Principles of Treatment
In this book we shall present only a brief discussion of the basic principles for the treatment of functional disorders. A more detailed description of therapeutic measures is anticipated in a future work.
An individualized functional therapy demands special knowledge in two distinctly separated areas, that of general therapeutic principles and that of specific clinical application. From a study of the literature and the diagrams in Figures 1–3 it is sufficiently apparent that in biological systems symptoms can arise from a multitude of potential etiological factors. The only effective means of treatment, therefore, is the systematic reduction of these harmful influences. It is completely irrelevant by which therapeutic measures the symptoms are reduced. By this we mean that the methods of alternative medicine have just as much justification as the procedures learned primarily in school, provided that evidence has been brought forth that they can effectively reduce the harmful influences.
In functional therapy a basic distinction should be made between symptomatic treatment and treatment that is directed toward the causative factors. A cause-oriented therapy is possible only if the cause of the symptoms (which may be at a completely different location) is known and can be eliminated by treatment directed specifically toward it. This presupposes a systematic diagnostic procedure with specific identification of the contributing factors. Symptomatic therapy, on the other hand, is applied for a generalized reduction of symptoms, frequently without knowing what the etiological factors are. The concept of symptomatic therapy includes many alternative therapeutic measures (dos Santos 1995, Wright and Schiffman 1995), the prescription of medications, alterations of diet (Ciochon et al. 1997, Hinton and Stinson 1997, Loudon 1997), acupuncture (Rosted 1998, Ernst and White 1999), hypnosis (Dubin 1992, Oakley et al. 1994, Crasilneck 1995), cold and heat application (Sturdivant and Fricton 1991, Feine et al. 1997), and psychotherapy (Rudy et al. 1995, Dworkin 1997), The contribution of dentistry is the reduction of occlusal factors with the help of occlusal splints. Only when occlusal vectors are identified in the same direction as the individual loading vectors can splint therapy be called a cause-oriented therapy. In all other cases, an occlusal splint is only a symptomatic treatment aid. Before irreversible alterations of the occlusion are undertaken, it must always be established with certainty that a causal connection exists between the static or dynamic occlusion and the current loading vector. The role of the physical therapist in the treatment team is to eliminate musculoskeletal impediments (pp. 138 and 304). In this respect a systematic functional therapyultimately comprises three components:
• Diagnosis and relief of overloaded, nonadapted structures (by the dentist).
• Mobilization of unyielding adapted structures (elimination of impediments in the direction of treatment by the physical therapist).
• Permanent reordering of the previous functional pattern (by the patient).
No long-term success can be expected if one or more of these components is missing. The more effectively the structures are unburdened, the more successful the treatment will be. With occlusal splint therapy, for example, there is long-term repositioning of only 36% of displaced disks (Okeson 1988), whereas with the more mechanically efficient Herbst hinge appliance the rate is 87% (Summer and Westesson 1997). Even so, a substantial change in functional patterns (either within the connective tissues or the nerves and muscles) by the patient leads to a significantly better therapeutic result (Turk et al. 1996). Under the unified concept, the interdisciplinary treatment team is composed ideally of a dentist (to remove local contributing factors), a physical therapist (to remove local impediments), an orthopedist (to remove systemic factors from the musculoskeletal system), and a craniosacral therapist (to remove systemic impediments). Additional adjuvant forms of therapy may also be required in individual cases.
Specific or Nonspecific Treatment?
During a tissue-specific examination using manual functional analysis the clinician may discover painful conditions, painless disorders, or even no pathological conditions at all.
With painful conditions there is the question of whether the loading vector is specific (pain can be elicited in only one primary direction) or nonspecific (there is pain from manipulations in multiple directions). If there is a specific loading vector it must be further determined whether or not there is an occlusal vector in the same direction. If this is the case, specific treatment can be provided, first reversibly by means of an occlusal splint and finally by permanently altering the occlusion. If there is a nonspecific loading vector, only nonspecific treatment for relief of pain can be administered (p. 303), at least initially.
The same is true in principle for painless disorders (constriction of the capsule and muscles, changes in muscle strength and tonus). If the changes are present in only one main direction, the problem can be addressed with physical therapy. Otherwise, only a nonspecific approach is possible.
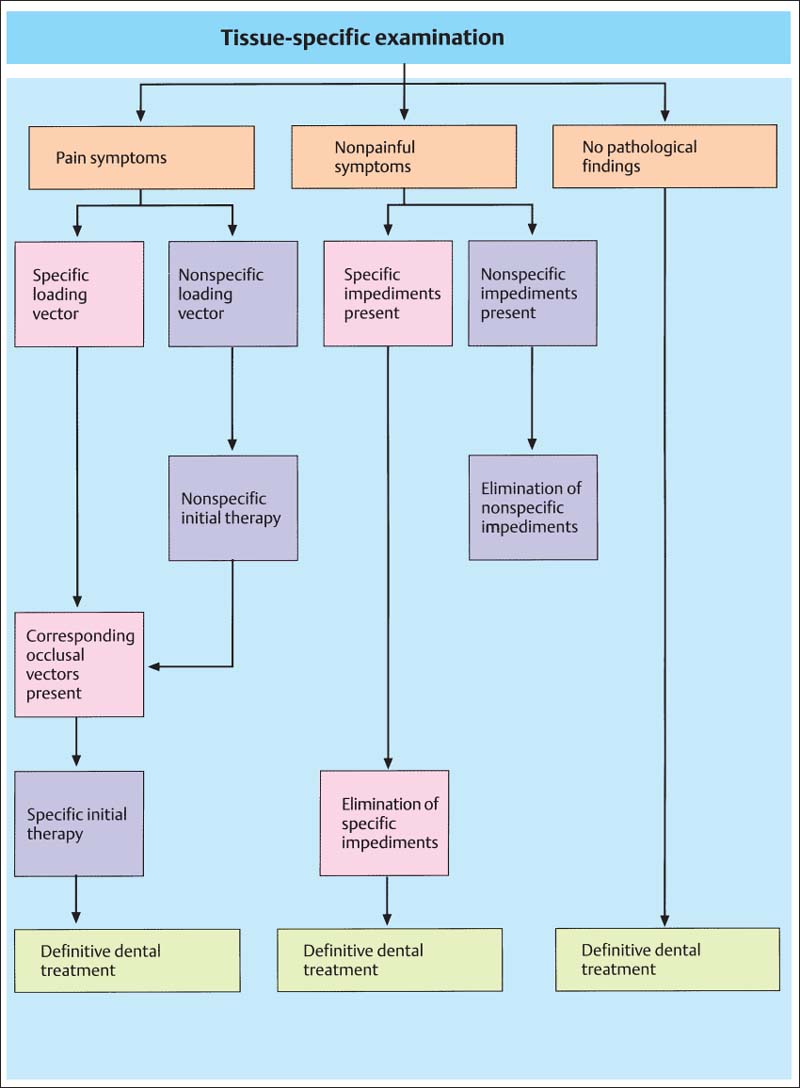
801 Specific versus nonspecific therapy
Schematic representation of the diagnostic parameters that lead to the decision as to whether a specific or a nonspecific therapy will be applied.
Nonspecific Treatment
Nonspecific treatment must always be used when inflammatory tissue changes or nonspecific loading vectors are present. These cases are usually diagnosed with the aid of the jointplay test (passive compressions, translations, and traction). While patients with positive responses limited to passive compressions can often be given specific treatment, there is no alternative to nonspecific treatment for those with positive responses to both passive compressions and translations, as well as to traction. In this phase, the dental team member may make use of a stabilization splint (with posterior cusp indentations and anterior or canine guidnce) and various medications (analgesics, anti-inflammatory drugs, muscle relaxants, sodium hyaluronate, glucocorticoid) (Brazeau et al. 1998). Injections of corticosteroids and hyaluronate can provide pain relief that has been reported as short-term (Kopp et al. 1991, Alstergren et al. 1996, Sandier et al. 1998) and long-term (Wenneberg et al. 1991), but these cause no radiographic changes in the joint. Effects that are frequently observed clinically such as on capsular hypomobility have not yet been systematically investigated.
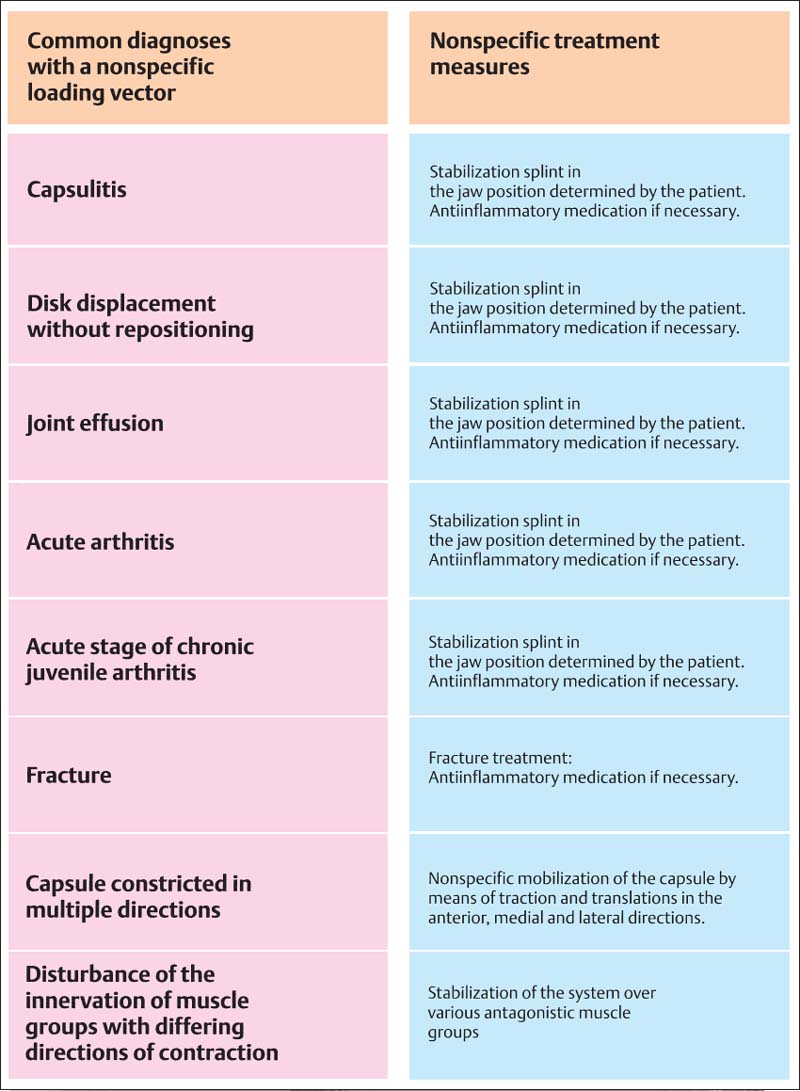
802 joint disorders with nonspecific loading vector and their initial treatment
A listing of the most frequent clinical diagnoses that can be associated with a nonspecific loading vector. Regardless of the current diagnosis, nonspecific treatment is instituted for the purpose of converting the nonspecific loading vector (evidenced by numerous nondirectional positive responses during the joint-play test) into a specific one (positive responses in separate limited directions). Only then can a causal relationship between the functional disturbance and the individual occlusion be tested. The nonspecific pain-relief phase, using a relaxation splint and anti-inflammatory medication usually lasts 3-7 days. If the pain does not significantly decrease during this time, the patient should be referred to a specialist. As soon as the nonspecific treatment for pain has rendered inferior traction and/or anterior translation painless, a physical therapist can be included in further treatment to relieve stresses on the joint.
Elimination of Musculoskeletal Impediments
Within the concept of interdisciplinary treatment, the primary assignment of the physical therapist is to remove musculoskeletal impediments (= restrictions). From the medical viewpoint, there is no urgent need for this unless restrictions exist in the direction of therapy. There are three separate treatment elements: physical therapy, manipulative therapy, and coordination exercises. The components of physical therapy are:
• cold and heat applications
• ultrasound
• laser treatment, and
• transcutaneous electric nerve stimulation [TENS) (Linde et al. 1995, Wright and Schiffman 1995. Conti 1997, Murphy 1997, Pinheiro et al. 1997. Gam et al. 1998, Rosted 1998, Craig et al. 1999. Ernst and White 1999).
Even if long-term success is not realized, physical therapy can help, at least as long as the treatment is continued (Di Fabio 1998). Many methods, however, have proven to have no benefit beyond the placebo effect (Feine and Lund 1997). One exception is treatment with cold (Oosterveld and Rasker 1994), in which ice massages were more effective than cold packs (Zemke et al. 1998).
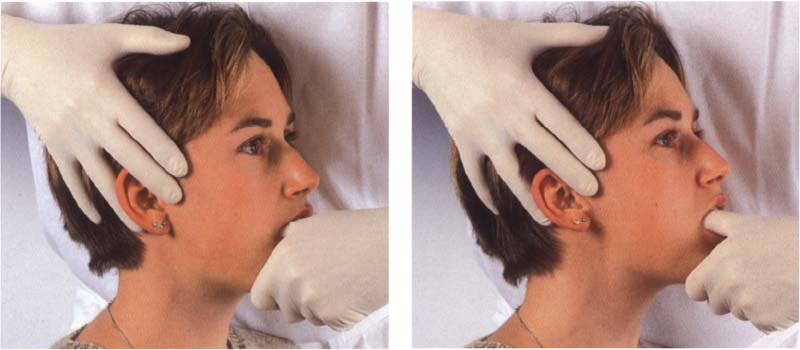
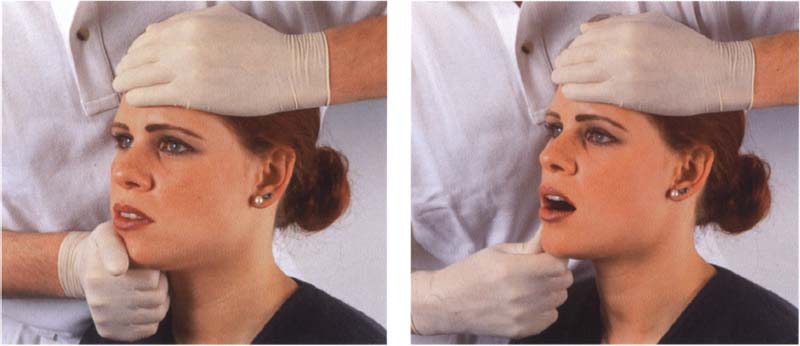
803 Capsule hypomobility
Left: A structural hypomobility (= constriction) of the joint capsule in the vertical direction can be treated through traction. However, this treatment can be used only if no pain could be elicited in this direction during the diagnostic procedures. The number of treatment sessions varies from one to three per week depending upon the individual case. Right:Anterior translation is used to treat capsule hypomobility in the horizontal direction.
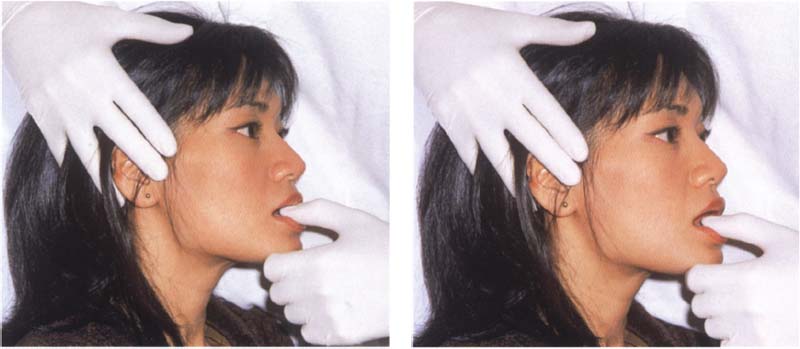
804 Shortening of the muscles
Left: Shortening of the noncontractile elements of a muscle (=muscle shortening) is treated by static and dynamic muscle stretching. This is performed by having the patient open the mouth to the first level of muscle tension and then exerting a light isometric force against the clinician’s thumb. This causes the contractile muscle cells to stretch the noncontractile elements.
Right: After the mouth has been opened in stages without strain, the procedure is repeated.
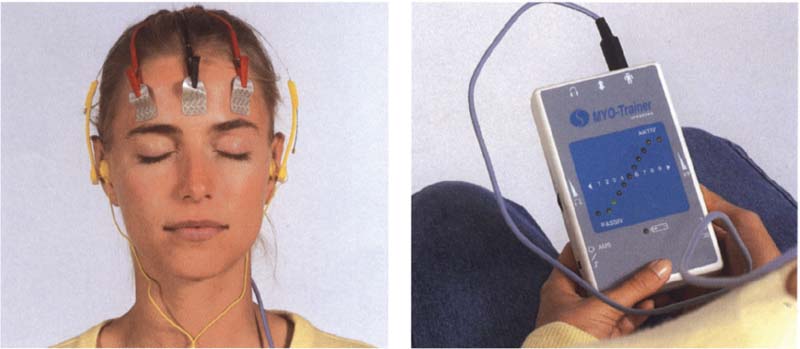
805 Muscle hypertonicity
Left: The electrodes of a biofeedback apparatus are placed on the forehead and temples. If the primary Involvement is with the masseter or the suprahyoid muscles, the electrodes may also be placed there.
Right: The patient monitors the muscle tonus at any given moment either visually by observing an analog scale of light-emitting diodes, or acoustically by listening to a frequency modulated tone. Biofeedback cannot eliminate endogenous causes, however.
Manipulative therapy is the essential tool of the physical therapist for treating restrictions in the masticatory system by
• mobilizing the joint capsule
• stretching the muscles, and
• strengthening weak muscles (Friedman and Weisberg 1984, Rocabado 1989. Israel and Syrop 1997).
If constriction of the joint capsule is causing activation of the pain receptors (Type IV, Wyke 1979) within the capsule, mobilization of the capsule may relieve the pain (Kraus 1994). Physical therapy will never provide long-term success unless there is a permanent modification of the patient’s coordination.
Exercises to improve the patient’s general state of physical fitness have a definite beneficial effect on the pain symptoms (Trott and Goss 1978, Minor et al. 1989) because they improve the ability of the system to compensate. Furthermore, specific dynamic exercises can strengthen the muscles, improve function, and reduce pain (Tegelberg and Kopp 1988).
Coordination exercises for the masseter and anterior temporal muscles can also reduce the burden on the joint (Itoh et al. 1997).
806 Reduced muscle strength
Left: Reduced strength in one muscle can upset the mutually antagonistic neuromuscular balance and thereby alter the condylar position. This is especially true of the lateral pterygoid muscle. In the first treatment phase the weak muscle is strengthened by isometric contractions, being performed here for the left muscle.
Right: Dynamic isotonic exercises are performed in the second treatment phase to functionally integrate the strengthened muscle.

807 Disturbance of coordination
Left: There are numerous techniques to improve muscle coordination (Rocabado et al. 1982, Lewit and Simons 1984, Osternig et al. 1987, Cottingham and Maitland 1997). In addition, the patient can perform isotonic exercises independently.
Right: Jaw movement exercises (“jawsercises,” Korn 1994) can not only improve coordination, they can also help stabilize the results of the manipulative treatment. Nonspecific exercises should be avoided, however.

808 Homework
Left: “Homework” assignments can serve to support active physical therapy or isolated symptomatic treatment or to stabilize the results of therapy. One very effective technique in this regard is autotraction. Right Active movements are usually supplemented by warm applications (“hot packs”). This is in contrast to the treatment for pain, which calls for application of cold.
Occlusal Splints
By the term “occlusal splint” or “occlusal device” is meant a removable artificial occlusal surface of plastic or metal that the patient wears temporarily to alter the occlusal contacts and the functional pattern of the mandible. Occlusal splints attempt to create equal contacts of the posterior teeth and to secure the centric or therapeutic mandibular position through maximal intercuspation against the splint.
A primary advantage of the occlusal splint over other types of occlusal treatment is that the occlusion can be altered without making it necessary to then irreversibly modify the patient’s natural dentition. Occlusal splints have been appropriately called “spectacles for the teeth” (Stachniss 1984). Early references to the use of occlusal devices for the purpose of relaxing the muscles were made by Goodwillie (1881), Ritter (1884) and Karolyi (1901).
Occlusal splints can be effectively used for the following purposes (Crispin et al. 1978, Clark et al. 1979, Manns et al. 1981, Hamada et al. 1982, Lotzmann 1983, Lundh et al. 1985, Okeson 1987):
• improving neuromuscular coordination
• treatment of myogenic pain
• improving function of the temporomandibular joint
• treatment of pain arising from the joints
• increasing the vertical dimension
• securing a definite mandibular position
• altering the pattern of mandibular movement
• testing the planned occlusal scheme In centric and eccentric positions
• splinting of loose teeth
• distributing the load in bruxism
• clarifying occlusal etiological factors while making a differential diagnosis.
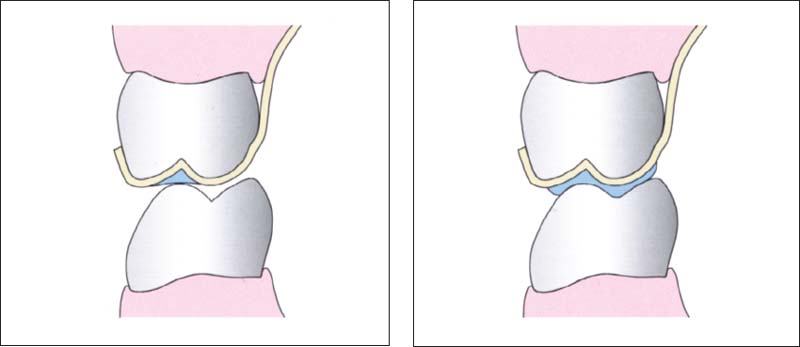
809 Principles of splint design in the posterior region
Left: In the posterior region the occlusal splint is made flat or with only shallow indentations. This design is preferred for the following: relaxation splints, decompression splints, and in some cases repositioning splints.
Right: Distinct imprints of the opposing cusps help to secure the mandibular position. This is the preferred form for stabilization splints and, in some cases, for repositioning splints.
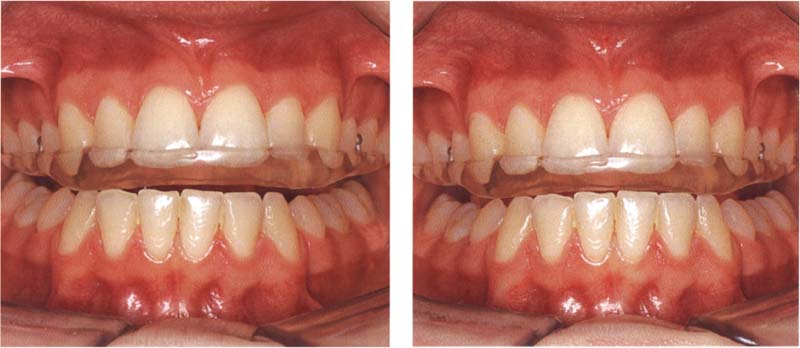
810 Dynamic occlusion
Left: It is preferred that occlusal splints provide anterior, or at least canine, guidance although they may incorporate other eccentric occlusal schemes. Here canine guidance causes vertical disocclusion of all the other teeth during lateral jaw movemiment.
Right: The anterior guiding surfaces of the splint are shaped so that all posterior teeth are out of contact in the protrusive movement also.
In evaluating the therapeutic effects one must consider that occlusal splints not only affect the occlusion, but also suppress proprioception by splinting the teeth together. Furthermore, parafunctional activities triggered by the initial insertion of the splint can temporarily switch off the actual traumatic parafunctions and give the false impression of a successful occlusal treatment.
Occlusal splints can be placed over either the upper or lower dental arches. Their placement depends upon where areas of lost support must be restored and whether the patient’s anterior guidance should be taken over or modified by the appliance. For example, the splint is made for the maxillary arch if the inclination of the anterior or canine guidance is uneven or needs to be made steeper.
An occlusal splint is effective only if the patient’s neuromuscular system can tolerate its presence and the occlusal changes it brings about. If, on the other hand, an occlusal device causes, supports, or intensifies excessive or persistent parafunctional contacts, the success of the treatment will be endangered. This makes it imperative to observe the following rules when inserting an occlusal splint:
• Occlusal splints must have adequate retention and a precise passive fit.
• Their form should be as thin and “periodontium friendly” as possible without jeopardizing stability and occlusal function.
• In accordance with a cause-oriented therapy, occlusal devices should simulate only those occlusal relationships that can be reproduced essentially unchanged in the final restorations.
• Preliminary occlusal splint therapy that is not diagnosis-specific, that is uncontrolled or is of excessively long duration can bring about pathological and to some extent irreversible changes in the masticatory system, such as caries progression, periodontal disease, tooth movement, and alterations in joint morphology.

811 Occlusal splint for a posteriorly shortened arch
Left: A removable partial denture with inadequate occlusion can be converted into an effective occlusal treatment device by adding acrylic to correct the occlusion. The old plastic teeth are not replaced by new ones until a comfortable mandibular position has been reached.
Right: When correctly formed, an occlusal splint can serve as a suitable temporary prosthesis for a posteriorly shortened dental arch (“free-end saddle”).

812 Occlusal splints for cases with visible gaps
For greater patient acceptance, occlusal devices should incorporate plastic teeth, at least where teeth are missing in the appearance zone. from the collection of H Gloerfeld
If the primary cause of the craniomandibular functional disturbance lies in a psychological illness, any form of treatment that is not specifically directed toward the psychological cause can lead to conversion of the psychic illness into physical symptoms (beware: “occlusion neurosis”). The clinician can sometimes satisfy a patient’s built-in need for occlusal therapy by merely inserting an occlusal splint. A placebo effect may be achieved even if the occlusion of the splint is inadequate (Greene and Laskin 1972).
The multitude of occlusal devices described in the literature can be classified according to their indications as follows (Lotzmann 1999):
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


