Chapter 10
Root Resorption
Introduction
Root resorption is the destruction of dental hard tissue, namely cementum and dentine, as a result of clastic cell action (Hammarström and Lindskog, 1985; Andreasen, 1988; Patel and Ford, 2007). It can be broadly classified according to the site of its occurrence on the root of the affected tooth; internal resorption affects the root canal wall, while external resorption occurs on the root’s outer surface. Both types of resorption are subclassified according to the specific histological nature of the resorptive processes occurring, each of which have specific radiographic features.
External root resorption
 External surface resorption
External surface resorption
 External inflammatory resorption
External inflammatory resorption
 External replacement resorption
External replacement resorption
 External cervical resorption
External cervical resorption
Internal root resorption
 Internal inflammatory resorption
Internal inflammatory resorption
 Internal replacement resorption
Internal replacement resorption
A diagnosis of root resorption is reliant on the radiographic demonstration of the process (Andreasen et al, 1987). However, several ex vivo and in vitro studies have demonstrated that conventional periapical radiography is not a reliable technique for detecting external root resorption, especially when the simulated resorptive defects are small (Andreasen et al, 1987; Chapnick, 1989; Goldberg et al, 1998). In contrast, ex vivo studies have confirmed improved accuracy with cone beam computed tomography (CBCT) over conventional periapical radiography in the detection of simulated internal (Kamburoğlu et al, 2011) and external (Bernardes et al, 2012; Ren et al, 2013) root resorption including situations where the external defects are minimal (Durack et al, 2011). Furthermore, some ex vivo studies have also demonstrated that, compared to periapical radiography, CBCT is a significantly more effective method of determining the exact site of simulated resorptive cavities on the external surfaces of roots (D’Addazio et al, 2011; Durack et al, 2011). It also proved the more successful method of differentiating between simulated resorption defects on the root canal wall and on the external surface of the root (D’Addazio et al, 2011; Kamburoğlu et al, 2011). One ex vivo study reported that CBCT could accurately calculate both the volume of resorptive cavities created on the lateral surfaces of roots and the extent of simulated apical root resorption in a linear plane (Ponder et al, 2013).
Clinical studies comparing the diagnostic accuracy of CBCT and conventional radiography in the detection of root resorption are limited. However, one clinical study demonstrated that CBCT is a significantly better imaging modality at determining the presence and extent of external root resorption when compared to conventional radiography (Estrela et al, 2009). In a further clinical study, the performance of periapical radiography and CBCT as diagnostic and treatment planning tools in the management of external cervical and internal root resorption were compared. CBCT could accurately detect the presence and differentiate between the types of resorption (internal and external) in all of the cases examined, and CBCT also performed significantly better than periapical radiography as a treatment planning tool. The overall sensitivity of intraoral radiographs was significantly lower than CBCT (Patel et al, 2009a).


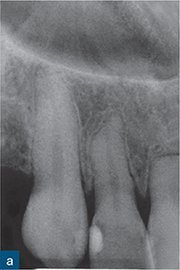
Fig 10-1 External surface resorption. A series of radiographs revealing extensive external surface resorption of the maxillary right first incisor and maxillary left central incisor, and to a lesser extent of the maxillary right second incisor. The patient gave a history of orthodontic treatment and dental trauma.
External root resorption
External surface resorption
Conventional radiography
The conventional radiographic appearance of surface resorption is variable, case-specific, and dependent on the stimulus for resorption. The appearance can vary from small, saucer-shaped, superficial excavations on an otherwise normal root surface outline (as a result of mild traumatic injuries or as a physiological occurrence) to partial or complete destruction of the root (Andreasen and Hjørting-Hansen, 1966a; Andreasen and Pedersen, 1985).
More extensive tissue destruction tends to occur in cases of surface resorption caused by pressure exerted on the roots by orthodontic treatment and/or adjacent impacted masses, such as teeth, cysts, tumours, etc. Teeth with orthodontic-related surface resorption typically present with blunted or uniformly shortened root ends, while the appearance of resorption associated with impacted masses tends to reflect the shape of the offending body (Fig 10-1). Regardless of the aetiology of surface resorption and the extent of the tissue destruction, an intact periodontal ligament (PDL) space/lamina dura typically surrounds the resorbed area of root in cases of surface resorption (Andreasen and Hjørting-Hansen, 1966a).
CBCT
On CBCT scans, external surface resorption has a similar basic radiographic appearance to that seen on conventional radiographs. However, the true nature of the lesion can be more accurately assessed than on conventional (two-dimensional) radiographs. The exact position of any resorptive defect can be pinpointed, and lesions undetectable on conventional radiographs will manifest on CBCT (Fig 10-2). These findings may alter the prognosis of the tooth/teeth under investigation.
External inflammatory resorption
Conventional radiography
External inflammatory resorption associated with dental trauma is characterised radiographically by radiolucent, concave, and sometimes ragged excavations along the root surface, with corresponding and associated radiolucencies in the adjacent alveolar bone (Fig 10-3). There is complete loss of the lamina dura in the area of the resorption (Andreasen and Hjørting-Hansen, 1966b).
External inflammatory resorption is also commonly associated with teeth with infected necrotic root canal systems, and is not always the result of traumatic dental injuries (TDIs) (Laux et al, 2000). In these cases, the resorption site on the affected root will reflect the portal of exit of the bacterial toxins from the root canal. More than one location on the root surface may therefore be affected. However, typically, the apical portion of the root is most commonly affected due to the proximity of the apical foramen (Patel et al, 2016). Conventional radiography may reveal an irregular root at the resorption site. The root may be shortened if the process is occurring apically. The degree of the hard tissue destruction is variable and will reflect the chronicity of the infection. Regardless of the site of the resorption, radiolucency will be present in the adjacent alveolar bone, in addition to the lamina dura, and PDL space will be absent.
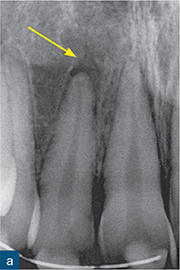

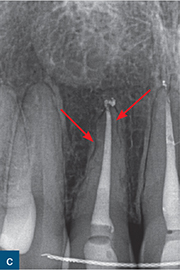
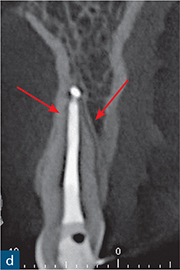
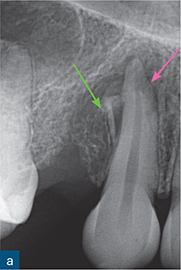
Fig 10-2 External surface resorption. (a) Periapical radiograph of the maxillary right incisor and canine teeth immediately after dental trauma. The maxillary right second incisor had been extruded; the yellow arrow reveals the extent of the extrusion. (b) The sagittal CBCT slice confirms the extent of the extrusion (green arrow). The traumatised non-vital teeth were subsequently endodontically treated and orthodontically repositioned. (c) A 4-year review radiograph reveals signs of external surface resorption (red arrows) on the mesial and distal aspects of the maxillary right incisor. (d) The sagittal CBCT slice confirms surface resorption of the labial and palatal surfaces of the root of the tooth. Note the presence of the intact PDL space and lamina dura around the entire root.

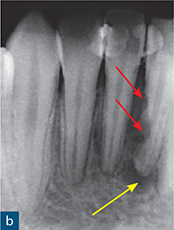
Fig 10-3 External inflammatory resorption. (a and b) Parallax periapical radiographs of the mandibular incisors reveal the classic saucer-shaped excavations on the root surface with associated radiolucencies in the adjacent alveolar bone (red arrows); note there is no intact lamina dura adjacent to the external inflammatory resorption. There is also periapical radiolucency (yellow arrow).
CBCT
On CBCT scans, external inflammatory resorption has a similar radiographic appearance to that seen on conventional radiographs. However, the extent of the lesion can be better appreciated, as can the associated periradicular radiolucencies in the adjacent bone (Figs 10-4 and 10-5). Furthermore, the exact position of any resorptive defect can be localised, and lesions undetectable by conventional radiography (buccal/palatal surfaces) can be seen on CBCT (Durack et al, 2011). These incidental findings, however, do not mean that CBCT should be used as a screening tool to routinely assess external inflammatory resorption.
External replacement resorption
Conventional radiography
The distinguishing radiographic features of ankylosis are replacement of the root with adjacent bone and associated disappearance of the normal PDL space (Fig 10-6). There is no radiolucency in the adjoining bone related to the area of resorption (Andreasen and Hjørting-Hansen, 1966a). External replacement resorption (ERR) can affect any portion of the root and may cause varying levels of tissue destruction..
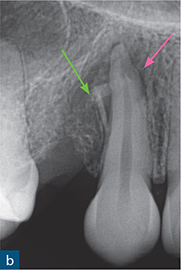

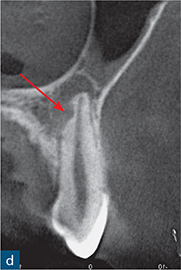
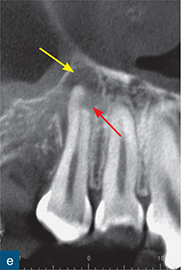
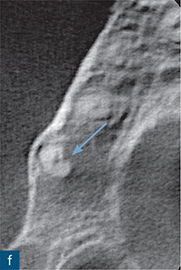
Fig 10-4 External inflammatory resorption. (a and b) Periapical radiograph of maxillary right canine tooth demonstrating a possible periapical radiolucency; note the small bony sequestrum (green arrow) distal to the canine, which was created after extraction of the first premolar, and a subtle radiolucent area (pink arrow) over the apical region of the tooth. (c and d) Sagittal CBCT slices reveal a well-defined periapical radiolucency (yellow arrow) and radiographic signs of external inflammatory resorption (red arrow) of the maxillary right canine tooth. (e) Coronal CBCT slice reflecting the presentation on the radiographs. (f) Axial CBCT slice confirming that the resorptive lesion has not perforated the root canal (blue arrow).
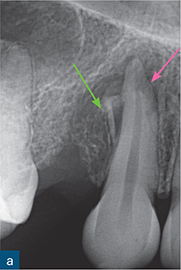
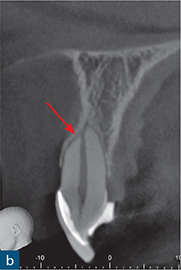

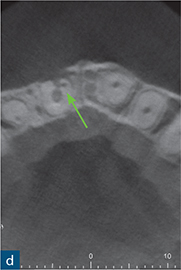
Fig 10-5 External inflammatory resorption. (a) Periapical radiograph of maxillary left central incisor, which has been treated with an intracanal dressing of calcium hydroxide, to a level which is short of the radiographic apex. The apex locator provided a ‘0’ reading at this level and as such the tooth was prepared to this length; note the external surface resorption associated with the mesial root surfaces of the maxillary right central incisor and the maxillary left lateral incisor. This is most likely attributable to a previous TDI suffered by the patient. (b) Sagittal CBCT slice reveals signs of external surface resorption on the mesial aspect of the maxillary left central incisor. (c) Sagittal CBCT slice reveals signs of external inflammatory resorption (yellow arrow) on the mesial aspect of the root of the maxillary left central incisor; note that this may not be seen on the radiograph due to its position on the root surface. (d) Axial CBCT slice reveals signs of external inflammatory resorption on the mesial aspect of the maxillary left central incisor. These CBCT images also confirm that the resorption defect has perforated (green arrow) the root canal system, and will therefore influence the management of this case.
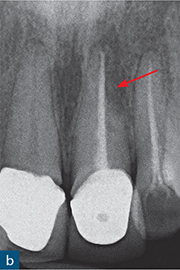
Fig 10-6 External replacement resorption. (a and b) Parallax radiographs of the maxillary left central incisor. Note how bone has directly replaced the root dentine, and how the size of the resorptive defect changes with the second radiograph (red arrow).
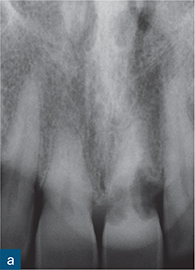

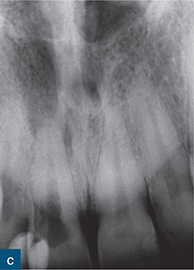
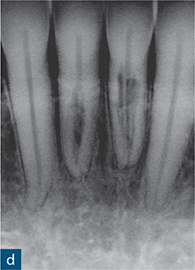
Fig 10-7 External cervical resorption. (a to d) A series of periapical radiographs from different cases demonstrating the variable radiographic presentation of ECR. (a) A ‘moth-eaten’ radiolucency with irregular margins on the mesial and distal surfaces of the maxillary left central incisor. (b) A well-defined symmetrical radiolucency associated with the cervical region of the maxillary left central incisor. (c) An irregular radiolucency with well-defined borders associated with the cervical region of the maxillary right central incisor. (d) A mottled appearance in the roots of both the mandibular right and left central incisors, indicating bone-like metaplastic changes.
CBCT
The radiographic findings are very similar to conventional radiography. However, small, distinct ERR on the labial and/or palatal aspects of the root can only be reliably detected with CBCT. Conventional radiography is better for detecting proximal defects, which have reached a minimum critical size, but is not able to reliably identify smaller lesions on the labial or palatal root surfaces.
External cervical resorption
Conventional radiography
The conventional radiographic appearance of external cervical resorption (ECR) is highly variable and is influenced by a number of factors, including the site of the defect on the affected tooth, to what extent and in which manner the resorptive process has invaded the root dentine, and the relative proportions of granulomatous and osseous tissue occupying the resorptive defect (Gunst et al, 2011, 2013).
ECR typically affects the cervical region of the affected tooth. However, it may not always appear to involve the tooth’s cervical region when assessed on conventional radiographs. ECR may initiate below the cervical region in accordance with the more apical position of the epithelial attachment on the affected tooth. In teeth with a normal periodontal attachment, the lesion may extend some distance apical and/or coronal to the cervical location at which it commenced, reflecting the invasive nature of the process (Heithersay, 1999, 2004).
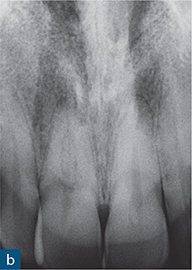

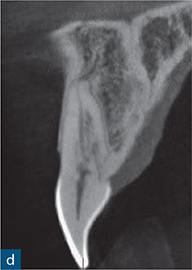
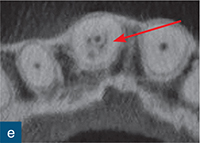
Fig 10-8 External cervical resorption. (a and b) Parallax radiographs of the maxillary right central incisors reveal a ‘fuzzy’ mottled appearance in the coronal and middle third of the root canal. (c) Reconstructed coronal, (d) sagittal, and (e) axial CBCT slices confirm the presence and true extent of the ECR lesion; note how the ECR is encompassing the root canal (red arrow). There is no significant change in position of the resorptive defect relative to the root canal with the parallax radiographs, possibly indicating an internal resorptive defect; CBCT confirms that defect is ECR (courtesy of Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography – an in vivo investigation. Int Endod J 2009a;42:831–838).
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses