Introduction
The aim of this clinical study was to investigate the skeletal, dentoalveolar, and soft-tissue effects of 2 skeletal anchorage rationales for Class III treatment compared with an untreated Class III control group.
Methods
Fifty-one subjects who were in the prepubertal or pubertal growth period were included in the study. In group 1 (n = 17), facemasks were applied from miniplates placed in the lateral nasal walls of the maxilla, and intermaxillary Class III elastics were applied from symphyseal miniplates to a bonded appliance on the maxilla in group 2 (n = 17). These skeletal anchored groups were compared with an untreated control group (n = 17). Lateral cephalometric radiographs were obtained at the beginning and the end of the observation periods in all groups and analyzed according to the structural superimposition method. Differences between the groups were assessed with the Wilcoxon signed rank test or the paired-samples t test.
Results
The treatment periods were 7.4 and 7.6 months in groups 1 and 2, respectively, and the untreated control group was observed for 7.5 months. The maxilla moved forward by 3.11 mm in group 1 and by 3.82 mm in group 2. The counterclockwise rotation of the maxilla was significantly less in group 1 compared with group 2 ( P <0.01). The mandible showed clockwise rotation and was positioned downward and backward in the treatment groups, and it was significantly greater in group 2 compared with group 1 ( P <0.01). Changes in the maxillary incisor measurements were negligible in group 1 compared with group 2. A significant amount of mandibular incisor retroclination was seen in group 1, and a significant proclination was seen in group 2. The maxillomandibular relationships and the soft-tissue profiles were improved remarkably in both treatment groups.
Conclusions
The protocols of miniplates with facemasks and miniplates with Class III elastics offer valid alternatives to conventional methods in severe skeletal Class III patients. However, the 2 maxillary protraction protocols demonstrated significant skeletal and dentoalveolar effects. The miniplate with facemask protocol is preferred for patients with severe maxillary retrusion and a high-angle vertical pattern, whereas in patients with a decreased or normal vertical pattern and retroclined mandibular incisors, miniplates with Class III elastics can be the intraoral treatment option. Therefore, the exact indication of the procedure should be considered carefully.
Skeletal Class III malocclusions originating from maxillary retrognathia are treated with protraction of the maxilla in growing children. The effects of conventional facemask therapy via tooth anchorage include counterclockwise rotation and forward displacement of the maxilla, clockwise rotation of the mandible, mesialization and extrusion of the maxillary molars, proclination of the maxillary incisors, and retroclination of the mandibular incisors. Indirect application of force not only limits the potential for orthopedic change but also causes undesirable tooth movements.
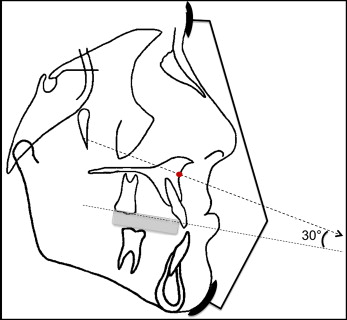
Researchers have attempted to use facemasks with temporary anchorage devices to eliminate side effects and increase the skeletal effects. In this way, orthopedic force can be directly transferred to the nasomaxillary complex. Placing the miniplates laterally to the nasal walls of the maxilla allows the protraction force vector to pass through the center of resistance of the nasomaxillary complex, and protraction of the maxilla is expected without a significant rotation. According to Tanne et al and Hirato, the center of resistance of the nasomaxillary complex is located between the root tips of the maxillary first and second premolars, whereas Miki found it to be between the first and second premolars in the posteroanterior direction and between the orbit and the distal root apex of first molars vertically. Staggers et al found it to be at the level of the zygomatic buttress. Moreover, according to Hata et al, the center of resistance of the maxilla is located 5 mm above the nasal floor.
Studies in which protraction facemasks were applied with miniplates have demonstrated significant amounts of maxillary protraction along with the elimination of dental side effects and decreases in the counterclockwise rotation of the maxilla.
Since the protraction facemask is applied extraorally and needs total patient cooperation at least 16 hours a day for 8 to 12 months, researchers have tended to use intraoral methods in recent years. De Clerk et al were the first researchers to apply intermaxillary Class III elastics from symphyseal miniplates to zygomatic miniplates for the treatment of skeletal Class III malocclusions. It was thought that with this approach, an extraoral facemask is no longer needed because intermaxillary traction can be applied 24 hours a day. After 2009, the same group of researchers published articles regarding the 3-dimensional outcomes of bone-anchored Class III elastics in a larger sample. Cevidanes et al compared the treatment effects for maxillary advancement induced by bone-anchored maxillary protraction and facemask with rapid maxillary expansion (RME). They reported that with the bone-anchored maxillary protraction protocol, significantly greater amounts of maxillary advancement were achieved compared with a facemask and RME.
According to a systematic review that compared the effectiveness of maxillary protraction with a temporary anchorage device with tooth-anchored maxillary protraction, it was concluded that maxillary protraction with a temporary anchorage device might have a greater effect on maxillary advancement and reduce the skeletal and dental side effects compared with tooth-anchored maxillary protraction.
Although the idea of obtaining more protraction of the maxilla is tempting and the results are promising, the surgical procedure is the main drawback of bone-anchored maxillary protraction.
This is the first study to comparatively evaluate the effects of symphyseal miniplate-anchored Class III elastic traction and miniplate-anchored protraction facemask treatment with an untreated Class III control group.
Material and methods
A total sample of 48 (16 per group) was required for a power of 85% at the 5% significance level. Sample size estimation was performed using PASS 2000 software (NCSS LLC, Caysville, Utah).
Fifty-one patients from orthodontic department of Başkent University, Ankara, Turkey, were included in this study. All subjects were between PP2= and MP3cap developmental stages at the initial observation (T1) according to their hand-wrist radiographs. The first 2 groups were constituted prospectively and compared in a retrospective manner.
The inclusion criteria were (1) skeletal and dental Class III malocclusion with maxillary deficiency (ANB, <0°; Nperp-A, <0 mm) and retrusive nasomaxillary complex with or without mandibular prognathia, (2) vertically normal or low growth pattern (SNGoGn, <40°), (3) anterior crossbite and Angle Class III molar relationship, and (4) normal or increased overbite. All subjects and parents were informed of the surgical procedure and signed an informed consent form, and the study was approved by the ethics committee of Başkent University, with the project numbers D-KA06/07 and D-KA10/04.
All patients were treated by 2 operators (C.S. and Z.S.) at the same university clinic until 4 to 5 mm of overjet was achieved. Before maxillary protraction in the treatment groups, a bonded RME appliance was applied, and the expansion screw (1114/10; Lewa-Dental, Remchingen, Germany) was activated twice a day for a week until the midpalatal suture was disturbed. The expansion was continued with a semirapid protocol (RME for 7 days, followed by slow maxillary expansion) in patients who still had a transverse deficiency, until adequate expansion was achieved. The major goal of applying the RME appliance is to disrupt the circummaxillary sutures and stimulate forward displacement of the maxilla.
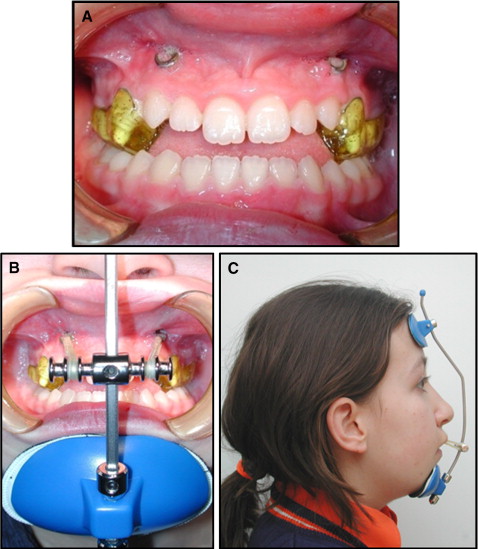
Group 1 (n = 17) consisted of patients treated with a miniplate-anchored orthopedic facemask. In each patient, 2 miniplates were inserted in the lateral nasal walls of the maxilla, and the facemasks were applied from 2 titanium miniplates (OsteoMed, Addison, Tex). An incision was made at the labial vestibule between the maxillary lateral incisors and canines, and a mucoperiosteal flap was elevated to expose the lateral nasal wall of the maxilla on both sides. The miniplates were adapted according to the anatomic shape of the apertura piriformis area and fixed in place with 2 monocortical miniscrews. Then the incisions were sutured with 3.0 polyglactin 910, exposing the third hole into the oral cavity ( Fig 1 ). After soft-tissue healing for 7 days, extraoral elastics of 400 g were applied from the miniplates to the facemasks ( Figs 2 and 3 ). The patients were asked to replace the elastics once a day and to wear the facemasks at least 16 hours a day.

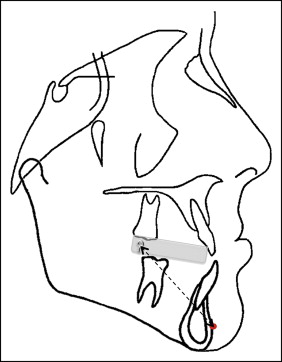
Group 2 (n = 17) was treated with Class III intermaxillary elastics from 2 titanium miniplates (55.MAN.003; Trimed, Ankara, Turkey) placed in the symphyseal region to a bonded RME appliance. The triangular-shaped titanium miniplates, used for orthodontic anchorage with 3 holes, were placed under local anesthesia. An incision was made at the labial vestibule between the mandibular lateral incisors and canines, and a mucoperiosteal flap was elevated to expose the cortical bone between the lateral incisor and the canine. It is crucial not to damage the roots of the permanent canines. Miniplates were shaped according to the anatomic structures, and the extensions of the miniplates were bent mesially to apply Class III elastics. The miniplates were fixed with 3 monocortical miniscrews. The incisions were sutured with 3.0 polyglactin 910, exposing the attachment arm through the attached gingiva near the mucogingival junction.
After a week to allow soft-tissue healing, 500 g of protraction force was applied with elastics from the extensions of the miniplates to the hooks of the bonded maxillary expansion appliance ( Figs 4 and 5 ). The patients were instructed to maintain good oral hygiene and wear the elastics 24 hours per day.

All surgical procedures in groups 1 and 2 were done by the same oral surgeon (S.U.).
In order to differentiate the treatment changes from normal growth changes, the third group was the untreated control group (n = 17). These subjects were matched to those in the treatment groups.
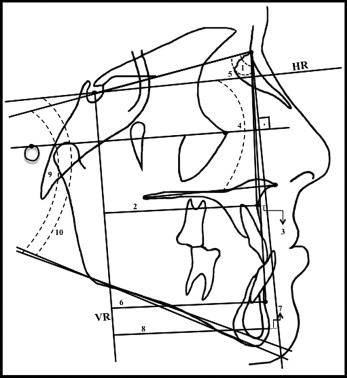
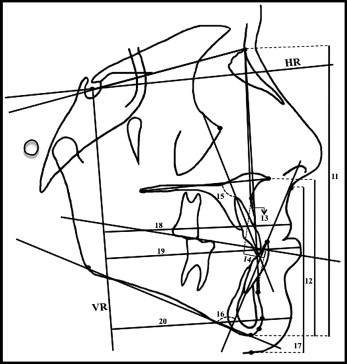
Lateral cephalograms were obtained at T1 and at the end of protraction therapy or the observation period (T2) in all groups. All cephalograms were hand traced and measured on a conventional light box by the same investigator (Z.S.), who repeated the measurements at 3-week intervals to ensure measurement accuracy using paired t tests. Horizontal and vertical reference planes were used to make the linear measurements. The horizontal reference plane was constructed by subtracting 7° from the sella-nasion line, and a vertical line passing through sella and perpendicular to the horizontal reference plane was used as the vertical reference plane.
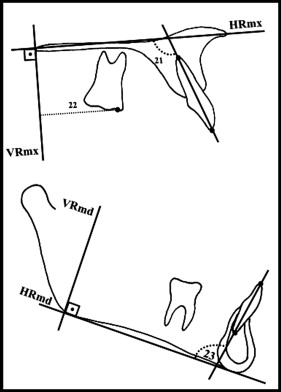
Lateral cephalometric radiographs obtained at T2 were superimposed on those at T1 by means of the total structural superimposition method as described by Bjork and Skieller. In addition, maxillary and mandibular regional superimpositions were done to measure the movement of the maxillary and mandibular dentitions relative to their basal bones. Maxillary regional superimpositions were made on the best fit of the lingual curvature of the palatal plate and internal bony structures. A maxillary horizontal line was defined as the line drawn along the anterior nasal spine and the posterior nasal spine, and a vertical line passing through posterior nasal spine and perpendicular to the maxillary horizontal line was used as the maxillary vertical line. Mandibular superimpositions were made on stable mandibular structures. A line passing through gonion and gnathion was used as the mandibular horizontal line, and the mandibular vertical line was defined as the line passing through gonion and perpendicular to the mandibular horizontal line. The degree of mandibular rotation was evaluated by measuring the angle between the sella-nasion lines of T1 and T2 radiographs on the superimposed tracings.
Cephalometric landmarks, reference planes, and measurements are shown in Figures 6 through 8 .
Statistical analysis
Data analysis was performed using SPSS for Windows (version 11.5; SPSS, Chicago, Ill). Whether the distributions of continuous variables were normal was determined by the Kolmogorov-Smirnov test. The Levene test was used for determining the homogeneity of the variances. Data were shown as means and standard deviations or medians, where applicable. The mean differences among the groups were compared with 1-way analysis of variance (ANOVA), and the Kruskal-Wallis test was applied for comparisons of the median values. When the P values from the 1-way ANOVA or Kruskal-Wallis test were statistically significant, the post hoc Tukey HSD or the Conover nonparametric multiple comparison test was used to determine which group differed from the others. Whether the mean differences between measurement times were statistically significant was evaluated by the paired-samples t test; otherwise, the Wilcoxon signed rank test was applied for comparisons of the median values. A P value less than 0.05 was considered statistically significant. In all possible multiple comparison tests, the Bonferroni adjustment was applied for controlling type I error.
To assess the reliability of the measurements, 3 weeks after the first measurements, 40 lateral cephalometric films of 20 randomly selected patients were analyzed by the same examiner (Z.S.). The intraclass correlation coefficients (ICCs) (r) were calculated for each variable in the T1 and T2 cephalograms, and the r values for each variable ranged between 0.911 and 1.000. Confidence intervals of 90% were considered statistically reliable. Table I presents the raw measurement errors for each parameter.
| Variable | T1 | T2 | ||||
|---|---|---|---|---|---|---|
| ICC | Lower limit | Upper limit | ICC | Lower limit | Upper limit | |
| SNA (°) | 0.993 | 0.998 | 1.000 | 0.999 | 0.999 | 1.000 |
| A-VR (mm) | 1.000 | 0.999 | 1.000 | 1.000 | 0.999 | 1.000 |
| Nperp-A (mm) | 0.997 | 0.995 | 0.994 | 0.994 | 0.988 | 0.997 |
| HR.PP (°) | 0.996 | 0.992 | 0.998 | 0.991 | 0.983 | 0.995 |
| SNB (°) | 1.000 | 0.999 | 1.000 | 0.999 | 0.997 | 0.999 |
| B-VR (mm) | 1.000 | 0.995 | 1.000 | 0.999 | 0.999 | 1.000 |
| Nperp-Pg (mm) | 0.991 | 0.994 | 0.998 | 0.995 | 0.991 | 0.998 |
| Pg-VR (mm) | 1.000 | 0.999 | 1.000 | 0.999 | 0.998 | 1.000 |
| SN.GoGn (°) | 0.999 | 0.997 | 0.999 | 0.998 | 0.996 | 0.999 |
| HR.GoMe (°) | 0.998 | 0.997 | 0.999 | 0.999 | 0.997 | 0.992 |
| N-Me (mm) | 1.000 | 0.999 | 1.000 | 1.000 | 1.000 | 1.000 |
| ANS-Me (mm) | 0.999 | 0.998 | 1.000 | 1.000 | 1.000 | 1.000 |
| ANB (°) | 0.997 | 0.995 | 0.992 | 0.997 | 0.994 | 0.998 |
| Wits (mm) | 0.953 | 0.911 | 0.976 | 0.997 | 0.994 | 0.998 |
| Overjet (mm) | 0.997 | 0.995 | 0.999 | 0.997 | 0.994 | 0.994 |
| Overbite (mm) | 0.998 | 0.995 | 0.999 | 0.998 | 0.995 | 0.999 |
| U1.PP (°) | 0.997 | 0.995 | 0.999 | 0.997 | 0.995 | 0.999 |
| L1.MP (°) | 1.000 | 1.000 | 1.000 | 0.998 | 0.996 | 0.993 |
| U1.HRmx (°) | 0.998 | 0.995 | 0.996 | 0.999 | 0.997 | 0.999 |
| U6-VRmx (mm) | 0.997 | 0.995 | 0.997 | 0.997 | 0.994 | 0.993 |
| L1.HRmd (°) | 0.998 | 0.997 | 0.999 | 1.000 | 0.999 | 1.000 |
| Sn-Me′ (mm) | 0.998 | 0.997 | 0.991 | 0.997 | 0.995 | 0.999 |
| UL-VR (mm) | 0.999 | 0.998 | 0.999 | 0.999 | 0.998 | 0.999 |
| LL-VR (mm) | 1.000 | 0.999 | 1.000 | 1.000 | 0.999 | 1.000 |
| Pg′-VR (mm) | 1.000 | 0.999 | 1.000 | 0.999 | 0.991 | 0.999 |
Results
There were no statistically significant differences between the groups at T1 for the analyzed parameters. Table II shows the mean values of the measurements at T1 and the comparison of the 3 groups. The differences between the changes from T2 to T1 in all groups are shown in Table III .
| Parameter | MP+FM (Group 1) Mean ± SD Median (range) |
MP+CI III Elastics (Group 2) Mean ± SD Median (range) |
Control Mean ± SD Median (range) |
|---|---|---|---|
| Chronologic age (y) | 11.23 ± 1.48 | 11.25 ± 1.52 | 9.87 ± 1.20 |
| Maxillary skeletal parameters | |||
| SNA (°) | 77.61 ± 3.12 | 76.05 ± 3.37 | 78.58 ± 3.36 |
| 77.00 (73.00-83.00) | 76.00 (70.50-82.00) | 78.00 (73.00-84.00) | |
| A-VR (mm) | 60.17 ± 3.96 | 58.88 ± 4.78 | 60.76 ± 3.06 |
| 61.00 (53.00-66.60) | 59.00 (52.50-68.50) | 61.50 (55.50-66.50) | |
| Nperp-A (mm) | −3.20 ± 1.91 | −3.85 ± 2.15 | −2.61 ± 2.40 |
| −3.00 (−7.00-0.00) | −3.00 (−8.00- −1.00) | −1.50 (−9.00-0.00) | |
| HR.PP (°) | 1.05 ± 2.60 | 3.76 ± 4.22 | 2.20 ± 2.37 |
| 1.00 (−4.00-6.00) | 3.00 (−5.00-13.00) | 2.00 (−2.00-6.00) | |
| Mandibular skeletal parameters | |||
| SNB (°) | 81.20 ± 2.93 | 80.67 ± 3.75 | 82.14 ± 3.08 |
| 80.00 (79.00-87.00) | 81.00 (76.00-89.00) | 82.00 (77.00-87.00) | |
| B-VR (mm) | 61.85 ± 6.07 | 61.38 ± 6.66 | 62.97 ± 4.66 |
| 61.50 (52.50-72.00) | 59.00 (51.50-78.00) | 64.00 (56.00-71.00) | |
| Nperp-Pg (°) | 1.38 ± 3.00 | 2.11 ± 2.33 | 1.32 ± 3.23 |
| 1.00 (−4.00-6.00) | 2.50 (−1.00-6.00) | 0.50 (−4.50-7.00) | |
| Pg-VR (mm) | 63.11 ± 6.88 | 62.08 ± 6.99 | 63.32 ± 5.44 |
| 61.50 (53.00-74.50) | 60.50 (51.00-80.00) | 63.50 (55.50-72.50) | |
| SN.GoGn (°) | 32.44 ± 4.76 | 32.64 ± 4.36 | 30.79 ± 4.31 |
| 32.00 (23.00-40.00) | 32.00 (23.00-39.50) | 30.00 (25.00-38.00) | |
| HR.GoMe (°) | 28.64 ± 4.92 | 28.82 ± 4.66 | 26.82 ± 5.59 |
| 29.00 (20.00-36.00) | 29.00 (19.00-36.00) | 25.50 (18.00-36.00) | |
| Facial heights | |||
| N-Me (mm) | 112.38 ± 7.00 | 112.14 ± 7.16 | 107.73 ± 5.44 |
| 113.00 (100.00-126.00) | 109.00 (103.50-129.00) | 106.00 (101.00-118.00) | |
| ANS-Me (mm) | 61.35 ± 5.82 | 59.91 ± 4.30 | 58.02 ± 4.00 |
| 62.00 (52.00-75.00) | 59.50 (54.50-70.00) | 58.00 (53.00-67.00) | |
| Maxillomandibular parameters | |||
| ANB (°) | −3.52 ± 1.86 | −4.61 ± 1.52 | −3.55 ± 2.19 |
| −3.00 (−7.50- −1.00) | −5.00 (−8.00- −2.50) | −3.00 (−9.00- −1.00) | |
| Wits (mm) | −9.44 ± 2.69 | −9.55 ± 2.89 | −8.76 ± 3.17 |
| −10.00 (−13.00- −4.00) | −9.50 (−16.00- −6.00) | −8.50 (−17.00- −3.50) | |
| Dentoalveolar parameters | |||
| Overjet (mm) | −3.26 ± 1.27 | −3.88 ± 1.53 | −3.70 ± 1.59 |
| −3.50 (−5.00- −0.50) | −4.00 (−6.50- −2.00) | −3.00 (−8.50- −2.00) | |
| Overbite (mm) | 4.00 ± 2.01 | 5.05 ± 2.92 | 4.50 ± 2.15 |
| 4.00 (0.50-8.50) | 5.00 (2.00-10.00) | 4.00 (1.00-9.00) | |
| U1.HRmx (°) | 109.47 ± 7.73 | 111.29 ± 7.46 | 110.61 ± 6.86 |
| 110.00 (96.00-120.00) | 109.00 (101.00-126.00) | 112.00 (99.00-122.00) | |
| U1.PP (°) | 109.47 ± 7.73 | 111.29 ± 7.46 | 110.61 ± 6.86 |
| 110.00 (96.00-120.00) | 109.00 (101.00-126.00) | 112.00 (99.00-122.00) | |
| U6-VRmx (mm) | 19.26 ± 4.22 | 21.41 ± 4.77 | 18.85 ± 1.05 |
| 19.50 (11.00-28.00) | 21.00 (13.50-31.00) | 19.00 (17.00-21.00) | |
| L1.HRmd (°) | 85.97 ± 6.68 | 87.94 ± 6.82 | 87.91 ± 7.28 |
| 85.00 (75.00-96.50) | 86.00 (75.00-104.00) | 87.00 (74.00-100.00) | |
| L1.MP (°) | 83.20 ± 7.13 | 84.70 ± 6.97 | 85.17 ± 7.38 |
| 82.00 (73.00-97.00) | 83.00 (71.50-101.00) | 84.00 (74.00-98.00) | |
| Soft-tissue parameters | |||
| Sn-Me′ (mm) | 62.94 ± 6.43 | 62.02 ± 3.76 | 61.29 ± 3.69 |
| 62.00 (55.00-78.00) | 61.00 (55.00-70.50) | 60.00 (57.00-70.00) | |
| UL-VR (mm) | 78.02 ± 5.75 | 77.26 ± 6.57 | 78.61 ± 4.04 |
| 78.00 (68.00-86.00) | 74.50 (68.00-91.00) | 78.00 (70.50-85.50) | |
| LL-VR (mm) | 79.44 ± 6.46 | 78.58 ± 7.53 | 79.97 ± 4.62 |
| 79.50 (69.00-91.00) | 75.50 (68.00-95.00) | 80.00 (70.00-88.00) | |
| Pg′-VR (mm) | 74.73 ± 7.11 | 73.35 ± 7.39 | 74.61 ± 5.84 |
| 74.00 (63.50-85.00) | 72.00 (62.50-93.00) | 76.00 (65.00-84.00) |
| Parameter | MP+FM (Group 1) Mean ± SD Median (range) |
P | MP+CI III Elastics (Group 2) Mean ± SD Median (range) |
P | P | Control Mean ± SD Median (range) |
P | 1-2 | 1-3 | 1-4 | 2-3 | 2-4 | 3-4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chronologic age (y) | 11.23 ± 1.48 | 11.25 ± 1.52 | 9.87 ± 1.20 | NS | NS | ∗ | NS | ∗ | NS | ||||
| Maxillary skeletal parameters | |||||||||||||
| SNA (°) | 3.14 ± 1.25 | ‡ | 3.14 ± 1.15 | ‡ | ‡ | 0.29 ± 1.43 | NS | NS | ∗ | ‡ | ∗ | ‡ | † |
| 3.00 (1.00-5.00) | 3.00 (1.50-5.50) | 0.50 (−2.50-3.00) | |||||||||||
| A-VR (mm) | 3.11 ± 0.94 | ‡ | 3.82 ± 1.45 | ‡ | ‡ | 0.32 ± 0.95 | NS | NS | † | ‡ | ‡ | ‡ | ‡ |
| 3.00 (1.50-5.00) | 3.50 (1.50-7.00) | 0.50 (−2.00-2.00) | |||||||||||
| Protraction rate (mm/mo) | 0.43 ± 0.15 | 0.53 ± 0.25 | 0.03 ± 0.14 | NS | † | ‡ | † | ‡ | ∗ | ||||
| 0.41 (0.17-0.75) | 0.54 (0.16-1.00) | 0.05 (−0.29-0.40) | |||||||||||
| Nperp-A (mm) | 3.14 ± 0.98 | ‡ | 3.94 ± 1.26 | ‡ | ‡ | −0.5 ± 0.93 | ∗ | NS | ∗ | ‡ | † | ‡ | ‡ |
| 3.50 (1.00-4.00) | 3.50 (2.00-6.50) | −0.5 (−2.50-1.50) | |||||||||||
| HR.PP (°) | −1.08 ± 1.25 | † | −2.55 ± 0.96 | ‡ | ‡ | −0.26 ± 0.56 | NS | † | ∗ | ∗ | NS | ‡ | ‡ |
| −1.00 (−4.00-1.00) | −3.00 (−4.50-1.00) | 0.00 (−1.00-0.50) | |||||||||||
| Mandibular skeletal parameters | |||||||||||||
| SNB (°) | −2.44 ± 1.04 | ‡ | −2.91 ± 0.81 | ‡ | ‡ | 1.08 ± 1.03 | † | NS | NS | ‡ | NS | ‡ | ‡ |
| −2.00 (−5.00- −1.00) | −3.00 (−4.50- −2.00) | 1.00 (−1.00-3.00) | |||||||||||
| B-VR (mm) | −3.26 ± 1.96 | ‡ | −4.20 ± 1.58 | ‡ | ‡ | 1.65 ± 1.04 | ‡ | NS | NS | ‡ | NS | ‡ | ‡ |
| −3.00 (−7.00-1.00) | −4.50 (−7.00- −1.00) | 2.00 (−1.00-3.00) | |||||||||||
| Nperp-Pg (°) | −3.05 ± 2.53 | ‡ | −3.41 ± 2.04 | ‡ | ‡ | 0.88 ± 1.06 | † | NS | NS | ‡ | NS | ‡ | ‡ |
| −3.50 (−7.00-2.50) | −3.00 (−8.00-0.50) | 1.00 (−0.50-3.00) | |||||||||||
| Pg-VR (mm) | −3.29 ± 2.01 | ‡ | −4.20 ± 1.64 | ‡ | ‡ | 2.02 ± 1.13 | ‡ | NS | NS | ‡ | NS | ‡ | ‡ |
| −3.50 (−6.00-2.00) | −4.50 (7.00- −1.00) | 2.50 (−1.00-3.50) | |||||||||||
| SN.GoGn (°) | 1.29 ± 1.04 | ‡ | 2.44 ± 0.68 | ‡ | ‡ | −0.88 ± 0.97 | † | † | ‡ | ‡ | NS | ‡ | ‡ |
| 1.50 (−2.00-2.50) | 2.50 (1.50-4.00) | −1.00 (–3.00-1.00) | |||||||||||
| HR.GoMe (°) | 1.23 ± 1.43 | † | 2.29 ± 1.10 | ‡ | ‡ | −0.76 ± 0.58 | † | ∗ | † | ‡ | NS | ‡ | ‡ |
| 1.00 (−1.00-4.00) | 3.00 (0.00-4.00) | −1.00 (−2.00-0) | |||||||||||
| Facial heights | |||||||||||||
| N-Me (mm) | 2.52 ± 1.65 | ‡ | 4.41 ± 1.66 | ‡ | ‡ | ∗ | † | NS | ∗ | NS | ‡ | ‡ | |
| 2.00 (1.00-7.00) | 5.00 (1.50-7.50) | 1.50 (–2.00-2.50) | |||||||||||
| ANS-Me (mm) | 2.61 ± 1.61 | ‡ | 4.23 ± 1.68 | ‡ | † | 0.14 ± 1.08 | NS | ∗ | NS | ‡ | NS | ‡ | ‡ |
| 2.50 (−1.00-5.00) | 4.00 (1.50-7.50) | 0.50 (−3.00-1.50) | |||||||||||
| Maxillomandibular parameters | |||||||||||||
| ANB (°) | 5.52 ± 1.56 | ‡ | 6.05 ± 1.24 | ‡ | ‡ | −0.79 ± 1.01 | † | NS | ∗ | ‡ | † | ‡ | ‡ |
| 6.00 (2.50-7.50) | 6.00 (4.00-8.00) | −1.00 (−2.50-1.00) | |||||||||||
| Wits (mm) | 7.08 ± 1.60 | ‡ | 10.52 ± 2.24 | ‡ | ‡ | −1.05 ± 1.57 | ∗ | ‡ | NS | ‡ | † | ‡ | ‡ |
| 7.50 (4.00-9.50) | 10.00 (7.50-16.00) | −1.5 (−3.00-2.00) | |||||||||||
| Dentoalveolar parameters | |||||||||||||
| Overjet (mm) | 7.79 ± 1.09 | ‡ | 6.61 ± 1.08 | ‡ | ‡ | −0.14 ± 0.52 | NS | ∗ | NS | ‡ | ∗ | ‡ | ‡ |
| 7.5 (6.00-10.00) | 7.00 (4.50-8.50) | 0.00 ( – 1.00-1.00) | |||||||||||
| Overbite (mm) | −1.29 ± 1.75 | NS | −4.29 ± 2.31 | ‡ | † | 0.61 ± 0.85 | ∗ | † | NS | ‡ | † | ‡ | ‡ |
| −1.50 (−4.50-2.50) | −4.00 (−7.50- −1.00) | 0.50 (−1.00-3.00) | |||||||||||
| U1.HRmx (°) | 0.14 ± 3.13 | NS | 3.76 ± 3.07 | ‡ | ∗ | 2.1 ± 1.76 | ‡ | † | NS | NS | NS | NS | NS |
| −1.00 (−7.00-5.00) | 3.50 (0.00-9.00) | 3.00 (0.00-5.00) | |||||||||||
| U1.PP (°) | −0.05 ± 4.72 | NS | 4.50 ± 3.12 | ‡ | ∗ | 1.91 ± 1.68 | ‡ | † | NS | NS | NS | NS | NS |
| 1.00 (−10.00-7.00) | 4.00 (0.00-11.00) | 2.00 (−0.50-5.00) | |||||||||||
| U6-VRmx (mm) | 0.17 ± 0.39 | NS | 4.50 ± 1.15 | ‡ | ‡ | 0.23 ± 1.03 | NS | ‡ | ‡ | NS | † | ‡ | ‡ |
| 0.00 (−0.50-1.00) | 4.50 (2.50-7.00) | 0.50 (−2.00-2.00) | |||||||||||
| L1.HRmd (°) | −6.91 ± 3.49 | ‡ | 9.23 ± 2.86 | ‡ | ‡ | 0.23 ± 2.40 | NS | ‡ | NS | ‡ | ‡ | † | † |
| −6.00 (−13.00-0.00) | 9.00 (4.00-16.00) | 0.00 (−4.00-4.00) | |||||||||||
| L1.MP (°) | −6.08 ± 3.35 | ‡ | 8.23 ± 2.81 | ‡ | † | −0.14 ± 2.14 | NS | ‡ | NS | ‡ | ‡ | † | † |
| −5.00 (12.00- −1.00) | 8.00 (3.50-15.00) | 0.00 (−4.00-3.00) | |||||||||||
| Soft-tissue parameters | |||||||||||||
| Sn-Me′ (mm) | 2.29 ± 2.22 | † | 4.08 ± 1.80 | ‡ | ‡ | 0.14 ± 1.56 | NS | † | NS | † | NS | ‡ | ‡ |
| 2.00 (−3.00-6.00) | 4.00 (0.50-7.00) | 0.00 (−3.50-2.00) | |||||||||||
| UL-VR (mm) | 3.55 ± 1.49 | ‡ | 3.61 ± 1.86 | ‡ | † | 1.08 ± 1.00 | † | NS | ∗ | ‡ | ∗ | ‡ | ∗ |
| 3.50 (1.00-7.00) | 3.50 (1.00-7.50) | 1.00 (−1.00-3.00) | |||||||||||
| LL-VR (mm) | −1.50 ± 1.88 | † | −1.55 ± 2.17 | † | ‡ | 1.79 ± 1.07 | ‡ | NS | NS | ‡ | NS | ‡ | ‡ |
| −1.50 (−5.50-1.50) | −2.00 (−6.00-3.00) | 2.00 (0.00-4.50) | |||||||||||
| Pg′-VR (mm) | −3.05 ± 2.03 | ‡ | −3.29 ± 1.93 | ‡ | ‡ | 2.02 ± 099 | ‡ | NS | NS | ‡ | NS | ‡ | ‡ |
| −3.00 (−6.50-0.50) | −4.00 (−5.50-1.00) | 2.00 (0.00-3.50) |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


