The distinctive features of the human face and its visibility to other people pose major challenges in facial reconstruction. When large or massive defects of the face are present, these challenges become truly great. Situations that induce extensive injury with such large losses of facial tissue are infrequent outside of wartime, the most common cause being gunshot wounds—either accidental, self-inflicted, or of criminal origin. Gunshots often produce unpredictable patterns of facial injury with large composite defects that may severely compromise multiple orofacial functions including breathing, eating, speaking, and seeing. Rarely, severe motor vehicle, industrial, or home accidents cause extensive damage, but this is usually of a more blunt nature, with crushing and comminution of facial structures rather than large tissue loss. Glass or metal shards may produce long and deep lacerations with underlying bone fractures, but this is usually a less complicated problem than the tissue loss that occurs with high-energy penetrating missiles and the blast effect from discharge of a gun close to the face.
When presented with a patient who has sustained a severe injury with loss of facial tissues, it can be bewildering to know where to begin after the initial resuscitation, control of bleeding, and systemic stabilization. The successful reconstruction of these facial defects involves replacement of much of the missing tissue before significant scarring and contracture have occurred. Such an approach demands early surgical intervention and the knowledge and application of every known reconstructive procedure and often new, creative designs.
Gunshot Pathophysiology
Although large composite facial defects can occur from numerous causes, they are most consistently produced by firearms. This problem is most significant in the United States, where the continued upward trend in firearm injuries will soon eclipse motor vehicles as the leading cause of traumatic death. As more of these facial insults occur, their management benefits from a basic understanding of ballistics and the mechanisms of tissue injury.
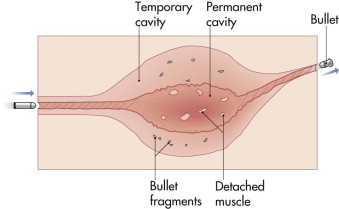
Scientific investigation of the interaction of penetrating projectiles with body tissues has a significant history but is often misunderstood in the medical literature. Although a large number of gun and bullet types exist, the mechanisms by which the projectile disrupts tissue are quite basic and are purely mechanical in nature. Initially, the bullet crushes sufficient tissue to make a hole (entrance), through which it penetrates the underlying tissue (permanent cavity). Depending on the caliber and the speed at which the bullet is traveling, the walls of the permanent cavity radiate outward to form a temporary cavity ( Fig. 20-1 ). The permanent cavity exhibits obvious tissue destruction, but the damaging effect in the temporary cavity is variable. A third mechanism, powder gases that follow the bullet out of the barrel and are forced into the tissues, occurs only in wounds in which the gun is in close contact with the skin at the time of firing.
The tissue damage produced by a projectile depends on numerous factors including its shape, construction, and mass, not just its velocity alone. This is best illustrated by comparing three well-known types of bullets, all of which travel at about the same projectile velocity. From a distance of 15 feet, the tissue damage caused by a .22 caliber bullet is less significant than that caused by a .44 Magnum hollow-point bullet. The increased size and deformation of the .44 Magnum bullet on impact account for the greater tissue damage. Both of these pale, however, when compared with the tissue disruption caused by a load of 00 buckshot from a 12-gauge shotgun. The pellets from a shotgun hit so close together that they shred tissue for a diameter of up to 10 cm, causing the greatest harm of any small firearm ( Fig. 20-2 ).

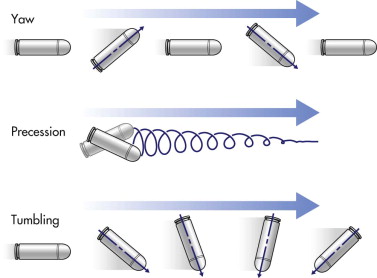
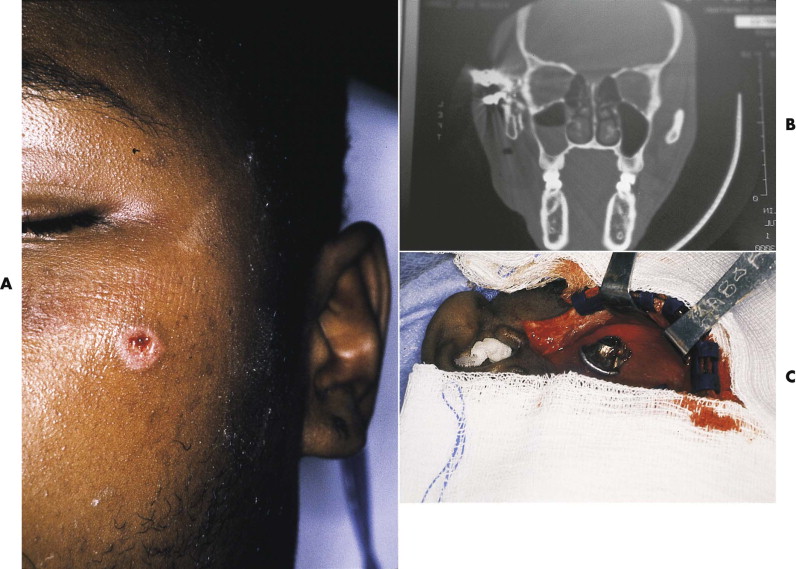
What makes the face unique in most gunshot injuries is that an unimpeded, through-and-through bullet wound occurs in only a minority of cases. The facial bones make up much of the volume of the face, and bone is almost always struck within 1 to 2 cm of the entry point in any facial area. This anatomical difference from the trunk and extremities accounts for two distinct considerations in evaluating and treating gunshot wounds to the face. First, the damage caused by projectiles is a function of tissue density (decreased elasticity). Facial bones, when hit, suffer significant damage, because they have the second highest specific gravity of any body tissue (exceeded only by the enamel of the teeth). Second, when bullets entering the face hit bone, they deform or yaw. Yaw causes them to change direction, altering their original straight path. Yawing of deformed bullets results in an unpredictable path, producing a large temporary cavity and damaging more tissue ( Fig. 20-3 ). Such behavior demands a thorough search for potential injury in all craniofacial areas, not just the structures between the entrance wound and the exit site, if an exit site exists at all ( Fig. 20-4 ).
Wound Classification
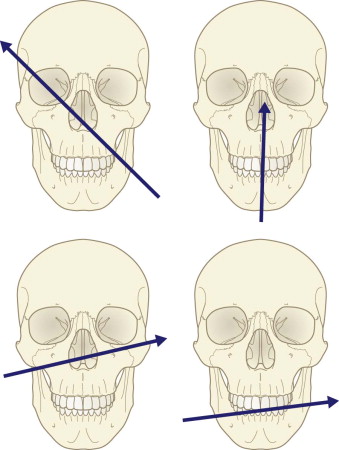
Certain patterns of facial injury caused by penetrating missiles have been reported in the literature. These are based on either the path of the missile (entrance and exit wound) or the pattern of tissue injury or loss that occurs. The four general patterns of involvement for gunshot wounds are the frontal cranium, the orbit, the lower midface, and the mandible ( Fig. 20-5 ). The location of the exit wound provides a rough guide to the pattern, which is most accurately predicted by the locations of the entrance and exit wounds. In general, skin and bone complications are less severe in the upper face and cranial area. In the lower face, there is greater comminution of fractures and damage to the intraoral lining.
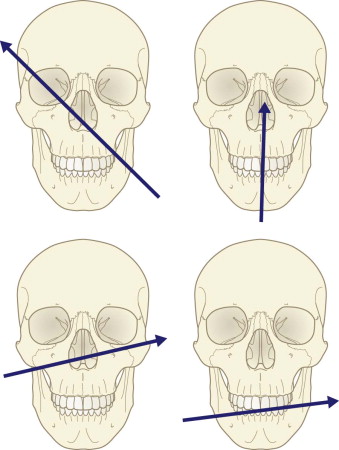
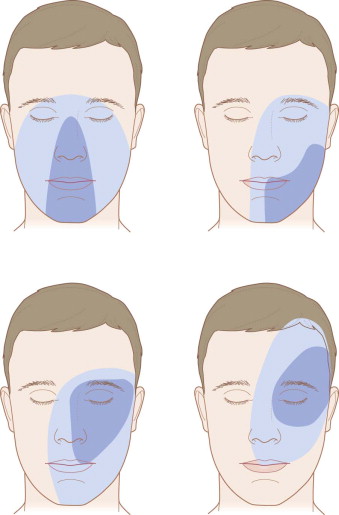
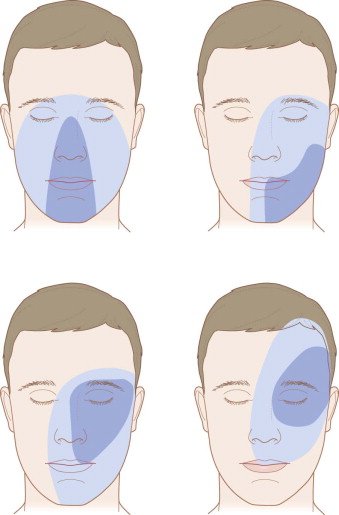
More clinically useful is an appreciation of the zones of facial tissue injury and tissue loss based on the patterns of gunshot wounds. These include the central face, the lateral mandible, the lateral midface and orbit, and the lateral cranium and orbit ( Fig. 20-6 ). In each case, a wide zone of hard and soft tissue injury surrounds a smaller zone of actual hard and soft tissue loss. The important point is to appreciate that the zone of injury is more expansive than that of tissue loss and must be factored into the plan of reconstruction.
Wound Classification
Certain patterns of facial injury caused by penetrating missiles have been reported in the literature. These are based on either the path of the missile (entrance and exit wound) or the pattern of tissue injury or loss that occurs. The four general patterns of involvement for gunshot wounds are the frontal cranium, the orbit, the lower midface, and the mandible ( Fig. 20-5 ). The location of the exit wound provides a rough guide to the pattern, which is most accurately predicted by the locations of the entrance and exit wounds. In general, skin and bone complications are less severe in the upper face and cranial area. In the lower face, there is greater comminution of fractures and damage to the intraoral lining.
More clinically useful is an appreciation of the zones of facial tissue injury and tissue loss based on the patterns of gunshot wounds. These include the central face, the lateral mandible, the lateral midface and orbit, and the lateral cranium and orbit ( Fig. 20-6 ). In each case, a wide zone of hard and soft tissue injury surrounds a smaller zone of actual hard and soft tissue loss. The important point is to appreciate that the zone of injury is more expansive than that of tissue loss and must be factored into the plan of reconstruction.
State-Of-The-Art Management: Basic Principles
The historical approach to early management of ballistic injuries to the face included multiple débridements, daily dressing changes, and delayed reconstruction. This was fostered and appeared rational based on the rate of complications that developed when early reconstruction was undertaken, which included infection, wound breakdown with necrosis, and ultimate collapse of the reconstructed facial segments. The application of craniofacial surgical and diagnostic techniques has revolutionized the management of blunt facial injuries but still frequently fails in cases of gunshot facial wounds if the fundamental differences between these two types of facial injuries are not appreciated. Recognition of the absence of tissue and the devascularized, compromised quality of some of the remaining hard and soft facial tissues is paramount in choosing the appropriate reconstructive techniques and the timing of their application.
The facial gunshot wound, first and foremost, must be controlled by débridement of necrotic, nonviable tissue; elimination or evacuation of hematoma and infection; obliteration of dead space with vascularized tissue; and re-creation of adequate skin and mucosal lining. In addition to understanding this most important conceptual approach, the initial management of facial gunshot wounds should take into account several basic principles derived from the unique anatomy of the face and the behavior of penetrating missiles.
Treat the Wound, Not the Weapon
The exact gun type and circumstances that caused the facial wound, while of interest, do not guide or alter the subsequent surgical management. Victims and observers of gunshot wounds are unreliable and frequently misrepresent many of the events of the shooting, particularly the type of weapon and the distance of fire. Focus on the facial damage present, and do not concern yourself with the details of the gun. The only gun-specific information that really matters is whether it was a single-bullet or a multiple-pellet firearm. However, the facial wound itself usually makes this obvious. Much is made of whether the penetrating missile is of high or low velocity, but this does not usually change the required treatment.
Provide Primary Care after Basic Trauma Resuscitation
In patients with significant injuries and severe facial tissue damage, management of the airway is of supreme importance. Intubation, or preferably tracheostomy, should be liberally done. In addition to solving issues of early airway patency and obstructive bleeding, this facilitates the numerous subsequent reconstructive procedures. Oral or nasal intubation often hinders proper access for the reconstruction, even many months later. It is not uncommon to keep a tracheostomy or feeding tube in place for up to 1 year after the injury in cases of severe facial tissue loss. Patients tolerate airway and feeding tubes well, and they do not preclude breathing around the tracheostomy tube or oral feeding between reconstructive surgeries.
Provide Adequate Antibiotic Coverage in the Immediate Injury State
A bullet is not sterilized by being fired. Penetrating projectiles carry bacteria into the wound. When combined with the presence of devitalized tissues and open wounds, a near-ideal bacterial culture medium may exist that can overcome even the superior blood supply of the face. Group A β-hemolytic streptococci and clostridia were historically reported from battlefield gunshot wounds but have been almost eliminated since the development of antibiotics during World War II. A broad-spectrum cephalosporin or penicillinase-resistant antibiotic should be given. Subsequent surgeries are covered as for any other facial reconstructive procedure.
Maintain a High Level of Suspicion for Vascular Injury
By definition, most facial gunshot wounds are classified as being in zone II (between the cricoid cartilage and the mandibular angle) or zone III (between the mandibular angle and the skull base). Vascular injury in these zones may be obscure and not easily diagnosed by clinical examination. Computed tomographic (CT) evaluation is especially helpful for assessment of major vessels and the cranial and orbital contents. When in doubt, consider carotid angiography.
Provide Initial Surgical Treatment with Minimal Débridement and Primary Closure
After stabilization, the patient should be taken to the operating room as soon as possible. This permits a thorough wound exploration and determination of what type of reconstruction will be needed. At this time, the following tasks can be accomplished:
- •
Remove loose teeth and bone.
- •
Remove obvious bullet fragments, but do not dissect and retrieve fragments that lie deep.
- •
Débride only obviously nonviable tissue.
- •
Irrigate copiously with saline.
- •
Close as much of the soft tissue as possible, going from the inside out.
- •
Stabilize facial bones by direct plate and screw and maxillomandibular fixation if enough teeth and jaw structures are present, or use an external mandibular or cranial halo (midface) fixator if large bone segments lack continuity and flail segments are present.
Plan for Early Reconstruction with Tissue Replacement
Early reconstruction with tissue replacement is the cornerstone of contemporary reconstruction of large facial defects. Early replacement of hard and soft tissue deficits provides the best long-term results. Until recently, treatment consisted of initial wound débridement, packing of extensive defects, and serial dressing changes followed by surgical débridement procedures until soft tissue closure could be achieved. Concerns about contamination and lack of reliability of local tissues were overriding themes. It is now clear that there is no facial advantage to allowing the wound to heal by secondary intention or skin grafting of open wounds before reconstruction is initiated. The historical approach allowed a tremendous amount of scar formation and contracture to occur, making the formal reconstruction attempts much more difficult and often leading to partial or patchwork results. Facial tissue should be replaced as soon as the patient is stable and the margins of wound viability are clear. Neurological and ophthalmological injuries frequently cause the initial reconstruction to be delayed, but often it can still be performed within the first weeks after injury. A pre-reconstruction CT scan, preferably three-dimensional, can be very informative as to the extent of missing bone.
The contemporary approach employs liberal use of microvascular tissue transfers to replace missing bone, oral lining, and cutaneous cover, often in a single operation. Although a single free flap alone cannot provide complete facial reconstruction, it does introduce healthy, unscarred tissue that can be manipulated in subsequent procedures.
Reconstructive Flap Options
The concept of early tissue replacement in extensive traumatic facial wounds is very similar to the reconstruction of facial defects after oncologic resection. Knowledge of a variety of tissue flaps, some that must be transferred as free tissue and others pedicled in design, provides powerful reconstructive options that permit early facial intervention. These include flaps composed of free bone with or without a skin paddle and free fasciocutaneous, free muscular, and pedicled fasciocutaneous options. Several superb texts are available on this topic that provide detailed descriptions of the entire scope of tissue flap anatomy, and the reader is referred to these for descriptive detail and operative guidance. The following sections are not meant to be all-inclusive but describe those flaps that are commonly used for facial gunshot wounds.
Free Fibular Flap
The fibula is the longest bone that can be transferred by microsurgical techniques. It is often described as an ideal mandibular replacement in terms of bony stock, but this is not entirely accurate. It has very similar cross-sectional thickness but inadequate vertical height—usually less than half that of a normal dentate mandible. Its available length, up to 24 cm, does allow it to be used for long bone defects. The pedicle is large and very reliable, and septocutaneous branches make formation of a significant skin paddle possible. It is a truly expendable long bone with little donor morbidity other than an external scar if properly harvested.
Fibular transfer depends on the endosteal and periosteal blood supplies from the peroneal artery. The endosteal circulation is supplied through a nutrient artery that typically enters the middle third of the fibula. The pedicle of the peroneal artery is rather short, usually about 6 to 8 cm at best. A single central artery with a diameter of 2 to 3 mm is surrounded by two venae comitantes. In addition to the nutrient and periosteal vessels to the fibula, the peroneal artery gives off multiple branches to all of the surrounding muscles of the leg and to the lateral leg skin. There are two to six cutaneous perforating branches of the peroneal artery which travel along the posterior crural septum and through the soleus and flexor hallucis longus muscles. They supply a longitudinally oriented area of skin that can be raised as a septofasciocutaneous flap with the central axis along the posterior crural septum ( Fig. 20-7A ).
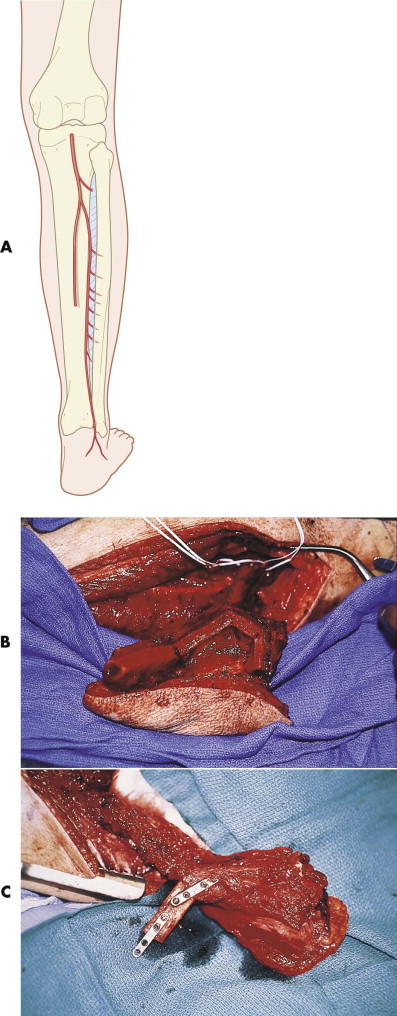
The fibular free flap is most commonly used for mandibular reconstruction, particularly of the symphysis and angle, where osteotomies may be required to provide a three-dimensional reconstruction. When used with a skin paddle, it offers replacement of the external skin, lip, or lining of the buccal mucosa or floor of the mouth (see Fig. 20-7B,C ). If only a small amount of bone is needed, such as in reconstruction of the anterior maxilla, a long vascular pedicle can be created by use of the more distal end of the bone.
Free Scapular Flap
The scapular flap has gained utility because it provides good bone stock with a large pedicle that is long and relatively easy to find. The circumflex scapular pedicle is a branch of the subscapular system, with a pedicle length of 5 to 6 cm and vessel diameters up to 2.5 mm. The direct vascular connection between the circumflex scapular artery and the periosteum of the scapula makes osseous transfer possible. The lateral border of the scapula provides a 10- to 14-cm segment of straight bone located between the glenoid fossa and the tip of the scapula. The lateral inferior axillary border of the scapula also receives a periosteal pedicle (angular) from a branch of the thoracodorsal artery and associated venae comitantes. If the thoracodorsal branch is included with the circumflex scapular pedicle, a second vascularized bone segment may be designed with the scapular flap. The overlying soft tissue can be harvested with the bone transfer, either with or without the overlying skin. The skin is thick and hairless and has only a thin layer of subcutaneous fat, which is usually advantageous in the face. The donor site can be closed primarily, even when a skin paddle is used, and the back scar is often wide but acceptable. One of its most significant advantages is the wide arc of movement between the skin paddle and the osseous portion of the flap, which is related to the differing transverse (skin paddle) and descending (bone) branches of the circumflex scapular pedicle ( Fig. 20-8 ).
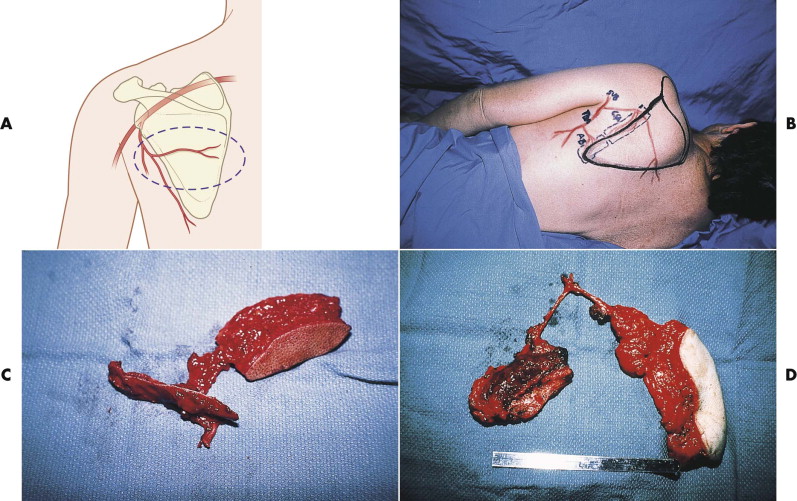
The scapular region also provides an excellent source of vascularized fasciocutaneous tissue, which was used long before its potential for bone transfer was recognized. The soft tissue is based on the horizontal or descending branch of the circumflex scapular artery in either a horizontal (scapular) or vertically oriented (parascapular) design. This provides thin, pliable tissue, up to 10 cm in width with skin attached, or larger if only the fascial component is required.
The one disadvantage to the scapular flap is the necessity for significant arm rotation to properly visualize and dissect the pedicle through the triangular space. This precludes a two-team approach with simultaneous flap elevation and facial recipient site preparation.
Use of the scapular free flap has been described for both mandibular and maxillary bone reconstruction. It is a good choice when a straight piece of bone is required. The use of a skin paddle with bone makes it useful for a variety of composite defects about the orofacial and orbitomaxillary regions. The fascial or fasciocutaneous component alone provides an excellent source of vascularized soft tissue fill.
Free Radial Flap
The radial forearm provides a potentially large, thin fasciocutaneous free flap on the ventral surface. It was historically described as a useful osteocutaneous flap, but the radius is a poor source of good bone stock and places the donor bone at a significant risk of postoperative fracture. If bone is needed, other free flap options (e.g., fibula, scapula) are usually better. The forearm should be used as a source of thin soft tissue only.
Almost all or any part of the skin and fascia extending from the antecubital fossa to the wrist may be elevated based on the radial artery and its septocutaneous branches. The more distal the skin flap is designed, the longer the pedicle will be. The radial artery is of good size (2.5 mm) and has a very consistent anatomy; it courses between the bellies of the brachioradialis and pronator teres in the upper forearm and between the tendons of the brachioradialis and flexor carpi radialis in the lower forearm. Most of the septocutaneous-fasciocutaneous branches are in the distal half of the radial artery and are easily identified emerging from the intermuscular septum, which must be preserved during harvest, at the radial border of the flexor carpi radialis muscle ( Fig. 20-9 ).
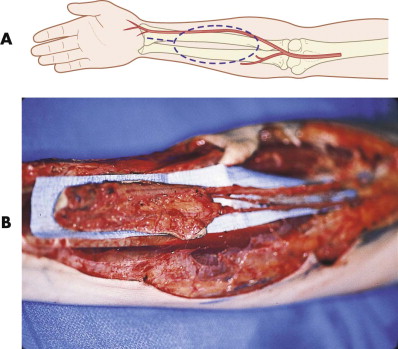
The radial forearm flap has numerous advantages as a soft tissue source, including a large amount of thin tissue, a long and large pedicle, and ease of harvest. These qualities make it particularly well suited for lining intraoral defects or as an external skin cover. However, the harvest of a flap from an extremity requires several precautions to avoid significant donor site complications. It is essential that the inflow to the hand be preoperatively evaluated with an Allen test to confirm that circulation through the ulnar artery is sufficient for survival of the hand. This should be reconfirmed during flap dissection by placement of a microvascular clamp distally and release of the tourniquet before division of the radial artery. The peritenon covering the tendons of the flexor carpi radialis, brachioradialis, and finger flexors must be preserved to avoid skin graft failure and possible loss of the tendons postoperatively.
Free Latissimus Flap
The latissimus dorsi is a large, flat, triangular muscle that offers the largest source of well-vascularized soft tissue in the body, measuring up to 25 × 35 cm in size. Its tendon attaches to the humerus proximally with broad attachments to the lower thoracic and sacral vertebrae, the posterior iliac crest, and the external abdominal muscles. Although it is responsible for adduction, extension, and rotation of the humerus, it is a completely expendable muscle in most patients as long as they have intact synergistic shoulder girdle musculature. Its dominant pedicle is the thoracodorsal artery and venae comitantes, which is a major branch off the subscapular artery. The thoracodorsal pedicle (2.5 mm in vessel size) offers reasonable length, approximately 8 cm, but this can be significantly extended if the distal portion of the muscle is the only tissue required. A reliable, large skin paddle can also be obtained, because there are extensive vascular communications to the overlying back skin. When a skin paddle is taken, the donor site can almost always be primarily closed. Whereas rotation of the muscle into the head and neck area can be done around the axilla with tunneling on top of the pectoralis muscle, it will extend only to the lower face and may potentially be compromised by compression of the overlying tissues. It is of far greater utility when transferred as a free microvascular flap ( Fig. 20-10 ).
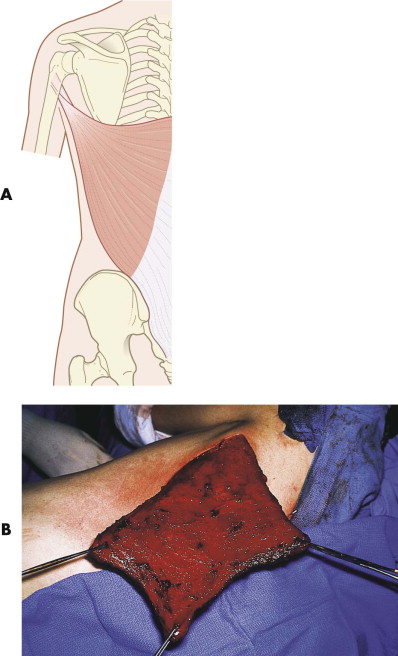
The latissimus dorsi free flap has numerous applications in reconstruction of the face. Over the past 20 years, it has been equally applied to the midface and the mandible with great reliability. Its wide muscular expanse makes it uniquely suited for extensive scalp replacement and calvarial coverage when combined with skin grafting. The reliability of its skin paddle can provide for reconstruction of large defects of the external skin cover, particularly in the lateral face. The patient position necessary for harvest does make it difficult for a simultaneous two-team approach, but the speed at which the flap can be raised makes this of little significance.
Free Rectus Flap
The paired, vertically oriented rectus muscles of the abdomen provide another reliable donor source for vascularized tissue. This long, flat muscle, measuring about 6 cm in width and 25 cm in length, is easy to harvest because of its constant anatomy, and this can be done simultaneously with facial work in a two-team approach. It lies within an anterior and posterior fascial sheath, and its dissection is complicated only by the release of the tenacious attachments of three sets of horizontal inscriptions. Although there are dual dominant pedicles, the inferior epigastric is always used because of its larger size, longer length, and easier dissection. Entering at the underside of the lateral surface of the muscle, the inferior epigastric is about 2.5 mm in diameter with a fairly short pedicle length of 4 to 5 cm. The length of the muscle typically makes the usable pedicle length longer than that of the actual vessels. A vertical or horizontally oriented skin paddle can be taken, but this is rarely done in facial reconstruction. The donor site, even if a skin paddle is taken, can always be primarily closed. Previous abdominal surgery with any horizontal scar across the rectus territory precludes its use.
The musculocutaneous territories supplied by the inferior epigastric have their greatest use in breast reconstruction, but they also have significant value in a variety of head and neck sites. When combined with a skin graft, they can be used for outer coverage of scalp and skull defects and as vascularized fill for a wide variety of lower facial wounds. The long length of the muscle rarely makes its short pedicle length a problem ( Fig. 20-11 ). However, extending the pedicle into the neck for anastomosis requires a very wide subcutaneous tunnel to avoid postoperative venous congestion of the flap.

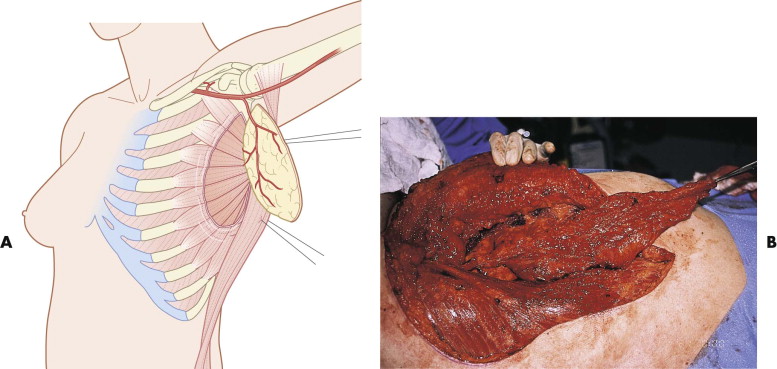
Free Serratus Flap
The free serratus flap provides a very long pedicled musculofascial flap that has excellent utility for facial applications. Its long pedicle (15-20 cm) combined with the length of muscle and fascia can easily reach the midface when anastomosed into the neck. It can be raised with both skin and muscle, but the amount of rib obtained is not sufficient for most facial reconstructive needs. The serratus is a thin, broad muscle that originates from the outer surface of ribs 8 and 9 and inserts on the ventral surface of the scapula. It has a dual blood supply from the lateral thoracic artery and branches of the thoracodorsal artery. Most commonly, the flap is based on the thoracodorsal branch as it emanates from the undersurface of the latissimus dorsi, because it is easier to elevate. The serratus has very predictable anatomy and is easy to identify and dissect out between the lateral borders of the latissimus and the pectoralis, tracing the pedicle up into the axilla ( Fig. 20-12 ).
Pedicled Forehead Flap
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


