
1

Salivary Gland Anatomy
The salivary gland system of the upper aerodigestive tract plays a critical role in the functions of digestion, respiration, communication, and overall homeostasis. Two distinct types of glands compose this system. The major salivary glands are the paired parotid, submandibular, and sublingual glands. The remaining glands are the thousands of small minor salivary glands that line the oral cavity and can be found in the pharynx, supraglottis, nasal cavity, and paranasal sinuses. These glands produce saliva, which functions in digestion, immunity, dental hygiene, lubrication, and hydration. This chapter will review the anatomical relationships of the salivary glands relevant for surgical management of neoplastic and non-neoplastic salivary gland disorders, as well as other processes that may involve the glands secondarily. The histology of salivary glands will be discussed in detail in Chapter 4.
 Parotid Gland
Parotid Gland
The parotid gland, weighing 15 to 30 g, is the largest of the salivary glands and is a slender, lobulated gland. The parotid glands are positioned on the lateral aspect of the face overlying the posterior surface of the mandible and anteroinferiorly to the auricle (Fig. 1–1). The lateral surface of the gland consists of fascia that forms a dense capsule. This fascia also covers the masseter muscle and is referred to as the parotidomasseteric fascia. John Conley1 describes four “dorsal investments of fascia” at the posterior border of the gland: (1) The fascia superior to the tragus is thick and partially attaches to the root of the zygoma. The temporal artery and vein and auriculotemporal nerve can be found there. (2) There is a thin fascia along the tragal and conchal cartilage that separates easily with blunt dissection. (3) The fascia is thick again as it attaches to the mastoid process. (4) There is a confluent thickening of the fascia at the inferior tip of the parotid gland separating it from the submandibular gland.
The gland has a small superior surface and larger anteromedial, posteromedial, and superficial surfaces. The superior border is the zygomatic arch. The anterior border is the masseter muscle. The posterior border is the tragal cartilage and the anterior border of the sternocleidomastoid muscle. The gland has a so-called tail, which is located posteriorly between the ramus of the mandible and the sternocleidomastoid muscle. This region overlies the digastric muscle. The inferior border of the parotid gland is variable and extends along the anterior border of the sternocleidomastoid muscle and the carotid sheath. Anteromedially, the gland is attached to the masseter muscle, the posterior border of the mandibular ramus, and the medial pterygoid muscle. Posteromedially, the gland is adjacent to the posterior belly of the digastric muscle, the styloid process, and its associated muscles and ligaments. Deeply, portions of the parotid gland rest in the prestyloid compartment of the parapharygeal space.
There has been much debate as to whether or not the parotid gland truly has a superficial and deep lobe. A traditional approach is to divide the gland into a superficial and deep lobe based on the course of the facial nerve as it travels through the gland (Fig. 1–2). This approach is particularly useful in defining the type of surgical resection that is undertaken. The superficial lobe is defined as parotid tissue located lateral to the facial nerve. The deep lobe is the remaining gland located medial to the facial nerve. Most benign tumors of the parotid gland are located in the superficial lobe and can be resected with a superficial parotidectomy. However, it is not uncommon to discover that masses that were initially diagnosed as superficial based on physical examination are actually located in the deep lobe.
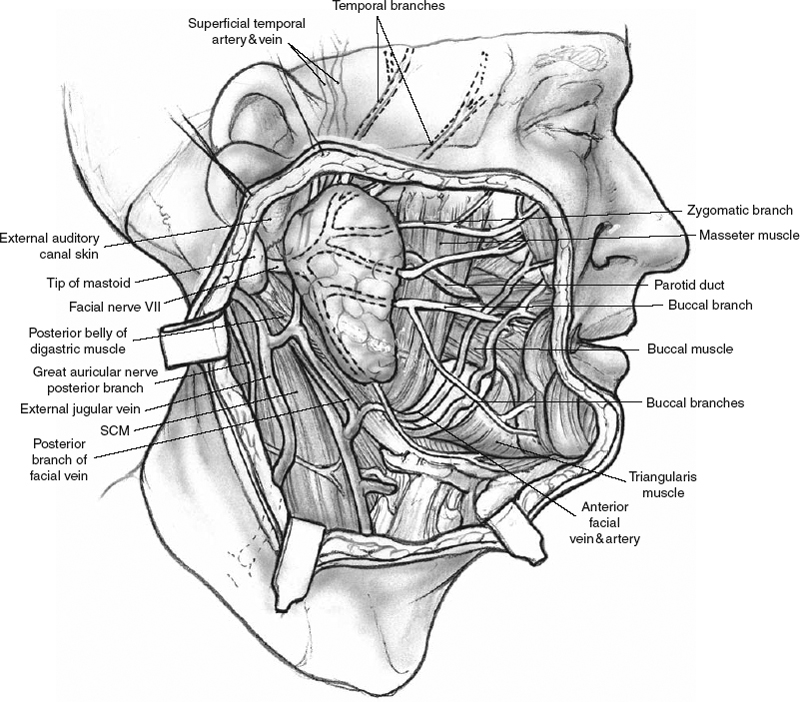
Figure 1-1 Lateral view of the face showing the parotid gland. SCM, sternocleidomastoid muscle.
With this prominent position in the head and neck, the parotid gland has an intimate relationship with numerous critical structures in the head and neck. Similarly, important arterial, venous, and neural structures traverse these glands.
Arterial Anatomy
The external carotid artery divides from the carotid bifurcation and travels below the posterior belly of the digastric muscle (Fig. 1–3, p. 4). Here the facial artery branches off and travels deep to the posterior belly of the digastric muscle to enter the submandibular triangle. The external carotid artery then courses medial to the parotid gland to divide into the maxillary artery and the superficial temporal artery. The maxillary artery exits the medial surface of the gland and divides to supply the infratemporal fossa and the pterygopalatine fossa. The superficial temporal artery gives off the transverse facial artery and exits from the superior pole of the gland. The superficial temporal artery then runs superior in the superior pretragal region toward the scalp.
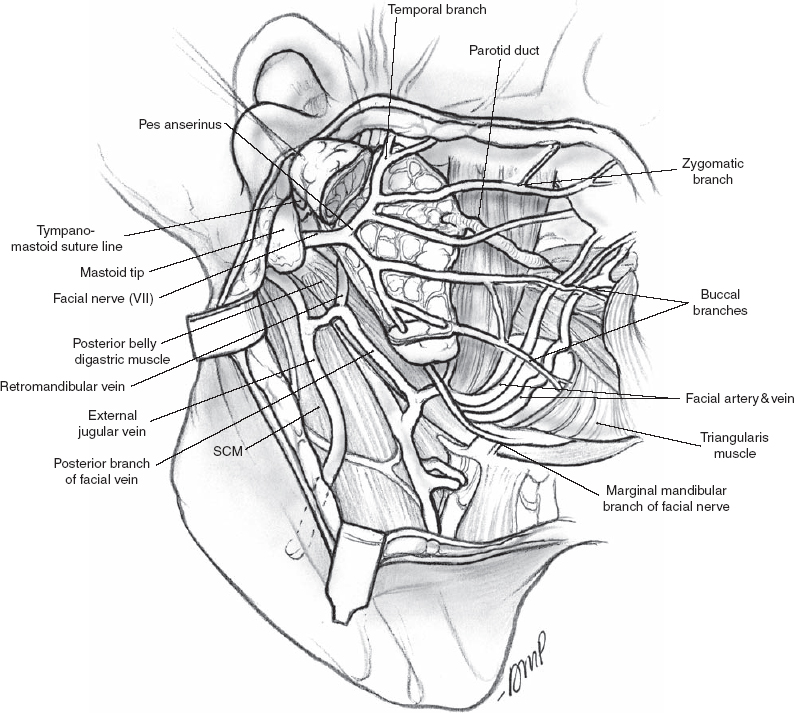
Figure 1-2 Superficial lobe is removed. SCM, sternocleidomastoid muscle
Of note, a prominent branch of the posterior auricular artery is located within 2 mm of the main trunk of the facial nerve. This branch can be an inadvertent source of bleeding during dissection, leading to difficulty when identifying the main trunk of the facial nerve. Similarly, care should be taken not to confuse this structure with the facial nerve propre.
Venous Anatomy
The venous system within the parotid gland parallels the arteries. The maxillary and superficial temporal veins join to form the retromandibular vein, which exits the gland inferiorly and then joins the external jugular vein. The retromandibular vein may also give off a posterior facial vein that joins the anterior facial vein, forming the common facial vein, draining into the internal jugular vein. This will often be the prominent draining pattern in situations where the external jugular system is small or nonexistent. The posterior facial vein is a reliable landmark for identifying the marginal mandibular branch of the facial nerve, as this vein lies immediately deep to the marginal mandibular branch. A mass that imaging studies demonstrate to be superficial to the retromandibular vein will usually be superficial to the nerve. Yet reports do exist of the nerve running deep to the vein.2,3
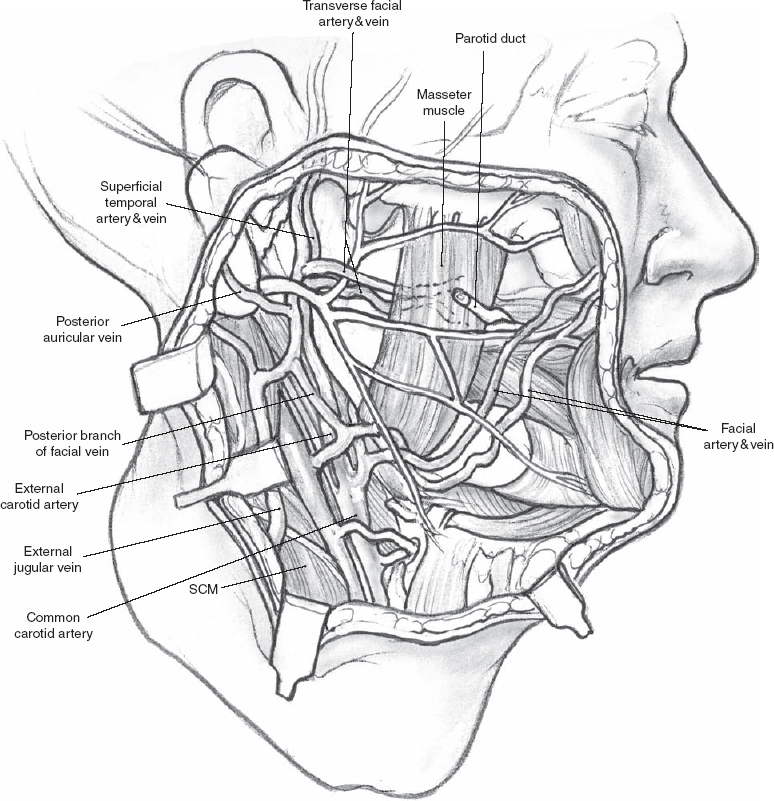
FIGURE 1-3 Arterial and venous anatomy. SCM, sternocleidomastoid muscle.
Stensen’s Duct
The parotid duct, or Stensen’s duct, forms from ductules that arise from the superficial lobe, deep lobe, or both. They join near the anterior border of the gland and traverse forward over the lateral surface of the masseter approximately a finger breadth below the zygomatic arch. The duct can be found along this imaginary line between the oral commissure and the attachment of the ear lobule, measuring 4 to 7 cm. The duct courses anteriorly and then makes a sharp turn and pierces the buccinator muscle and buccal fat pad. The duct opens into the oral cavity at the parotid papilla at the level of the upper second molar. A small accessory parotid gland can be found in 21 to 56% of patients.4,5 It can be found along the parotid duct between the buccal and zygomatic branches of the facial nerve and can be a source of parotid tumors. Accessory glands are distinct from the main body of the parotid but drain into Stensen’s duct via one or more small tributaries.
Neural Anatomy
Great Auricular Nerve
The great auricular nerve is a sensory nerve that arises from the cervical plexus, specifically rootlets of C2 and C3. The nerve is located approximately 1 cm cephalad to the external jugular vein along the lateral surface of the sternocleidomastoid muscle in a subplatysmal plane. As the nerve approaches and enters the tail of the parotid gland, it divides into anterior and posterior branches. The anterior branch supplies the facial skin overlying the parotid gland. The posterior branch supplies the ear lobule. The great auricular nerve is commonly sacrificed during parotid surgery, with resultant long-term postoperative numbness of the ear lobule. Efforts to save the posterior branch of the great auricular nerve during parotidectomy are favored by some surgeons with varying degrees of success. Up to 50% of patients who have preservation of the posterior branch of the facial nerve will have reduced hyposthesia.6 In such dissections, the nerve must be dissected through the lateral surface of the gland. Specific care must be taken during the elevation of the lobule not to sever the distal branches of the nerve as they enter the lobule.
Facial Nerve
Thorough familiarity with the anatomy of the facial nerve is critical to any successful surgical procedure involving the parotid gland. The facial nerve has five segments before exiting the temporal bone: intracranial (pontine) segment, internal auditory canal (meatal) segment, labyrinthine segment, tympanic segment, and mastoid segment (Fig. 1–4). The pontine segment measures 23 to 24 mm long and extends from the pons up to the internal auditory canal. The meatal segment measures 7 to 8 mm and is contained within the internal auditory canal. The labyrinthine segment measures 3 to 4 mm long and extends from the fundus of the internal auditory canal to the geniculate ganglion. The tympanic segment (or horizontal segment) measures 12 to 13 mm long and extends from the geniculate ganglion to the pyramidal turn. The mastoid segment (or vertical segment) measures 15 to 20 mm long and extends from the pyramidal turn to the stylomastoid foramen.
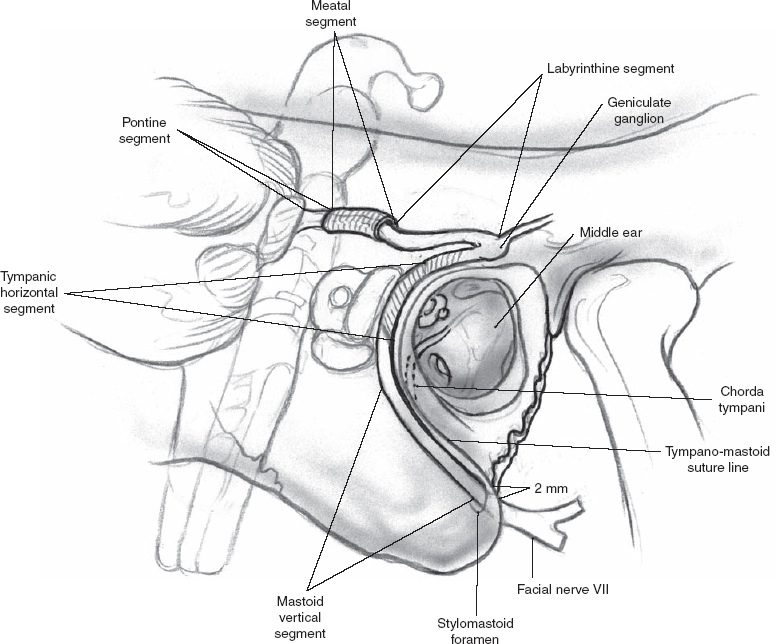
Figure 1-4 Facial nerve from brainstem to stylomastoid foramen.
The extratemporal segment of the facial nerve exits the skull base at the stylomastoid foramen. It is located slightly posterolateral to the styloid process and anteromedial to the mastoid process and digastric groove. In rare occasions, the nerve may follow an aberrant course and exit from the anterior surface of the mastoid process. Before the main trunk of the facial nerve enters the parotid gland, it usually gives off branches to the posterior belly of the digastric muscle, the stylohyoid muscle, and the auricular muscles. The facial nerve divides within the parotid gland, and as it courses through the gland, it becomes more superficial. As the facial nerve enters the parotid gland, it forms the pes anserinus (the characteristic multiple branching pattern that resembles a goose foot), which gives off the two main divisions of the facial nerve. The upper division (temporofacial) branches into the temporal, zygomatic, and buccal branches. The lower division (cervicofacial) gives off the marginal mandibular and cervical branches. Buccal branches may arise from the upper division or the lower division.
There have been many variations of facial nerve branching patterns described. Davis et al7 described six types of branching patterns. The type I pattern, seen in 13% of cases, has no anastomosis between the five branches. The other five types have varying patterns of anastomosis between the five branches. Miehlke et al8 described eight branching patterns where no anastomoses between the branches were seen in 48% of patients. This group also found that the buccal branches can arise from either the temporofacial division (21%) or the cervicofacial division (35%). The temporal branches innervate the anterior auricular muscle, superior auricular muscle, frontalis muscle, and orbicularis oculi muscle. The zygomatic branches innervate the orbicularis oculi muscle, nasal aperture muscles, and elevators of the upper lip. The buccal branches innervate the muscles of the upper and lower lip. The marginal mandibular branch innervates the muscles of the lower lip. The cervical branch innervates the platysma muscle (Table 1-1).
Table 1-1 Facial Nerve Branches and the Muscles They Innervate
| Facial nerve branch | Facial muscle |
| Temporal branch | Frontalis muscle |
| Temporal branch | Anterior and superior auricular muscle |
| Posterior auricular branch | Posterior auricular muscle |
| Temporal and zygomatic branch | Orbicularis oculi muscle |
| Buccal branch | Levators of lip/mouth (zygomaticus major and minor, levator anguli oris, levator labii superioris) |
| Buccal branch | Orbicularis oris muscle |
| Buccal branch | Buccinator muscle |
| Mandibular branch | Depressors of lip/mouth (depressor angularis oris, depressor labii inferioris) |
| Cervical branch | Platysma muscle |
Locating the main trunk of the facial nerve can be facilitated by the following landmarks (Fig. 1–5): (1) The tympanomastoid (TM) suture line is the most constant landmark for finding the main trunk. The facial nerve is usually located ~2 to 4 mm deep to the inferior end of the tympanomastoid suture line. (2) The posterior belly of the digastric muscle is a good landmark for the approximate depth of the main trunk. (3) The tragal pointer is the medial end of the tragal cartilage in the tympanomastoid notch. The facial nerve is located ~1 cm deep and slightly anteroinferior to the tragal pointer. (4) The styloid process can be identified during dissection, and the nerve will be in the soft tissue inferior and superficial to this structure.
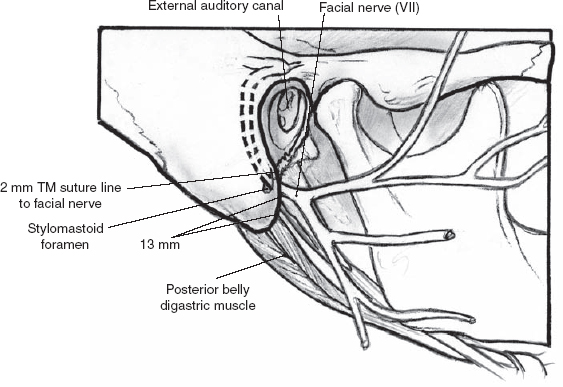
Figure 1-5 Surgical landmarks to identify cranial nerve (CN) VII. TM, tympanomastoid.
The two most important competing landmarks, the tympanomastoid suture and posterior belly of the digastric muscle, have been compared.9 The mean closest distances from the tympanomastoid suture and posterior belly of the digastric muscle to the facial nerve are 1.8 mm (range 0–4 mm) and 12.4 mm (range 7–17 mm), respectively (p < .05), for cadavers. The mean closest distances in live patients from the tympanomastoid suture and posterior belly of the digastric muscle to the facial nerve are 2.0 mm (range 0–4mm) and 10.7 mm (range 5–14 mm), respectively (p < .05). The tympanomastoid suture is a significantly closer and less variable anatomical landmark compared with the posterior belly of the digastric muscle both in cadaver dissection and in live patients (Fig. 1–6).
Should the main trunk not be identifiable at the stylomastoid foramen, alternative means of identification can be undertaken. One approach is to locate the distal branches and trace them centrally toward the main trunk. The marginal mandibular nerve can be identified as it passes over the submandibular gland fascia and dissected retrograde. The marginal mandibular nerve will usually pass superficial to the posterior facial vein. Similarly, the buccal branch can be identified anteriorly at the middle portion of the gland. This branch will lie in close approximation to Stensen’s duct as it courses toward the mouth. The zygomatic branches can likewise be identified as they cross the zygomatic arch. Should this approach fail or if transtemporal identification is preferable, as is seen during reoperation with extensive scarring, a mastoid approach can be used. This is achieved by detaching the sternocleidomastoid muscle from the mastoid tip, which can be opened with a drill to expose the main trunk of the facial nerve. Simple mastoidectomy can also assist with this approach.

Figure 1-6 Cadaver dissection. Single arrow: facial nerve; arrowhead: tympanomastoid suture; double arrow: posterior belly of digastric muscle.
The Autonomic Nerve Supply
The glossopharyngeal nerve (ninth cranial nerve, CN IX) supplies the secretomotor fibers to the parotid gland (Fig. 1–7). The parasympathetic preganglionic fibers arise from the inferior salivatory nucleus and travel via CN IX through the jugular foramen. The tympanic branch (Jacobson’s nerve) turns back into the skull via the inferior tympanic canaliculus and enters the middle ear inferiorly over the promontory proceeding anterosuperiorly. It then courses along the roof of the middle ear to the petrous ridge in the subdural space of the middle cranial fossa as the lesser petrosal nerve. The lesser petrosal nerve then exits the skull through the foramen ovale, and the fibers synapse within the otic ganglion. The otic ganglion is found on the undersurface of the mandibular division (V3)of the trigeminal nerve. The postganglionic parasympathetic fibers exit the ganglion and join the auriculotemporal branch of the mandibular division of the trigeminal nerve in the infratemporal fossa. The auriculotemporal nerve travels parallel to the superficial temporal vein and artery, supplying parasympathetic innervation to the parotid gland for salivary production.
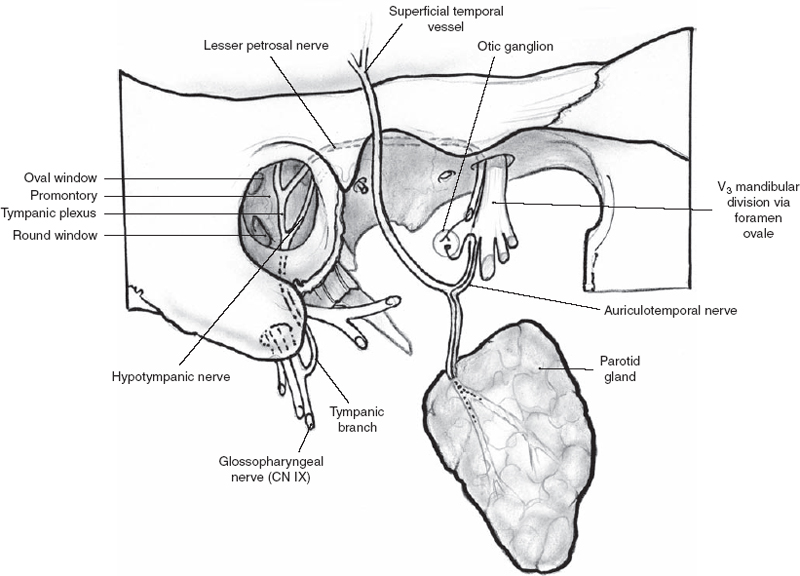
Figure 1-7 Autonomic nerve supply to the parotid gland.
The sympathetic supply reaches the gland from the superior cervical ganglion via the external carotid plexus. Injury to the cervical sympathetic chain leads to anhydrosis as part of Horner’s syndrome. Loss of sympathetic input to the parotid is the explanation for first bite syndrome in patients who have had carotid body tumors (paragangliomas) resected. Cramping in the parotid area is described with the first bite of food of the day or with strong sialagogues such as tart food. With gustatory stimulation, parasympathetic neurotransmitters are released, and concomitant cross-stimulation of sympathetic receptors causes a supramaximal response or denervation supersensitivity of myoepithelial cells.10
Lymph Nodes
The parotid gland is seeded with lymph nodes, unlike other salivary glands. These lymph nodes are within and around the parotid parenchymal tissue. About 90% are located in the superficial lobe.
Parapharyngeal Space
Deep lobe parotid tumors can extend into the para-pharyngeal space. The parapharyngeal space is described as an inverted pyramid with its base at the petrous bone of the skull base and apex at the hyoid bone. The medial boundary is the lateral pharyngeal wall, consisting of the buccopharyngeal fascia, tensor veli palatini, and superior constrictor muscles of the pharynx and nasopharynx. The lateral boundary is the medial pterygoid muscles and its fascia and the ramus of the mandible. The posterior boundary is the carotid sheath, prevertebral fascia, and paravertebral muscles. The anterior boundary extends along the medial pterygoid muscle and the pterygomandibular raphe. The parapharyngeal space lies posterior to the infratemporal fossa.
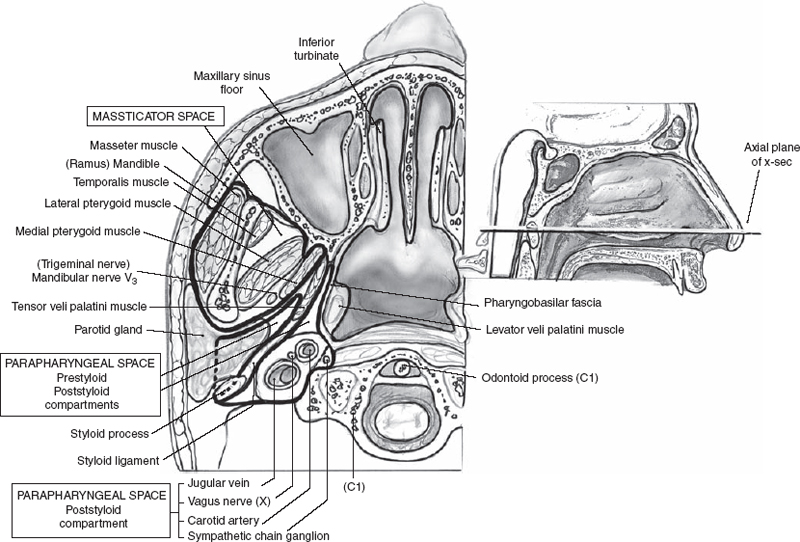
Figure 1-8 Deep parotid anatomy.
The parapharyngeal space is divided into a prestyloid and poststyloid compartment by the fascia of the tensor veli palatini muscle (Fig. 1–8). The prestyloid compart ment normally contains only lymphatics, adipose tissue, and small blood vessels. The poststyloid compartment contains the carotid sheath, with the internal jugular vein, carotid artery, and vagus nerve. This compartment is also traversed by the cervical sympathetics, the glossopharyngeal nerve, and the hypoglossal nerve. On computed tomography (CT) imaging, one can see this fascia extending obliquely from the pterygoid plates anteromedially to the styloid process posterolaterally. Masses that are located anterior and lateral to the fascia are in the prestyloid compartment. Conversely, masses that are posterior and medial to the fascia are in the poststyloid compartment. Deep lobe tumors of the parotid gland are the most common masses of the prestyloid compartment of the parapharyngeal space. Neurogenic tumors such as paragangliomas are the most common tumors of the poststyloid compartment. Schwannomas of the cervical sympathetics and of cranial nerves IX, X, XI, and XII also may be present here.
Parotid gland masses can extend medially into the parapharyngeal space in two ways: (1) the mass can pass posteroinferior to the stylomandibular ligament, or (2) the tumor can pass through the stylomandibular tunnel into the parapharyngeal space, forming a dumbbell-shaped mass. Patients typically present with a mass either in the neck or in the lateral pharyngeal wall (Fig. 1–9). Examination of the oropharynx can reveal medial displacement of the soft palate, tonsil, and lateral pharyngeal wall. The surgical approaches to salivary gland masses within the parapharyngeal space are discussed in detail in a later chapter.
 Submandibular Gland
Submandibular Gland
The submandibular gland, weighing 7 to 16 g, is located in a triangle of the neck bordered superiorly by the inferior edge of the mandible and inferiorly by the anterior and posterior bellies of the digastric muscle. Referred to as the submandibular triangle, this area likewise corresponds to level 1 in the neck staging system. Accordingly, the submandibular gland has an Internal jugular vein intimate relationship with the mandible, hyoglossal muscle, mylohyoid muscle, posterior belly of the digastric muscle, facial artery and vein, lingual nerve, and hypoglossal nerve.
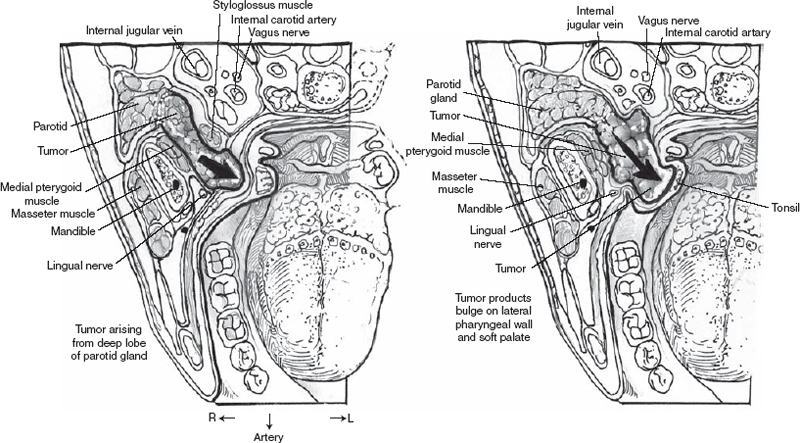
Figure 1-9 Tumor produces bulge on lateral pharyngeal wall.
The submandibular gland is a horseshoe-shaped structure wrapped around the mylohyoid muscle (Fig. 1–10). The smaller sublingual portion is located anteriorly, while resting superior and deep to the mylohyoid muscle. The majority of the gland is located inferior to the mylohyoid muscle in the submandibular triangle. In older patients the gland may lie more inferior in the neck, below the digastric muscles, and is described as ptotic.
Fascial Anatomy
The submandibular gland is surrounded by the middle layer of the deep cervical fascia. This layer is distinct from the superficial layer of the deep cervical fascia that surrounds the platysma muscle. The submandibular fascia is clinically relevant during surgery of this region because the marginal mandibular branch of the facial nerve lies superficial to this fascia and facial vein. Similarly, this facial nerve branch is deep to the fascia surrounding the platysma muscles. Any surgical procedure to this region, whether it is direct removal of the submandibular gland, neck dissection encompassing this region, or external approaches to mandibular fractures, must include a directed effort to preserve the integrity of the marginal mandibular nerve. The surgeon can approximate the location of the nerve as lying superior to a line two finger breadths below the angle of the mandible. In appropriate cases, the surgeon can protect the nerve without direct identification by dividing the anterior facial vein at the inferior surface of the gland and elevating the vein with the fascia. As the nerve runs superficial to the vein, it will be protected during dissection inferior to this plane. However, in clinical settings in which malignancy is suspected, one should strongly consider directly identifying and preserving the marginal mandibular nerve, allowing the fascia to be resected in an en bloc fashion with the gland.
Arterial Anatomy
The facial artery branches from the external carotid system just superior or in combination with the lingual artery. The facial artery courses deep to the posterior belly of the digastric muscle entering the submandibular triangle. It continues superiorly, usually indenting the posterior portion of the submandibular gland. The artery is intimately involved with the gland in this region, giving off small branches to supply the gland. Exiting the superior aspect of the gland, the artery then loops around the inferior border of the mandible, leaving a small indentation in the bone, known as the facial notch. Here, the artery is in close approximation to the lower branches of the facial nerve as it courses superiorly into the face. Although the artery is standardly ligated in two positions, at the inferior border of the mandible and superior to the posterior belly of the digastric muscle during submandibular gland surgery, its integrity can be preserved in certain clinical settings.
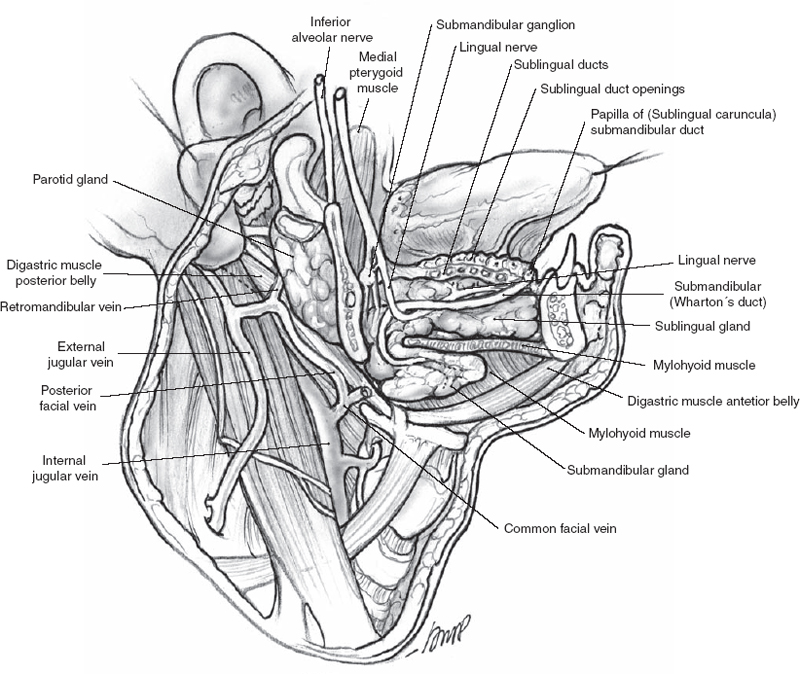
Figure 1-10 Submandibular gland and related anatomy.
Venous Anatomy
The anterior facial vein is adjacent to the facial artery as it descends from the face over the inferior border of the mandible. The anterior facial vein then coalesces with the posterior facial vein and descends over the midportion of the gland forming the common facial vein. Inferiorly, this vein lies lateral to the gland as it exits the lower aspect of the submandibular triangle to ultimately join the internal jugular vein. Although numerous variations exist for the course of the common facial vein, the importance of this structure to the surgeon has already been discussed.
Wharton’s Duct
The ductules comprising the drainage pathway of this secretory gland coalesce into the submandibular duct, which emerges from the sublingual portion of the gland. The duct then courses anteriorly between the hyoglossus and mylohyoid muscles to form Wharton’s duct as it enters the floor of the mouth. Along its course, the submandibular duct runs deep to the lingual nerve and medial to the sublingual gland. It then opens as a papilla in the floor of the mouth adjacent to the frenulum of the tongue.
Neural Anatomy
The facial nerve (CN VII) provides the secretomotor innervation for the submandibular and sublingual glands (Fig. 1–11). The fibers originate in the superior salivatory nucleus in the brainstem and exit via the nervus intermedius before joining CN VII in the internal auditory canal. The fibers then leave CN VII via the chorda tympani nerve in the mastoid segment of CN VII. The chorda tympani nerve courses through the middle ear and enters the petrotympanic fissure to the infratemporal fossa. It then joins the lingual nerve, a branch of the mandibular division of the trigeminal nerve. The fibers then synapse in the submandibular ganglion, and the postganglionic fibers innervate the submandibular gland. Other fibers return to the lingual nerve to innervate the sublingual glands.
Lingual Nerve
The lingual nerve, which provides somatosensory and taste function to the anterior two thirds of the tongue arises from the third division of the fifth cranial nerve, V3 (Fig. 1–12). After exiting the foramen ovale, V3 courses laterally toward the inner surface of the ramus of the mandible. The nerve then branches into the mandibular nerve, which enters the mandible, and the lingual nerve, which travels anteriorly and inferiorly along the lateral surface of the floor of the mouth. A small motor branch to the mylohyoid muscle will separate from the posterior aspect of the nerve under the mandible. This nerve becomes visible when the gland is mobilized inferiorly during removal. Sacrifice of this motor branch is necessary in the majority of cases. The lingual nerve is attached to the deep surface of the submandibular gland at the submandibular ganglion. The nerve carries preganglionic parasympathetic fibers into the submandibular ganglion from which emerge postganglionic parasympathetic fibers to the gland. Traveling anterior to the ganglion, the nerve lies adjacent and superior to the submandibular duct. The lingual nerve and submandibular duct are exposed during dissection when the posterior edge of the mylohyoid muscle is retracted anteromedially.
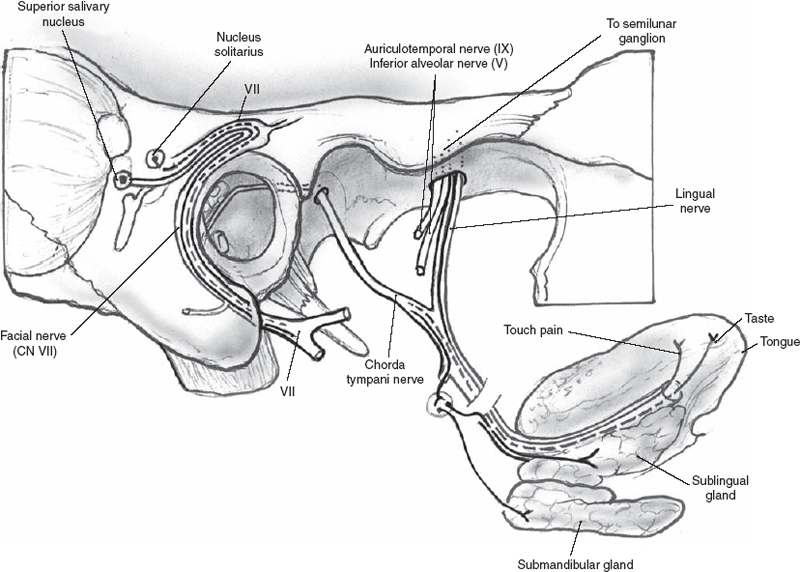
Figure 1-11 Autonomic nerve supply to the submandibular gland.
The Hypoglossal Nerve
The hypoglossal nerve, which provides motor function to the tongue, enters the submandibular triangle just posterior and deep to the junction of the anterior and posterior bellies of the digastric muscle at the lesser cornu of the hyoid bone (Fig. 1–12). The nerve runs in a plane deep to the submandibular gland and its associated structures and is paralleled in its course by a prominent venae comitantes system. The hypoglossal nerve will travel anteroinferiorly to the lingual nerve and is deep to the lingual nerve and submandibular duct. Care is taken to identify the hypoglossal nerve during dissection on the deep surface of the submandibular gland to preserve the integrity of this important motor nerve. The hypoglossal nerve can be readily identified in the submandibular triangle with gentle dissection just posterior to the junction of the anterior belly of the digastric muscle with the inferior attachment of the mylohyoid muscle.
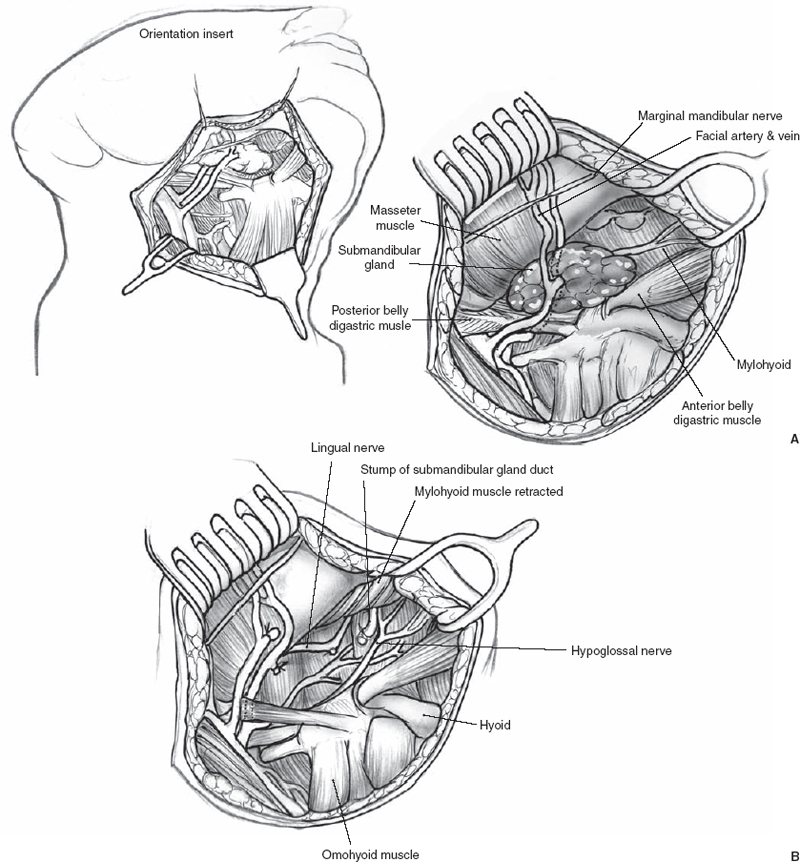
FIGURE 1-12 (A) The submandibular gland is removed, the marginal mandibular nerve is retracted superiorly, and (B) the hypoglossal and lingual nerves are visualized.
Lymph Nodes
The lymph nodes associated with the gland are found superficial to the fascia. They can be located superior to the gland and are associated with the facial artery and vein. These nodes are called prevascular and postvascular nodes. They are important for oral cavity cancers, particularly those of the floor of the mouth. Unlike the parotid gland, the submandibular gland does not contain lymph nodes or lymphoid follicles.
 Sublingual Gland
Sublingual Gland
The sublingual gland is the smallest of the major salivary glands, weighing 2 to 4 g. It is a flat structure lying in the floor of the mouth superior to the mylohyoid muscle (Fig. 1–13). The sublingual glands are paired glands lying opposite the lingual frenulum. The sublingual gland is covered only by oral mucosa. The gland does not have a single duct but rather several ductules that open into the floor of the mouth (Rivinus ducts) or submandibular duct (Bartholin’s duct). The sublingual glands are innervated by secretomotor fibers of CN VII from the superior salivatory nucleus in the brainstem.
Cysts or mucoceles of the sublingual gland, so-called ranulas, can form in the floor of the mouth and extend or “plunge” into the neck inferior to the mylohyoid muscle. Ranulas will be discussed in greater detail in another chapter.
 Minor Salivary Glands
Minor Salivary Glands
Minor salivary glands are found in the lips, tongue, buccal mucosa, palate, retromolar trigone, pharynx supraglottis, and paranasal sinuses and number ~600 to 1000. They are 1 to 5 mm in size. Each gland has its own duct emptying into the oral cavity, pharynx, or paranasal sinuses. They are concentrated in the lips, tongue, buccal mucosa, and palate. The lingual nerve supplies the postganglionic parasympathetic fibers to the majority of the minor salivary glands, though the more superior palatal glands receive innervation from the sphenopalatine ganglion. Salivary gland neoplasms can arise at any of these sites.
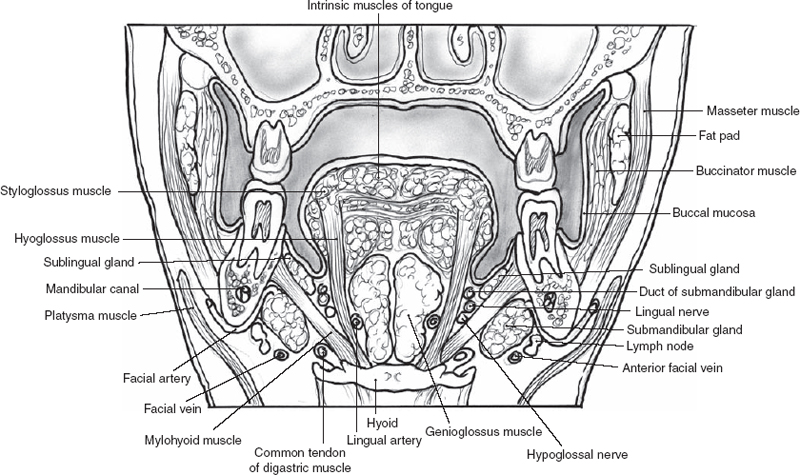
FIGURE 1-13 The floor of the mouth.
REFERENCES
1. Conley, JJ. Surgical anatomy relative to the parotid gland. In: Conley, JJ, ed. Salivary Glands and the Facial Nerve. Stuttgart, Germany: Georg Thieme Verlag; 1975: 7–13
2. Bhattacharyya, N Varvares, MA. Anomalous relationship of the facial nerve and the retromandibular vein: a case report. J Oral Maxillofac Surg 1999; 57 (1): 75–76
3. Kopuz, C Ilgi, S Yavuz, S Oneroglu, S. Morphology of the retromandibular vein in relation to the facial nerve in the parotid gland. Acta Anat (Basel) 1995; 152 (1): 66–68
4. Frommer, J. The human accessory parotid gland: its incidence, nature, and significance. Oral Surg Oral Med Oral Pathol 1977; 43 (5): 671–676
5. Toh, H Kodoma, J Fukuda, J Rittman, B Mackenzie, I. Incidence and histology of human accessory parotid glands. Anat Rec 1993; 236 (3): 586–590
6. Witt, R. Minimally invasive surgery for parotid pleomorphic adenoma. Ear Nose Throat J 2005; 84: 310–311
7. Davis, RA Anson, BJ Budinger, JM Kurth, LR. Surgical anatomy of the facial nerve and parotid gland based upon a study of 350 cervicofacial halves. Surg Gynecol Obstet 1956; 102 (4): 385–412
8. Miehlke, A Stennert, E Chilla, R. New aspects in facial nerve surgery. Clin Plast Surg 1979; 6: 451–470
9. Witt, R Weinstein, G Rejto, L. Tympanomastoid suture and digastric in cadaver and live parotidectomy. Laryngoscope 2005; 115 (4): 574–577
10. Netterville, JL, Reilly, KM Robertson, D Reiber, ME Armstrong, WB Childs, P. Carotid body tumors: a review of 30 patients with 46 tumors. Laryngoscope 1995; 105: 115–126
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


