


